Abstract
Purpose
To evaluate, whether the regional variability of tonsil surgery in terms of the 16 Federal States of Germany was mirrored by a comparable variability of bleeding complications in male and female patients.
Methods
A longitudinal population-based inpatient cohort study was performed including all patients who had undergone tonsil surgery between 2005 and 2018. The database was provided by the Federal Statistical Office of Germany and included all inpatient cases after tonsillectomy (with or without adenoidectomy), tonsillotomy, abscess-tonsillectomy and secondary tonsillectomy. The population was stratified by region (16 Federal States) and gender. Operation rates were calculated in relation to the end-year population number of each region. Bleeding percentages were calculated for each calendar year and region as the number of procedures to achieve hemostasis divided by the total number of operations.
Results
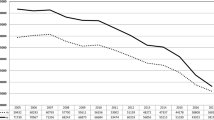
The surgical rates varied significantly between the 16 Federal States in male, female and all patients (p = 0.001). Revision surgery to achieve hemostasis was predominantly performed in male patients (5.2–11.4% male vs. 3.7–7.6% female patients). Bleeding percentages did not differ significantly from national values in male and female patients in 5 Federal States, but were significantly higher than the national average in 3 Federal States and significantly lower in 7 Federal States for both genders (p < 0.05), while in 1 Federal State it was significantly lower only for the male patients. Pearson’s correlation coefficient for surgical and bleeding rates was positive and statistically significant (p < 0.05) for all Federal States, except for two. This phenomenon was emphasized by female gender.
Conclusions
Gender had an impact not only on surgical rates but also on bleeding percentages and this was independent from the decrease in the total number of operations. Surprisingly, there was a clear correlation between the rates of both variables in the majority of the Federal States of Germany. It needs further studies to clarify, why a higher prevalence of surgical practice, thus surgical experience, was not followed by lower bleeding complications.


Similar content being viewed by others
Abbreviations
- SLH:
-
Schleswig–Holstein
- HH:
-
Hamburg
- NS:
-
Niedersachsen
- BR:
-
Bremen
- NRW:
-
Nordrhein–Westfalen
- HE:
-
Hessen
- RLP:
-
Rheinland–Pfalz
- BW:
-
Baden–Württemberg
- BA:
-
Bayern
- SAA:
-
Saarland
- BER:
-
Berlin
- BRA:
-
Brandenburg
- MV:
-
Mecklenburg–Vorpommern
- SAC:
-
Sachsen
- SAN:
-
Sachsen–Anhalt
- TH:
-
Thüringen
- TE:
-
Tonsillectomy
- ATE:
-
Tonsillectomy with adenoidectomy
- TT:
-
Tonsillotomy
References
Appleby J, Raleigh V, Frosini F et al (2011) Variations in health care. The good, the bad and the inexplicable. London
Elinder K, Hessen Soderman AC, Stalfors J et al (2016) Factors influencing morbidity after paediatric tonsillectomy: a study of 18,712 patients in the National Tonsil Surgery Register in Sweden. Eur Arch Otorhinolaryngol 273:2249–2256
Faktencheck-Gesundheit.De/De/Publikationen/Publikation/Did/Faktencheck-Gesundheit-Gaumenmandeln. 2013. Accessed 20 Feb 2020
Fedeli U, Marchesan M, Avossa F et al (2009) Variability of adenoidectomy/tonsillectomy rates among children of the Veneto Region. Italy BMC Health Serv Res 9:25
Glover JA (1938) The incidence of tonsillectomy in school children: (section of epidemiology and state medicine). Proc R Soc Med 31:1219–1236
Hinton-Bayre AD, Noonan K, Ling S et al (2017) Experience is more important than technology inpaediatric post-tonsillectomy bleeding. J Laryngol Otol 131:35–40
Hsueh WY, Hsu WC, Ko JY et al (2018) Population-based survey of inpatient pediatric tonsillectomy and postoperative hemorrhage in Taiwan, 1997–2012. Int J Pediatr Otorhinolaryngol 108:55–62
Lechner M, Chandrasekharan D, Vithlani R et al (2017) Evaluation of a newly introduced tonsillectomy operation record for the analysis of a regional post-tonsilectomy bleed data: a quality improvement project at the London North West Healthcare NHS Trust. BMJ Open Quality 6:e000055
Liu JH, Anderson KE, Willging JP et al (2001) Posttonsillectomy hemorrhage: what is it and what should be recorded? Arch Otolaryngol Head Neck Surg 127:1271–1275
Lowe D, Van Der Meulen J, Audit NPT (2004) Tonsillectomy technique as a risk factor for postoperative hemorrhage. Lancet 364:642–643
Lowe D, Van Der Meulen J, Cromwell D et al (2007) Key messages from the national prospective tonsillectomy audit. Laryngoscope 117:717–724
Mitchell RB, Archer SM, Ishman SL et al (2019) Clinical practice guideline: tonsillectomy in children (update). Otolaryngol Head Neck Surg 160:S1–S42
Ostvoll E, Sunnergren O, Stalfors J (2018) Increasing readmission rates for hemorrhage after tonsil surgery: a longitudinal (26 years) national study. Otolaryngol Head Neck Surg 158:167–176
Sarny S, Ossimitz G, Habermann W et al (2012) The Austrian tonsil study 2010–part 1: statistical overview. Laryngorhinootologie 91:16–21
Sarny S, Ossimitz G, Habermann W et al (2013) Austrian tonsil study part 3: surgical technique and postoperative haemorrhage after tonsillectomy. Laryngorhinootologie 92:92–96
Soderman AC, Odhagen E, Ericsson E et al (2015) Post-tonsillectomy haemorrhage rates are related to technique for dissection and for haemostasis. An analysis of 15734 patients in the National Tonsil Surgery Register in Sweden. Clin Otolaryngol 40:248–254
Spektor Z, Saint-Victor S, Kay DJ et al (2016) Risk factors for pediatric post-tonsillectomy hemorrhage. Int J Pediatr Otorhinolaryngol 84:151–155
Stalfors J, Ericsson E, Hemlin C et al (2013) Annual report 2013. The National Tonsil Surrey Regisetr in Sweden https://www.registercentrum.blob.core.windows.net/orl/r/-rsrapport-2013-Tonsilloperationsregistrets-engelska-version-ByOVNca.pdf. Accessed 19 Apr 2020
Suleman M, Clark MP, Goldacre M et al (2010) Exploring the variation in paediatric tonsillectomy rates between English regions: a 5-year NHS and independent sector data analysis. Clin Otolaryngol 35:111–117
Van Den Akker EH, Hoes AW, Burton MJ et al (2004) Large international differences in (adeno)tonsillectomy rates. Clin Otolaryngol Allied Sci 29:161–164
Wei JL, Beatty CW, Gustafson RO (2000) Evaluation of posttonsillectomy hemorrhage and risk factors. Otolaryngol Head Neck Surg 123:229–235
Wennberg J, Gittelsohn A (1973) Small area variations in health care delivery. Science 182:1102–1108
Windfuhr JP (2013) Faults and failure of tonsil surgery and other standard procedures in otorhinolaryngology. Laryngorhinootologie 92(Suppl 1):S33–72
Windfuhr JP (2016) Indications for tonsillectomy stratified by the level of evidence. GMS Curr Top Otorhinolaryngol Head Neck Surg 15:Doc09
Windfuhr JP (2013) Serious complications following tonsillectomy: how frequent are they really? ORL J Otorhinolaryngol Relat Spec 75:166–173
Windfuhr JP, Chen YS (2019) Do changing trends in tonsil surgery affect hemorrhage rates? A longitudinal study covering 1,452,637 procedures. Eur Arch Otorhinolaryngol 276:2585–2593
Windfuhr JP, Chen YS (2019) Tonsil surgery in the federal states of Germany: similarities and differences. HNO
Windfuhr JP, Wienke A, Chen YS (2009) Electrosurgery as a risk factor for secondary post-tonsillectomy hemorrhage. Eur Arch Otorhinolaryngol 266:111–116
https://www.destatis.de. Accessed 26 Nov 2018
https://www.gba.ge. Accessed 28 Nov 2018
https://www.gbe-bund.de. Accessed 01 Oct 2020
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. According to the policy of the IRB responsible for the authors, this study was exempt from ethical approval, because it was a secondary analysis of a publicly available dataset with anonymous data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Windfuhr, J.P., Alizoti, P. & Hendricks, C. Regional variability of hemorrhage following tonsil surgery in 1,520,234 cases. Eur Arch Otorhinolaryngol 277, 3169–3177 (2020). https://doi.org/10.1007/s00405-020-06080-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06080-x