Abstract
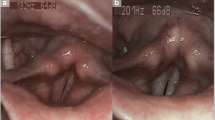
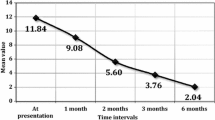
The objective is to assess the differences in the severity of symptoms, signs, voice quality, and quality of life before and after treatment according to age in suspected laryngopharyngeal reflux (LPR) patients. The design used in this paper is prospective multi-center study. Eighty clinically diagnosed LPR patients with a reflux finding score (RFS) >7 and a reflux symptom index (RSI) >13 were treated with pantoprazole and diet recommendations for 3 months. Patients were subdivided into three groups according their age: group 1 (18–39 years, N = 21), group 2 (40–59 years, N = 31), and group 3 (≥60 years, N = 28). RSI, RFS, Voice Handicap Index (VHI), Short Form 36 questionnaire (SF36), aerodynamic, and acoustic measurements were evaluated at baseline and after treatment. The response to the empiric treatment was also assessed. Significant improvements in RSI, RFS, and VHI were found in all patient groups. The elderly patients showed a significantly lower RSI score than younger subjects (p = 0.035) without RFS difference among groups. At baseline, the SF36 score was better in group 3 with respect to social functioning (p = 0.049). At the 3-month follow-up, we found significant improvement of acoustic parameters only in the younger age groups (group 1 and group 2). The rate of resistant patients to the empiric treatment was higher in the younger group than in the elderly patient group (42.9 versus 28.6%). Age appears to reduce the subjective LPR symptom perception, leading to a lower rate of uncured patients. The utilization of acoustic parameters as an indicator of treatment effectiveness seems less useful for elderly subjects, probably due to an overlap between an aging voice and LPR.

Similar content being viewed by others
References
Koufman JA, Aviv JE, Casiano RR, Shaw GY (2002) Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg 127(1):32–35
Sen P, Georgalas C, Bhattacharyya AK. A systematic review of the role of proton pump inhibitors for symptoms of laryngopharyngeal reflux. Clin Otolaryngol. 2006; 31(1):20-4; discussion 24
Jin BJ, Lee YS, Jeong SW, Jeong JH, Lee SH, Tae K (2008) Change of acoustic parameters before and after treatment in laryngopharyngeal reflux patients. Laryngoscope 118(5):938–941
Lee JS, Lee YC, Kim SW, Kwon KH, Eun YG (2014) Changes in the quality of life of patients with laryngopharyngeal reflux after treatment. J Voice 28(4):487–491
Lechien JR, Finck C, Costa de Araujo P, Huet K, Delvaux V, Piccaluga M, Harmegnies B, Saussez S (2017) Voice outcomes of laryngopharyngeal reflux treatment: a systematic review of 1483 patients. Eur Arch Otorhinolaryngol 274(1):1–23
Ulualp SO, Toohill RJ, Shaker R (2001) Outcomes of acid suppressive therapy in patients with posterior laryngitis. Otolaryngol Head Neck Surg 124(1):16–22
Lee YS, Choi SH, Son YI, Park YH, Kim SY, Nam SY (2011) Prospective, observational study using rabeprazole in 455 patients with laryngopharyngeal reflux disease. Eur Arch Otorhinolaryngol 268(6):863–869
Sataloff RT, Hawkshaw MJ, Gupta R (2010) Laryngopharyngeal reflux and voice disorders: an overview on disease mechanisms, treatments, and research advances. Discov Med. 10(52):213–224
Noordzij JP, Khidr A, Desper E, Meek RB, Reibel JF, Levine PA (2002) Correlation of pH probe-measured laryngopharyngeal reflux with symptoms and signs of reflux laryngitis. Laryngoscope 112(12):2192–2195
Ford CN (2005) Evaluation and management of laryngopharyngeal reflux. JAMA 294(12):1534–1540
Gupta N, Green RW, Megwalu UC (2016) Evaluation of a laryngopharyngeal reflux management protocol. Am J Otolaryngol 37(3):245–250
Morgan S, Smith H, Simpson I, Liddiard GS, Raphael H, Pickering RM, Mant D (1999) Prevalence and clinical characteristics of left ventricular dysfunction among elderly patients in general practice setting: cross sectional survey. BMJ 318(7180):368–372
Griffin MA, Solomon DH (1986) Hyperthyroidism in the elderly. J Am Geriatr Soc 34:887–892
Morton LS, Fromkes JJ (1993) Gastroesophageal reflux disease: diagnosis and medical therapy. Geriatrics 48(3):60–66
Lee YC, Lee JS, Kim SW, Kwon KH, Eun YG (2013) Influence of age on treatment with proton pump inhibitors in patients with laryngopharyngeal reflux disease: a prospective multicenter study. JAMA Otolaryngol Head Neck Surg. 139(12):1291–1295
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111(8):1313–1317
Koufman JA (2011) Low-acid diet for recalcitrant laryngopharyngeal reflux: therapeutic benefits and their implications. Ann Otol Rhinol Laryngol. 120(5):281–287
Lechien JR, Saussez S, Harmegnies B, Finck C, Burns JA (2017) Laryngopharyngeal reflux and voice disorders: a multifactorial model of etiology and pathophysiology. J Voice. doi:10.1016/j.jvoice.2017.03.015
Woisard V, Bodin S, Puech M (2004) The Voice Handicap Index: impact of the translation in French on the validation. Rev Laryngol Otol Rhinol (Bord) 125(5):307–312
Lechien JR, Huet K, Khalife M et al (2016) Impact of laryngopharyngeal reflux on subjective and objective voice assessments: a prospective study. J Otolaryngol Head Neck Surg 45(1):59
Koufman J, Sataloff RT, Toohill R (1996) Laryngopharyngeal reflux: consensus conference report. J Voice 10(3):215–216
Locke GR III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ III (1997) Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 112(5):1448–1456
Räihä IJ, Impivaara O, Seppälä M, Sourander LB (1992) Prevalence and characteristics of symptomatic gastroesophageal reflux disease in the elderly. J Am Geriatr Soc 40(12):1209–1211
Collen MJ, Abdulian JD, Chen YK (1995) Gastroesophageal reflux disease in the elderly: more severe disease that requires aggressive therapy. Am J Gastroenterol 90(7):1053–1057
el-Serag HB HB, Sonnenberg A (1997) Associations between different forms of gastro-oesophageal reflux disease. Gut 41(5):594–599
Li J, Zhang L, Zhang C, Cheng JY, Li J, Jeff Cheng CF (2016) Linguistic adaptation, reliability, validation, and responsivity of the Chinese version of reflux symptom index. J Voice 30(1):104–108
Kim HS, Kim DS, Kim H, Yi SM (2012) Relationship between mortality and fine particles during Asian dust, smog-Asian dust, and smog days in Korea. Int J Environ Health Res 22(6):518–530
Pascal M, de Crouy Chanel P, Wagner V et al (2016) The mortality impacts of fine particles in France. Sci Total Environ 571:416–425
Kang CM, Kang BW, Lee HS (2006) Source identification and trends in concentrations of gaseous and fine particulate principal species in Seoul, South Korea. J Air Waste Manag Assoc 56(7):911–921
Ancona C, Badaloni C, Mataloni F et al (2015) Mortality and morbidity in a population exposed to multiple sources of air pollution: a retrospective cohort study using air dispersion models. Environ Res 137:467–474
Joo YH, Lee SS, Han KD, Park KH (2015) Association between chronic laryngitis and particulate matter based on the Korea National Health and Nutrition Examination Survey 2008–2012. PLoS One 10(7):e0133180
Siupsinskiene N, Adamonis K, Toohill RJ (2007) Quality of life in laryngopharyngeal reflux patients. Laryngoscope 117(3):480–484
Karkos PD, Wilson JA (2006) Empiric treatment of laryngopharyngeal reflux with proton pump inhibitors: a systematic review. Laryngoscope 116(1):144–148
Stull DE, de de Jonge PV, Houghton K, Kocun C, Sandor DW (2011) Development of a frequent heartburn index. Qual Life Res 20(7):1023–1034
Roberts T, Morton R, Al-Ali S (2011) Microstructure of the vocal fold in elderly humans. Clin Anat 24(5):544–551
Pernambuco L, Espelt A, Góis AC, de Lima KC (2017) Voice disorders in older adults living in nursing homes: prevalence and associated factors. J Voice 31(4):510.e15–510.e21
Pernambuco L, Espelt A, Costa de Lima K (2017) Screening for voice disorders in older adults (RAVI)-part III: cutoff score and clinical consistency. J Voice 31(1):117.e17–117.e22
Graupp M, Kiesler K, Friedrich G et al (2014) Vocal fold fibroblast response to growth factor treatment is age dependent: results from an in vitro study. J Voice 28(4):420–423
Chung HY, Cesari M, Anton S et al (2009) Molecular inflammation: under- pinnings of aging and age-related diseases. Ageing Res Rev 8:18–30
Patel AK, Mildenhall NR, Kim W, Carroll TL (2014) Symptom overlap between laryngopharyngeal reflux and glottic insufficiency in vocal fold atrophy patients. Ann Otol Rhinol Laryngol 123(4):265–270
Woo P, Casper J, Colton R, Brewer D (1992) Dysphonia in the aging: physiology versus disease. Laryngoscope 102:139–144
Vaca M, Mora E, Cobeta I (2015) The aging voice: influence of respiratory and laryngeal changes. Otolaryngol Head Neck Surg 153(3):409–413
Wan Y, Yan Y, Ma F, Wang L, Lu P, Maytag A, Jiang JJ (2014) LPR: how different diagnostic tools shape the outcomes of treatment. J Voice 28(3):362–368
Vaezi MF (2006) Reflux-induced laryngitis (laryngopharyngeal reflux). Curr Treat Options Gastroenterol 9(1):69–74
Pisegna JM, Yang S, Purcell A, Rubio A (2017) A mixed-methods study of patient views on reflux symptoms and medication routines. J Voice 31(3):381.e15–381.e25
Lechien JR, Saussez S, Harmegnies B, Finck C, Burns JA (2017) Laryngopharyngeal reflux and voice disorders: a multifactorial model of etiology and pathophysiology. J Voice
Lien HC, Wang CC, Lee SW, Hsu JY, Yeh HZ, Ko CW, Chang CS, Liang WM (2015) Responder definition of a patient-reported outcome instrument for laryngopharyngeal reflux based on the US FDA guidance. Value Health 18(4):396–403
Acknowledgements
This research has been subsidized by the ARC No. AUWB-2012-12/17-UMONS convention from Communauté Française de Belgique. American Journal Expert for the proofreading of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lechien, J.R., Finck, C., Huet, K. et al. Impact of age on laryngopharyngeal reflux disease presentation: a multi-center prospective study. Eur Arch Otorhinolaryngol 274, 3687–3696 (2017). https://doi.org/10.1007/s00405-017-4671-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4671-z