Abstract
Purpose
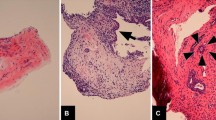
The thesis that cholesteatoma evolves from a retraction pocket is widely accepted today. Yet, its prime etiology, the question of what triggers the invagination of healthy skin, still remains unclear despite centuries of investigations into the origin of cholesteatoma. A new idea interprets the horizontal migration of skin into the middle ear cavities as a self-healing process, curing an underlying inflammation in the tympanic cavity, through the overgrowth and contact with immunologically active tissue.
Methods
A retrospective analysis of the interrelation of retraction pockets and underlying granulation tissue was conducted in 209 second-look cholesteatoma surgeries over the last decade.
Results
A stable tympanic membrane over aerated, healthy middle ear mucosa was found in 71.3% of cases. In 11%, small retractions with air in other parts of the middle ear cleft (epitympanic, sinus or anterior mesotympanum) were described. In 6.2%, granulations under a retraction were found. Only 3.8% of the reports revealed air behind a retraction or did not provide enough information on the mucosa situation behind the drum membrane.
Conclusions
A new hypothesis interprets the origin of a retraction pocket—the precursor of a cholesteatoma—as a natural attempt by the body to cure an underlying inflammation in a cavity. Analogous phenomena exist, e.g. the migration of the omentum towards a local inflammation in the abdomen. This idea, which is supported by the findings in our 209 second-look surgeries, is the first explanation of the origin of retraction pockets that is compatible with the various characteristics of original or recurrent cholesteatoma. A prophylaxis against a recurrent cholesteatoma might be attained by securing free drainage of the mucosa into the tubal orifice with the use of thin silicone foils in an attempt to prevent any granulation in the middle ear cleft, similar to the principles of modern rhinosinusoidal surgery with its emphasis on unblocked mucosa clearance. This allows gas production in the healed middle ear mucosa to recover, reducing the risk of a recurrent retraction.
Similar content being viewed by others
References
Kuo CL (2014) Etiopathogenesis of acquired cholesteatoma: prominent theories and recent advances in biomolecular research. Laryngoscope 125:234–240
Soldati D, Mudry A (2001) Knowledge about cholesteatoma, from the first description to the modern histopathology. Otol Neurotol 22:723–730
Jackler RK, Santa Maria PL, Varsak YK, Nguyen A, Blevins NH (2015) A new theory on the pathogenesis of acquired cholesteatoma: mucosal traction. Laryngoscope 125(Suppl. 4):1–14
Tos M (1981) Upon the relationship between secretory otitis in childhood and chronic otitis and its sequelae in adults. J Laryngol Otol 95:1011–1022
Habermann J (1898) Zur Entstehung des Cholesteatoms des Mittelohres. Arch Ohrenheilkunde 27:42–50
Gruber J (1888) Das Cholesteatom (Perlgeschwulst). Lehrbuch der Ohrenheilkunde. Berlin. C. Geralds Sohn
Michaels L (1986) An epidermoid formation in the developing middle ear: possible source of cholesteatoma. J Otolaryngol 15:169–174
Escher F (1979) Die Therapie des Mittelohrcholesteatoms. HNO 27:145–149
Steinbach E, Pusalkar A, Heumann H (1988) Cholesteatoma—pathology and treatment. Adv Oto-Rhino-Laryngol 39:94–106
Karmody CS, Northrop C (2011) The pathogenesis of acquired cholesteatoma of the human middle ear: support for the migration hypothesis. Otol Neurotol 33:42–47
Sudhoff H, Tos M (2007) Pathogenesis of sinus cholesteatoma. Eur Arch Oto-Rhino-Laryngol 264:137–143
Deong KK, Prepageran N, Raman R (2006) Epithelial migration of the postmyringoplasty tympanic membrane. Otol Neurotol 27:855–858
Tos M (1988) Incidence, etiology and pathogenesis of cholesteatoma in children. Adv Oto-Rhino-Laryngol 40:110–117
Wayoff M, Charachon R, Roulleau P, Lacher G, Deguine C (1987) Surgical treatment of middle ear cholesteatoma. In: Advances in Oto-Rhino-Laryngology, vol 36. Karger, Basel
Tos M, Lau T (1988) Attic cholesteatoma. Recurrence rate related to observation time. Am J Otol 9:456–464
Louw L (2010) Acquired cholesteatoma pathogenesis: stepwise explanations. J Laryngol Otol 124:587–593
Hüttenbrink KB (1984) Die chronische Otitis media. In: Nauman H, Helms J, Herberhold C, Kastenbauer E (eds) Oto Rhino Laryngologie in Klinik und Praxis, Band 1 Ohr, G. Thieme, Stuttgart, pp 601–632
Bezold F (1891) Über das Cholesteatom des Mittelohres. Z Ohrenheilkunde. 21:252–271
Marchioni D, Alicandri-Ciufelli M, Molteni G, Artioli FL, Genovese E, Presutti L (2010) Selective epitympanic dysventilation syndrome. Laryngoscope 120:1028–1033
Morimitsu T, Nagay T, Nagay M, Ide M, Makino K, Tono T (1989) Long term results of anterior tympanotomy for cholesteatoma. In: Tos M, Thomssen J, Peitersen E (eds) Cholesteatoma and mastoid surgery. Kugler, Amsterdam, pp 875–880
Meyerhoff WL, Wright CG, Gerken GM (1990) Effects of middle ear ventilation on cholesteatoma development in experimental animals. Acta Otolaryngol 110:279–285
Tos M, Stangerup SE, Holm-Jensen S, Sørensen CH (1984) Spontaneous course of secretory otitis and changes of the eardrum. Arch Otolaryngol 110:281–289
Spilsbury K, Ha JF, Semmens JB, Lannigan F (2013) Cholesteatoma in cleft lip and palate: a populations-based follow-up study of children after ventilation tubes. Laryngoscope 123:2024–2029
Heumann A, Steinbach E, Koneberg F (1981) Untersuchung zur Cholesteatomentstehung durch Verschluss der Tube bei Kaninchen. Arch Oto-Rhino-Laryngol 231:813–815
Buckingham RA (1988) Patent eustachian tube in the underaerated middle ear: a paradox. Ann Otol Rhinol Laryngol 97:219–221
Sadé J, Luntz M, Levy D (1995) Middle ear gas composition and middle ear aeration. Ann Otol Rhinol Laryngol 104:369–373
Gaihede M, Dirckx JJ, Jacobsen H, Aernouts J, Sovso M, Tveteras K (2010) Middle ear pressure regulation-complementary active actions of the mastoid and the Eustachian tube. Otol Neurotol 31:603–611
Wullstein HL, Wullstein SR (1980) Cholesteatoma. Etiology, nosology and tympanoplasty. J Otorhinolaryngol 42:313–335
Chole RA, Lim DJ (2015) In reference to a new theory on the pathogenesis of acquired cholesteatoma: mucosal traction. Laryngoscope 126:E129–E130
Kuo CL (2016) Letter to the editor in reference to a new theory on the pathogenesis of acquired cholesteatoma: mucosal traction. Laryngoscope 126:E132
Yeger H, Minaker E, Charles D, Rubin A, Sturgess JM (1988) Abnormalities of cilia in the middle ear in chronic otitis media. Ann Otol 97:180–191
Schwartz M (1984) Die genetischen Faktoren des Mittelohrcholesteatoms. HNO 32:59–60
Ruedi L (1978) Pathogenesis and surgical treatment of the middle ear cholesteatoma. Acta Otolaryngol 361(Suppl):1–45
Beutner D, Helmstaedter V, Stumpf R, Beleites D, Zahnert T, Lüers JC, Hüttenbrink KB (2010) Impact of partial mastoid obliteration on caloric vestibular function in canal wall down mastoidectomy. Otol Neurotol 31:1399–1403
Vercruysse JP, van Dinther JJ, De Foer B, Casselman J, Somers T, Cremers CC, Offeciers E (2016) Long-term results of troublesome CWD cavity reconstruction by mastoid and epitympanic bony obliteration (CWR-BOT) in adults. Otol Neurotol 37:698–703
Kaufmann E, Staemmler M (1956) Lehrbuch der speziellen pathologischen Anatomie. Band 1; 1. Hälfte. De Gruiter, Berlin
Rost F (1925) Pathologische Physiologie des Chirurgen. F.C.W. Vogel, Leipzig 3. Aufl. 1925
Beutner D, Hüttenbrink KB, Stumpf R, Beleites D, Zahnert T, Lüers JC, Helmstaedter V (2010) Cartilage plate tympanoplasty. Otol Neurotol 31:105–110
Shields TW (2009) General thoracic surgery, 7th edn. Lippincott Williams & Wilkins, Philadelphia
Veldman JE (1985) The Langerhans’ T cell microenvironment in aural cholesteatoma. Kugler, Amsterdam, pp 69–79
Hüttenbrink KB (2018) Eingriffe am Ohr. In: Rettinger G, Werner JA, Hosemann W, Hüttenbrink KB (eds) HNO-Operationslehre. Thieme, Stuttgart
Shimada T, Lim DJ (1972) Distribution of ciliated cells in the human middle ear. Electron and light microscopic observations. Ann Otol-Rhinol-Laryngol 81:203–211
Lund V (2002) The evolution of surgery on the maxillary sinus for chronic rhinosinusitis. Laryngoscope 112:415–419
Elliott KA, Stringer SP (2006) Evidence based recommendations for antimicrobial nasal washes in chronic rhinosinusitis. Am J Rhinol 20:1–6
Takahashi H (2012) The middle ear. Springer, Berlin
Funding
No support or funding was received for this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hüttenbrink, KB. A new theory interprets the development of a retraction pocket as a natural self-healing process. Eur Arch Otorhinolaryngol 276, 367–373 (2019). https://doi.org/10.1007/s00405-018-5246-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5246-3