Abstract
Purpose
Upper airway stimulation (UAS) is an alternative second-line treatment option for patients with obstructive sleep apnea (OSA). In our substudy of a previous multicentre study of patients implanted with UAS, we focused on patient-related outcomes like Epworth Sleepiness Scale (ESS), the Functional Outcomes of Sleep Questionnaire (FOSQ), snoring and personal satisfaction 6 and 12 months after the implantation.
Methods
60 patients, who were initially non-adherent to CPAP and implanted with UAS, were included in a prospective multicentre study. Data were collected preoperative, 6 and 12 months after implantation regarding FOSQ, ESS, snoring, and their experience with the UAS device.
Results
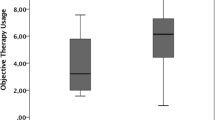
Besides relevant Apnoea–Hypopnea Index (AHI) reduction, we saw significant improvements in ESS (p < 0.001), FOSQ (p < 0.001) and snoring under UAS therapy. A strong correlation between AHI results postoperative and the personal satisfaction of the patients after implantation was found as well as between usage results and AHI compared to the preoperative results.
Conclusion
The more the patients benefit from UAS according to their self-reported outcome, the higher is the therapy use.




Similar content being viewed by others
References
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365(464):1046–1053
Heinzer R, Vat S, Marques-Vidal P et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3(4):310–318
Woehrle H, Graml A, Weinreich G (2011) Age- and gender- dependent adherence with continuous positive airway pressure therapy. Sleep Med 12(10):1034–1036
Chai-Coetzer CL, Luo YM, Antic NA et al (2013) Predictors of long-term adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea and cardiovascular disease in the SAVE study. Sleep 36(12):1929–1937
Sommer JU, Heiser C, Gahleitner C, Herr RM, Hörmann K, Maurer JT, Stuck BA (2016) Tonsillectomy with uvulopalatopharyngoplasty in obstructive sleep apnea. Dtsch Arztebl Int 113:1–8
Strollo PJ Jr, Gillespie MB, Soose RJ et al (2015) Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep 38(10):1593–1598
Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B (2017) Selective upper-airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol 274(3):1727–1734
Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A (2017) Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg 156(2):378–384
Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C (2017) Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. https://doi.org/10.1002/lary.26688
Hofauer B, Philip P, Wirth M, Knopf A, Heiser C (2017) Effects of upper-airway stimulation on sleep architecture in patients with obstructive sleep apnea. Sleep Breath 21(4):901–908
Huntley C, Kaffenberger T, Doghramji K, Soose R, Bonn M (2017) Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med 13(9):1075–1079
Steffen A, Kilic A, König IR, Suuma MV, Hofauer B, Heiser C (2017) Tongue motion variability with changes of upper airway stimulation electrode configuration and effects on treatment outcomes. Laryngoscope. https://doi.org/10.1002/lary.27064
Hofauer B, Hasselbacher K, Knopf A, Steffen A, Heiser C (2018) Adherence to upper airway stimulation in the treatment of obstructive sleep apnea. Chest 153(2):574–575
McEvoy RD, Antic NA, Heeley E et al (2016) SAVE I.A.C: CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 375:919–931
Woodson BT, Soose RJ, Gillespie MB et al (2016) Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg 154(1):181–188
Kuhn E, Schwarz EI, Bratton DJ, Rossi VA, Kohler M (2017) Effects of CPAP and mandibular advancement devices on health-related quality of life in OSA: a systematic review and meta-analysis. Chest 151(4):786–794
Heiser C, Thaler E, Boon M, Soose RJ, Woodson BT (2016) Updates of operative techniques for upper airway stimulation. Laryngoscope 126(Suppl 7):S12–S16
Heiser C, Thaler E, Soose RJ, Woodson BT, Boon M (2017) Technical tips during implantation of selective upper airway stimulation. Laryngoscope. https://doi.org/10.1002/lary.26724
R Core Team (2018) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Newson R (2002) Parameters behind “nonparametric” statistics: Kendall’s tau. Somers’ D and median differences. Stata J 2(1):45–64
Huntlex C, Kaffenberger T, Doghramji K, Soose R, Boon M (2017) Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med 13(9):1075–1079
Woodson BT, Gillespie MB, Soose RJ et al (2014) Randomized controlled withdrawal study of upper airway stimulation on OSA: short-and long-term effect. Otolaryngol Head Neck Surg 151:880–887
Gillespie MB, Soose RJ, Woodson BT et al. on Behalf of the STAR Trail Investigators (2017) Upper airway stimulation for obstructive sleep apnea: patient-reported outcomes after 48 months of follow-up. Otolaryngol Head Neck Surger 156 (4): 765–771
Acknowledgements
We are in debt to all participants of this study for their dedication to clinical research. Sleep technologists Sabrina Wenzel, Oliver Schmidt, Christian Lange, Gudrun Bunk were instrumental in overnight titration studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclosure
This study is sponsored by Inspire Medical Systems, Inc.
Conflict of interest
Katrin Hasselbacher received personal fees and travel expenses from Inspire Medical Systems. Benedikt Hofauer received personal fees and travel expenses from Inspire Medical Systems. Armin Steffen has received reimbursement of conference fees and travel and accommodation expenses, fees for preparing scientific continuing professional development or other events, funding for research he himself initiated, and fees for conducting clinical studies on related subjects from Inspire Medical Systems, and Resmed. Joachim T. Maurer has received consultancy fees, reimbursement of conference fees and travel expenses, honoraria for scientific lectures and surgical training from Neuwirth Medical, ImThera Medical, Heinen & Löwenstein, Revent Medical, MedEl, Philips, Sissel, Inspire Medical Systems, and Nyxoah. Clemens Heiser is a consultant for Inspire Medical Systems. Clemens Heiser received reimbursement of conference fees and travel and accommodation expenses from Inspire Medical Systems, Neuwirth Medical Products, Heinen & Löwenstein and Sutter Medizintechnik. Clemens Heiser received consultancy fees from Inspire Medical Systems and Sutter Medizintechnik. J. Ulrich Sommer has received consultancy fees, reimbursement of conference fees and travel and accommodation expenses, fees for preparing scientific continuing professional development or other events, funding for research he himself initiated, and fees for conducting clinical studies on related subjects from Neuwirth Medical, ImThera Medical, Fisher & Paykel Healthcare, Heinen & Löwenstein, Medtronic, Revent Medical, MedEl, Philips, Meda Pharma, Inspire Medical Systems, and Nyxoah.
Rights and permissions
About this article
Cite this article
Hasselbacher, K., Hofauer, B., Maurer, J.T. et al. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol 275, 1913–1919 (2018). https://doi.org/10.1007/s00405-018-5017-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5017-1