Abstract
Purpose
Several murine models have been established to mimic human eosinophilic chronic rhinosinusitis (ECRS). However, in most of these models, ECRS was induced using ovalbumin, which does not cause sinusitis in humans. Thus, we aimed to develop a more clinically relevant murine model of ECRS using multiple airborne allergens. We also investigated the effects of exposure duration of the allergens on ECRS development.
Methods
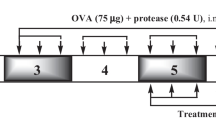
C57BL/6 mice were intranasally administered multiple airborne allergens (house dust mite, Aspergillus fumigatus, Alternaria alternata, and protease from Staphylococcus aureus) three times weekly for 4, 8, 12, and 16 consecutive weeks. Histopathological changes, the levels of cytokines and chemokines in the nasal lavage fluid, and immune cells of the blood and spleen were analyzed.
Results
The mice administered multiple allergens showed significantly increased eosinophil infiltration, epithelial thickening and disruption, and subepithelial collagen deposition from 8 weeks compared to the control group. Goblet cell hyperplasia, polyp-like lesions, and blood eosinophils, as well as the levels of interleukin-5 and eotaxin in the nasal lavage fluid were considerably increased in the ECRS group from 12 weeks compared to those of controls. Instillation of allergens for 16 weeks exacerbated the eosinophil infiltration and eotaxin increase in the nasal lavage fluid.
Conclusions
We successfully established a new murine model of ECRS using more clinically relevant multiple airborne allergens. Prolonged exposure to airborne allergens for 12 weeks or more, corresponding to the definition of human ECRS, strongly induced eosinophil infiltration as well as epithelial remodeling.





Similar content being viewed by others
References
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, Cohen N, Cervin A, Douglas R, Gevaert P, Georgalas C, Goossens H, Harvey R, Hellings P, Hopkins C, Jones N, Joos G, Kalogjera L, Kern B, Kowalski M, Price D, Riechelmann H, Schlosser R, Senior B, Thomas M, Toskala E, Voegels R, de Wang Y, Wormald PJ (2012) EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50(1):1–12. https://doi.org/10.4193/Rhino50E2
Halawi AM, Smith SS, Chandra RK (2013) Chronic rhinosinusitis: epidemiology and cost. Allergy Asthma Proc 34(4):328–334. https://doi.org/10.2500/aap.2013.34.3675
Wang X, Zhang N, Bo M, Holtappels G, Zheng M, Lou H, Wang H, Zhang L, Bachert C (2016) Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: a multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol 138(5):1344–1353. https://doi.org/10.1016/j.jaci.2016.05.041
London NR Jr, Tharakan A, Ramanathan M Jr (2016) The role of innate immunity and aeroallergens in chronic rhinosinusitis. Adv Otorhinolaryngol 79:69–77. https://doi.org/10.1159/000445132
Jarvis D, Newson R, Lotvall J, Hastan D, Tomassen P, Keil T, Gjomarkaj M, Forsberg B, Gunnbjornsdottir M, Minov J, Brozek G, Dahlen SE, Toskala E, Kowalski ML, Olze H, Howarth P, Kramer U, Baelum J, Loureiro C, Kasper L, Bousquet PJ, Bousquet J, Bachert C, Fokkens W, Burney P (2012) Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy 67(1):91–98. https://doi.org/10.1111/j.1398-9995.2011.02709.x
Ishitoya J, Sakuma Y, Tsukuda M (2010) Eosinophilic chronic rhinosinusitis in Japan. Allergol Int 59(3):239–245. https://doi.org/10.2332/allergolint.10-RAI-0231
Zhang N, Van Zele T, Perez-Novo C, Van Bruaene N, Holtappels G, DeRuyck N, Van Cauwenberge P, Bachert C (2008) Different types of T-effector cells orchestrate mucosal inflammation in chronic sinus disease. J Allergy Clin Immunol 122(5):961–968. https://doi.org/10.1016/j.jaci.2008.07.008
Kato A (2015) Immunopathology of chronic rhinosinusitis. Allergol Int 64(2):121–130. https://doi.org/10.1016/j.alit.2014.12.006
Schleimer RP (2017) Immunopathogenesis of chronic rhinosinusitis and nasal polyposis. Annu Rev Pathol 12:331–357. https://doi.org/10.1146/annurev-pathol-052016-100401
Kim SJ, Lee KH, Kim SW, Cho JS, Park YK, Shin SY (2013) Changes in histological features of nasal polyps in a Korean population over a 17-year period. Otolaryngol Head Neck Surg 149(3):431–437. https://doi.org/10.1177/0194599813495363
Katotomichelakis M, Tantilipikorn P, Holtappels G, De Ruyck N, Feng L, Van Zele T, Muangsomboon S, Jareonchasri P, Bunnag C, Danielides V, Cuvelier CA, Hellings PW, Bachert C, Zhang N (2013) Inflammatory patterns in upper airway disease in the same geographical area may change over time. Am J Rhinol Allergy 27(5):354–360. https://doi.org/10.2500/ajra.2013.27.3922
Wang H, Lu X, Cao PP, Chu Y, Long XB, Zhang XH, You XJ, Cui YH, Liu Z (2008) Histological and immunological observations of bacterial and allergic chronic rhinosinusitis in the mouse. Am J Rhinol 22(4):343–348. https://doi.org/10.2500/ajr.2008.22.3184
Kim DW, Khalmuratova R, Hur DG, Jeon SY, Kim SW, Shin HW, Lee CH, Rhee CS (2011) Staphylococcus aureus enterotoxin B contributes to induction of nasal polypoid lesions in an allergic rhinosinusitis murine model. Am J Rhinol Allergy 25(6):e255–e261. https://doi.org/10.2500/ajra.2011.25.3727
Kim HC, Lim JY, Kim S, Kim JH, Jang YJ (2017) Development of a mouse model of eosinophilic chronic rhinosinusitis with nasal polyp by nasal instillation of an Aspergillus protease and ovalbumin. Eur Arch Otorhinolaryngol 274(11):3899–3906. https://doi.org/10.1007/s00405-017-4717-2
Nials AT, Uddin S (2008) Mouse models of allergic asthma: acute and chronic allergen challenge. Dis Model Mech 1(4–5):213–220. https://doi.org/10.1242/dmm.000323
Kim JH, Yi JS, Gong CH, Jang YJ (2014) Development of Aspergillus protease with ovalbumin-induced allergic chronic rhinosinusitis model in the mouse. Am J Rhinol Allergy 28(6):465–470. https://doi.org/10.2500/ajra.2014.28.4100
Lindsay R, Slaughter T, Britton-Webb J, Mog SR, Conran R, Tadros M, Earl N, Fox D, Roberts J, Bolger WE (2006) Development of a murine model of chronic rhinosinusitis. Otolaryngol Head Neck Surg 134(5):724–730. https://doi.org/10.1016/j.otohns.2005.11.048 (discussion 731–732)
Park SC, Hwang CS, Chung HJ, Purev M, Al Sharhan SS, Cho HJ, Yoon JH, Kim CH (2019) Geographic and demographic variations of inhalant allergen sensitization in Koreans and non-Koreans. Allergol Int 68(1):68–76. https://doi.org/10.1016/j.alit.2018.07.005
Lam K, Schleimer R, Kern RC (2015) The etiology and pathogenesis of chronic rhinosinusitis: a review of current hypotheses. Curr Allergy Asthma Rep 15(7):41. https://doi.org/10.1007/s11882-015-0540-2
Black PN, Udy AA, Brodie SM (2000) Sensitivity to fungal allergens is a risk factor for life-threatening asthma. Allergy 55(5):501–504
deShazo RD, Swain RE (1995) Diagnostic criteria for allergic fungal sinusitis. J Allergy Clin Immunol 96(1):24–35
Shin SH, Ponikau JU, Sherris DA, Congdon D, Frigas E, Homburger HA, Swanson MC, Gleich GJ, Kita H (2004) Chronic rhinosinusitis: an enhanced immune response to ubiquitous airborne fungi. J Allergy Clin Immunol 114(6):1369–1375. https://doi.org/10.1016/j.jaci.2004.08.012
Bartemes KR, Iijima K, Kobayashi T, Kephart GM, McKenzie AN, Kita H (2012) IL-33-responsive lineage-CD25+ CD44(hi) lymphoid cells mediate innate type 2 immunity and allergic inflammation in the lungs. J Immunol 188(3):1503–1513. https://doi.org/10.4049/jimmunol.1102832
Sachse F, Becker K, von Eiff C, Metze D, Rudack C (2010) Staphylococcus aureus invades the epithelium in nasal polyposis and induces IL-6 in nasal epithelial cells in vitro. Allergy 65(11):1430–1437. https://doi.org/10.1111/j.1398-9995.2010.02381.x
Khalmuratova R, Lee M, Kim DW, Park JW, Shin HW (2016) Induction of nasal polyps using house dust mite and Staphylococcal enterotoxin B in C57BL/6 mice. Allergol Immunopathol (Madr) 44(1):66–75. https://doi.org/10.1016/j.aller.2015.04.004
Jacob A, Chole RA (2006) Survey anatomy of the paranasal sinuses in the normal mouse. Laryngoscope 116(4):558–563. https://doi.org/10.1097/01.MLG.0000202085.23454.2F
Tajudeen BA, Ganti A, Kuhar HN, Mahdavinia M, Heilingoetter A, Gattuso P, Ghai R, Batra PS (2019) The presence of eosinophil aggregates correlates with increased postoperative prednisone requirement. Laryngoscope 129(4):794–799. https://doi.org/10.1002/lary.27693
Van Bruaene N, Derycke L, Perez-Novo CA, Gevaert P, Holtappels G, De Ruyck N, Cuvelier C, Van Cauwenberge P, Bachert C (2009) TGF-beta signaling and collagen deposition in chronic rhinosinusitis. J Allergy Clin Immunol 124(2):253–259. https://doi.org/10.1016/j.jaci.2009.04.013 (259 e251–252)
Cho SH, Oh SY, Zhu Z, Lee J, Lane AP (2012) Spontaneous eosinophilic nasal inflammation in a genetically-mutant mouse: comparative study with an allergic inflammation model. PLoS One 7(4):e35114. https://doi.org/10.1371/journal.pone.0035114
Kouzaki H, Matsumoto K, Kikuoka H, Kato T, Tojima I, Shimizu S, Kita H, Shimizu T (2017) endogenous protease inhibitors in airway epithelial cells contribute to eosinophilic chronic rhinosinusitis. Am J Respir Crit Care Med 195(6):737–747. https://doi.org/10.1164/rccm.201603-0529OC
Kim DW, Eun KM, Jin HR, Cho SH, Kim DK (2016) Prolonged allergen exposure is associated with increased thymic stromal lymphopoietin expression and Th2-skewing in mouse models of chronic rhinosinusitis. Laryngoscope 126(8):E265–E272. https://doi.org/10.1002/lary.26004
Takai T, Kato T, Sakata Y, Yasueda H, Izuhara K, Okumura K, Ogawa H (2005) Recombinant Der p 1 and Der f 1 exhibit cysteine protease activity but no serine protease activity. Biochem Biophys Res Commun 328(4):944–952
Kauffman HF, Tomee JF, van de Riet MA, Timmerman AJ, Borger P (2000) Protease-dependent activation of epithelial cells by fungal allergens leads to morphologic changes and cytokine production. J Allergy Clin Immunol 105(6 Pt 1):1185–1193
Snelgrove RJ, Gregory LG, Peiro T, Akthar S, Campbell GA, Walker SA, Lloyd CM (2014) Alternaria-derived serine protease activity drives IL-33-mediated asthma exacerbations. J Allergy Clin Immunol 134(3):583–592e586. https://doi.org/10.1016/j.jaci.2014.02.002
Dubin G (2002) Extracellular proteases of Staphylococcus spp. Biol Chem 383(7–8):1075–1086
Takai T, Ikeda S (2011) Barrier dysfunction caused by environmental proteases in the pathogenesis of allergic diseases. Allergol Int 60(1):25–35. https://doi.org/10.2332/allergolint.10-RAI-0273
Balenga NA, Klichinsky M, Xie Z, Chan EC, Zhao M, Jude J, Laviolette M, Panettieri RA Jr, Druey KM (2015) A fungal protease allergen provokes airway hyper-responsiveness in asthma. Nat Commun 6:6763. https://doi.org/10.1038/ncomms7763
Brescia G, Alessandrini L, Zanotti C, Parrino D, Tealdo G, Torsello M, Zybine V, Giacomelli L, Barion U, Marioni G (2019) Histopathological and hematological changes in recurrent nasal polyposis. Int Forum Allergy Rhinol. https://doi.org/10.1002/alr.22314
Snidvongs K, Lam M, Sacks R, Earls P, Kalish L, Phillips PS, Pratt E, Harvey RJ (2012) Structured histopathology profiling of chronic rhinosinusitis in routine practice. Int Forum Allergy Rhinol 2(5):376–385. https://doi.org/10.1002/alr.21032
Tokunaga T, Sakashita M, Haruna T, Asaka D, Takeno S, Ikeda H, Nakayama T, Seki N, Ito S, Murata J, Sakuma Y, Yoshida N, Terada T, Morikura I, Sakaida H, Kondo K, Teraguchi K, Okano M, Otori N, Yoshikawa M, Hirakawa K, Haruna S, Himi T, Ikeda K, Ishitoya J, Iino Y, Kawata R, Kawauchi H, Kobayashi M, Yamasoba T, Miwa T, Urashima M, Tamari M, Noguchi E, Ninomiya T, Imoto Y, Morikawa T, Tomita K, Takabayashi T, Fujieda S (2015) Novel scoring system and algorithm for classifying chronic rhinosinusitis: the JESREC Study. Allergy 70(8):995–1003. https://doi.org/10.1111/all.12644
Brescia G, Sfriso P, Marioni G (2019) Role of blood inflammatory cells in chronic rhinosinusitis with nasal polyps. Acta Otolaryngol 139(1):48–51. https://doi.org/10.1080/00016489.2018.1538567
Tomassen P, Vandeplas G, Van Zele T, Cardell LO, Arebro J, Olze H, Forster-Ruhrmann U, Kowalski ML, Olszewska-Ziaber A, Holtappels G, De Ruyck N, Wang X, Van Drunen C, Mullol J, Hellings P, Hox V, Toskala E, Scadding G, Lund V, Zhang L, Fokkens W, Bachert C (2016) Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clin Immunol 137(5):1449–1456e1444. https://doi.org/10.1016/j.jaci.2015.12.1324
Yao T, Kojima Y, Koyanagi A, Yokoi H, Saito T, Kawano K, Furukawa M, Kusunoki T, Ikeda K (2009) Eotaxin-1, -2, and -3 immunoreactivity and protein concentration in the nasal polyps of eosinophilic chronic rhinosinusitis patients. Laryngoscope 119(6):1053–1059. https://doi.org/10.1002/lary.20191
Tharakan A, Dobzanski A, London NR Jr, Khalil SM, Surya N, Lane AP, Ramanathan M Jr (2018) Characterization of a novel, papain-inducible murine model of eosinophilic rhinosinusitis. Int Forum Allergy Rhinol 8(4):513–521. https://doi.org/10.1002/alr.22072
Jacob A, Faddis BT, Chole RA (2001) Chronic bacterial rhinosinusitis: description of a mouse model. Arch Otolaryngol Head Neck Surg 127(6):657–664
Cao PP, Li HB, Wang BF, Wang SB, You XJ, Cui YH, Wang DY, Desrosiers M, Liu Z (2009) Distinct immunopathologic characteristics of various types of chronic rhinosinusitis in adult Chinese. J Allergy Clin Immunol 124(3):478–484. https://doi.org/10.1016/j.jaci.2009.05.017 (484.e471–472)
Saitoh T, Kusunoki T, Yao T, Kawano K, Kojima Y, Miyahara K, Onoda J, Yokoi H, Ikeda K (2010) Role of interleukin-17A in the eosinophil accumulation and mucosal remodeling in chronic rhinosinusitis with nasal polyps associated with asthma. Int Arch Allergy Immunol 151(1):8–16. https://doi.org/10.1159/000232566
Brescia G, Zanotti C, Parrino D, Barion U, Marioni G (2018) Nasal polyposis pathophysiology: endotype and phenotype open issues. Am J Otolaryngol 39(4):441–444. https://doi.org/10.1016/j.amjoto.2018.03.020
Funding
This study was supported by the Bio & Medical Technology Development Program of the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (MSIP) (2016M3A9D5A01952414), and the NRF grant funded by the Korean Government (MSIP) (2016R1A5A2008630). This research was also supported by the NRF Grant funded by the Korean Government (Ministry of Science and ICT) (NRF-2018R1C1B6007431).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in this study involving animals were approved by the Ethics Committee and Institutional Animal Care and Use Committee of Yonsei University Health System (2017-0094), and the study was conducted according to international guidelines (ARRIVE) on animal experiments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
405_2019_5465_MOESM1_ESM.tif
Supplementary material 1 (TIFF 17995 kb) Supplementary Fig. 1 Comparison of eosinophil infiltration between nine different areas of the nasal mucosa. Sirius red stain showing increased eosinophil infiltration in the ECRS group compared to that of controls in all areas measured, especially along the nasal septum (indicated areas 1, 2, 3, and 4), followed by the superior maxillary turbinate (indicated areas 5 and 6) and inferior maxillary turbinate (indicated areas 7 and 8). Data are expressed as means ± SD. * p < 0.05, ** p < 0.01, *** p < 0.001 between the control and ECRS groups. ECRS, eosinophilic chronic rhinosinusitis; HPF, high power fields
405_2019_5465_MOESM2_ESM.tif
Supplementary material 2 (TIFF 17481 kb) Supplementary Fig. 2 Comparison of goblet cell hyperplasia between nine different areas of the nasal mucosa. Periodic acid-Schiff stain showing increased goblet cell hyperplasia in the ECRS group compared to that of controls in all areas measured, especially in the nasal septum (indicated areas 2, 3, and 4) and superior maxillary turbinate (indicated area 6). Data are expressed as means ± SD. * p < 0.05 between the control and ECRS groups. ECRS, eosinophilic chronic rhinosinusitis; HPF, high power fields
405_2019_5465_MOESM3_ESM.tif
Supplementary material 3 (TIFF 13680 kb) Supplementary Fig. 3 Representative photomicrographs of epithelium disruption and formation of polyp-like lesions. a Hematoxylin and eosin-stained sections showing epithelial disruption only in the ECRS group from 8 weeks. b Sirius red stained section showing polyp-like lesions, defined as elevated mucosal lesions with eosinophilic infiltration and/or microcavity formation, which were detected only in the ECRS group from 12 weeks. (both panels: original magnification, ×400; magnified image of the ×40 figure on the left side; scale bar, 50 μm)
405_2019_5465_MOESM4_ESM.tif
Supplementary material 4 (TIFF 16476 kb) Supplementary Fig. 4 Flow cytometry gating strategy for analysis of neutrophils and eosinophils in the blood. Eosinophils (CD11c-, CD11b+, Ly-6G-, Siglec-F+) and neutrophils (CD11c-, CD11b+, Ly-6G+, Siglec-F-) were identified as shown
405_2019_5465_MOESM5_ESM.tif
Supplementary material 5 (TIFF 19800 kb) Supplementary Fig. 5 Flow cytometry gating strategy and immune cell analysis in the spleen at 16 weeks. a Flow cytometry gating scheme for analysis of immune cells to identify B cells (CD45+,CD11c-, MHC II+, CD19+), T cells (CD45+,CD11c-, MHC II-, CD3e+), dendritic cells (CD45+,CD11c+, MHC II+), and macrophages (CD45+,CD11c+, F4/80+, CD64+). b At 16 weeks, the percentage of spleen eosinophils among CD45+ cells was significantly elevated in the ECRS group compared to that of controls. *** p < 0.001 between the control and ECRS groups. ECRS, eosinophilic chronic rhinosinusitis
Rights and permissions
About this article
Cite this article
Park, S.C., Kim, S.I., Hwang, C.S. et al. Multiple airborne allergen-induced eosinophilic chronic rhinosinusitis murine model. Eur Arch Otorhinolaryngol 276, 2273–2282 (2019). https://doi.org/10.1007/s00405-019-05465-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05465-x