Abstract
Purpose
Dietary micronutrient intakes of iron, folate and vitamin B12 are known to influence hemoglobin. Low maternal hemoglobin (maternal anemia) has been linked to low birthweight and other adverse health outcomes in the fetus and infant. Our primary aim was to explore relationships between maternal dietary micronutrient intakes, maternal full blood count (FBC) parameters and fetal abdominal circumference (AC) and estimated fetal weight (EFW) growth trajectories. Secondarily, we aimed to assess relationships between maternal dietary micronutrient intakes, maternal hemoglobin values and placental weight and birthweight.
Methods
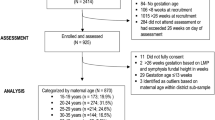
Mother–child pairs (n = 759) recruited for the ROLO study were included in this analysis. Maternal dietary micronutrient intakes were calculated from food diaries completed during each trimester of pregnancy. FBC samples were collected at 13- and 28-weeks’ gestation. Fetal ultrasound measurements were recorded at 20- and 34-weeks’ gestation. Growth trajectories for AC and EFW were estimated using latent class trajectory mixture models.
Results
Dietary intakes of iron and folate were deficient for all trimesters. Mean maternal hemoglobin levels were replete at 13- and 28-weeks’ gestation. Dietary iron, folate and vitamin B12 intakes showed no associations with fetal growth trajectories, placental weight or birthweight. Lower maternal hemoglobin concentrations at 28 weeks’ gestation were associated with faster rates of fetal growth and larger placental weights and birthweights.
Conclusion
The negative association between maternal hemoglobin at 28 weeks’ gestation and accelerated fetal and placental growth may be due to greater consumption of maternal iron and hemoglobin by fetuses’ on faster growth trajectories in addition to placental biochemical responses to lower oxygen states.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
While this study found no associations between dietary micronutrient intakes and fetal growth, we found that lower maternal hemoglobin concentrations at 28 weeks’ gestation were associated with faster rates of fetal growth and larger placental weights and birthweights. Based on these findings we postulate the ‘consumption theory’ of pregnancy: that fetuses on faster growth trajectories have a higher requirement for oxygen that results in a greater consumption of maternal iron and hemoglobin. |
Introduction
Anemia is defined as the reduced oxygen carrying capacity of blood due to low serum hemoglobin concentrations [1]. Hemoglobin concentrations are influenced by dietary micronutrient intakes of iron, vitamin B12 and folate [1]. Iron deficiency is the most widespread nutritional disorder in the world affecting up to 50% of pregnant women [2, 3]. It is by far the most common cause of anemia and has been linked to adverse health outcomes in the mother, fetus and infant [4]. Maternal iron deficiency is a risk factor for low birthweight, pre-term birth, stillbirth and perinatal death [5]. Maternal iron deficiency also increases the risk of infant anemia during the first year of life and has been associated with impaired infant cognitive function [6, 7].
Previous research has found that folate deficiency is a cause of megoblastic anemia [8], and vitamin B12 deficiency leads to pernicious anemia [9]. Deficiencies of vitamin B12 and folate may be associated with lower birthweight infants [9, 10].
Understanding the interrelation between maternal dietary micronutrient intakes, maternal hemoglobin and fetal growth may provide insight into prevention of adverse health outcomes for the fetus and infant.
Universal iron supplementation in pregnancy has been adopted by the World Health Organisation and the International Federation of Gynaecology and Obstetrics [11, 12]. Current guidance in some countries including the United Kingdom (UK) and Ireland favour dietary prevention of iron deficiency and do not commit to universal iron supplementation for all women [4, 5, 13]. This may be due, in part, to evidence suggesting that iron supplementation for pregnant women at low risk of iron deficiency, some of whom will develop iron excess with supplementation, results in a higher incidence of hypertensive disorders of pregnancy, small for gestational age infants and smaller placental weights [14, 15].
UK and Irish guidance recommend the daily consumption of 14.8 mg dietary iron and 1.5 mg dietary vitamin B12 for women of childbearing age [16,17,18]. Dietary reference intakes (DRI) of folate for this cohort vary internationally from 200 to 400 mcg daily [16, 17, 19]. Globally, it is recommended that all women take an additional daily 400 mcg folic acid supplement in the preconceptual period and for at least the first 3 months of pregnancy [17, 19]. Further research is needed into associations of maternal intakes of iron, vitamin B12 and folate during pregnancy, hemoglobin concentrations during pregnancy and measures of fetal and neonatal growth, including fetal growth trajectories as growth trajectories allow for determination of longitudinal growth patterns.
Our primary aim was to assess differences between maternal dietary micronutrient intakes (iron, folate and vitamin B12), and maternal full blood count (FBC) parameters, according to fetal abdominal circumference (AC) and estimated fetal weight (EFW) growth trajectory classes. Secondarily, we aimed to assess associations between maternal dietary micronutrient intakes (iron, folate and vitamin B12), and maternal hemoglobin, with placental weight and birthweight.
Material and methods
Study participants
This study is a secondary analysis of 759 mother–child pairs from the Randomised cOntrol trial of LOw glycaemic index diet in pregnancy to prevent macrosomia (ROLO study), conducted at the National Maternity Hospital, Dublin between 2007 and 2011 [20]. Secundagravida women aged > 18 years old, with a singleton pregnancy ≤ 18 week’s gestation, who previously delivered an infant > 4 kg in their first pregnancy, were eligible to take part [20]. Women with known medical disorders and those taking any regular medications were also excluded, in addition to women with a current or past history of gestational diabetes [20]. Women were randomised to either the intervention group where they received low glycemic index dietary advice, or to the control group where they received routine antenatal care. More detailed methods and results from the ROLO study have been published previously [20, 21].
Maternal measurements
Maternal height (m), weight (kg) and body mass index (kg/m2) were recorded at the first antenatal consultation (booking visit) at 13 weeks’ gestation (Table 1). Blood samples were also obtained at 13 weeks’ gestation and again at 28 weeks’ gestation. All bloods were processed to obtain serum samples, and serum subsequently analysed for full blood count (FBC) parameters, including hemoglobin, using the Sysmex XE-2100 fluorescence flow cytometry analyser. The results were displayed using the CliniSys WinPath laboratory information management system and accessed retrospectively for this secondary analysis. FBC reference ranges were derived from Dacie and Lewis Practical Haematology Edition 10 (2006) in line with local haematology policy [22]. Smoking status and supplement intake were self-reported by women. While nutritional supplement intake was recorded, the supplement type was not.
Dietary intake
Dietary assessments were carried out for each trimester of pregnancy using comprehensive 3-day food diaries: one in the first trimester before the low glycemic index dietary intervention and one each in the second and third trimesters of pregnancy [20]. Dietary intakes were analysed using NetWISP nutritional analysis software version 3.0 (Tinuviel software, Llanfechell, Anglesey, UK). This software package utilised the food composition database from the sixth edition of McCance and Widdowson’s food composition tables and provided an indication of the amounts and types of foods eaten, as well as the nutritional content of the women’s diets [23].
Measures of fetal growth
Fetal ultrasound measurements were obtained at 20- and 34-weeks’ gestation by one of two blinded ultrasonographers using a Voluson 730 Expert (GE Medical Systems, Germany) [20, 24]. AC and EFW were recorded. EFW was calculated using the Hadlock 4-parameter formula [25]. Infant measurements obtained at delivery included: birthweight, birth length, head circumference and abdominal circumference (Table 1). Placental weight was also recorded. Birthweight centiles were calculated using Gestation Network’s Bulk Calculator version 6.2.3 UK as described by Walsh et al. [20]. AC and EFW growth trajectory models were developed subsequently using latent class modelling as described by Bartels et al. [24]. Briefly, measures of AC and EFW collected at 20- and 34-weeks’ gestation, and weight and AC at birth were used to derive AC and EFW trajectories [24]. Two fetal growth trajectories were identified for AC: a “slow” trajectory and a “fast” trajectory [24]. For EFW, four trajectories were identified: a “very-slow” trajectory, a “moderately-slow” trajectory, a “moderately-fast” trajectory and a “very-fast” trajectory [24].
Statistical analyses
All statistical analyses were carried out using IBM Statistical Package for the Social Sciences software version 26 for Mac. Individual descriptive data were presented as mean and standard deviation or median and interquartile range depending on normality. Independent-Samples T Tests and Analysis of Variance were used with bootstrapping to explore differences between maternal FBC and dietary micronutrient parameters and the AC and EFW growth trajectories. Linear regression was completed to analyse relationships between maternal dietary micronutrient intakes and FBC results with placental weight and birthweight. Several variables were controlled for in all regression models, including randomised control trial group, maternal body mass index at booking, maternal age at delivery, use of supplements during pregnancy and maternal education status (as a surrogate for socioeconomic status). Statistical significance was set at P < 0.05.
Ethical approval
This study was Granted ethical approval and maternal written consent was obtained for all participants. Ethics Committee approval was granted by the National Maternity Hospital, Dublin in June 2006. The clinical trial registry number for the parent study is ISRCTN54392969 (http://www.isrctn.com/).
Results
Baseline characteristics for the 759 mother–child pairs analysed in the ROLO study control and intervention groups are shown in Table 1. 65.8% of women reported taking folic acid almost daily during pregnancy. 56.9% of women reported using additional supplements during pregnancy, the specifics of which were not captured as part of the ROLO study. Overall dietary intakes of iron, folate and vitamin B12 were stable across all three trimesters of pregnancy (Table 2). While dietary intakes of vitamin B12 were replete in each trimester, dietary intakes of iron and folate showed similar levels of deficiency across all three trimesters (Table 2). Maternal hemoglobin showed a downward trend from early to late pregnancy (Table 2) with 1.7% of mothers having anemia in the first trimester, and 10.9% of mothers having anemia in the third trimester. Other FBC parameters did not show the same downward trend between early and late pregnancy.
No evidence of differences in dietary intakes of iron, vitamin B12 and folate between those infants with an AC on a “slow trajectory” compared to those on a “fast trajectory” were found. Mean differences in dietary iron intake between the AC “slow” and “fast” growth trajectories were negligible across all trimesters (Table 3). All FBC parameters were similar across the three trimesters for the slow and fast AC growth trajectories (Table 3). Similarly, there were no significant differences in dietary intakes of iron, vitamin B12 and folate between the four EFW growth trajectories of “very slow”, “moderately slow”, “moderately fast” and “very fast”. There was a 1 mg mean difference in dietary iron for all trimesters between the EFW growth trajectory classes but this did not reach statistical significance (Table 4). Mean FBC parameters were also similar across the EFW growth trajectory classes. We found small but statistically significant differences, between the moderately slow and moderately fast EFW trajectory classes and hemoglobin (P = 0.046) and haematocrit (P = 0.026) in late pregnancy (28 weeks) (Table 4).
Regression models were completed to determine associations between dietary intakes, maternal hemoglobin and placental weight, taking account of confounding variables (Table 5). There were no associations between dietary intakes of iron, folate or vitamin B12 and placental weight across the three trimesters of pregnancy. There was a negative association between placental weight at birth and maternal hemoglobin at 28 weeks’ gestation (B = − 0.103 (CI − 35.05, − 2.86) P = 0.021). Associations between dietary intakes, maternal hemoglobin and birthweight were also investigated using regression models (Table 5). There were no associations between dietary intakes of iron, folate or vitamin B12 and birthweight across the three trimesters of pregnancy. Birthweight and hemoglobin at 28 weeks’ gestation were found to be negatively associated (B = − 0.107 (CI − 95.43, − 13.10) P = 0.010).
Discussion
In the current study, median dietary iron intakes were below the 14.8 mg DRI for all trimesters of pregnancy, and median dietary folate intakes were below the 400 mcg DRI across all three trimesters. Conversely, vitamin B12 intakes were above the 1.5 mcg DRI across all trimesters of pregnancy. Despite inadequate dietary intakes of both dietary iron and folate, maternal hemoglobin levels were replete at both 13- and 28-week’s gestation (Table 2). This is likely due to the fact that 56.9% of women used supplements during pregnancy, many of which may have been iron supplements. Additionally, 65.8% of women took supplemental folic acid in pregnancy.
No differences were found between dietary intakes of iron, folate or vitamin B12 between the various classes of the AC and EFW growth trajectories. Dietary data was collected using 3 day food diaries, and while food diaries are regarded as the gold standard for collection of dietary information, they are prone to reporting errors due to the burden on participants [26]. Mean maternal hemoglobin levels were higher in mothers carrying fetuses on moderately slow EFW growth trajectories compared to moderately fast EFW growth trajectories at 28 weeks’ gestation (Table 4). It should be noted that the majority of fetuses (n = 664) fell within these two trajectory classes while the other trajectory classes were small and inferences about them had lower power. We postulate that fetuses on faster growth trajectories have a higher requirement for oxygen and hemoglobin which may explain why maternal hemoglobin levels decreased across the four EFW growth trajectory classes in late pregnancy. In support of this theory, we found that neonates with higher birthweights were negatively associated with maternal hemoglobin levels at 28 weeks’ gestation (Table 5). This gives greater credence to the theory of oxygen and hemoglobin consumption by fetuses on a faster growth trajectory resulting in larger birthweights.
Maternal anemia has traditionally been seen as a risk factor for low birthweight and fetal growth restriction [27]. Studies have found lower birthweights in pregnancies with both low and high hemoglobin concentrations, thus highlighting an inverted U-shaped relationship [14, 28, 29]. The reasons for lower birthweights at the extremes of maternal hemoglobin concentrations appear to be intrinsically linked to placental growth responses to both low and high hemoglobin concentrations [14, 30]. Our findings of an overall negative association for birthweight and maternal hemoglobin at 28 week’s gestation may be relatable to the physiology of plasma volume expansion in pregnancy. We know that there is a maternal plasma volume expansion in pregnancy that leads to a reduction in hemoglobin concentration. Jwa et al. hypothesised that a reduction in maternal hemoglobin levels from early pregnancy to mid- or late pregnancy is a proxy for plasma volume increase during pregnancy that may be protective against adverse birth outcomes including delivery of a low birthweight or small for gestational age infant [31]. Previous studies have shown that the absence of an adequate increase in plasma volume in pregnancy is associated with lower birthweight and placental weights [32,33,34]. Jwa et al. showed that women with the least reduction in hemoglobin from early to late pregnancy had a significantly increased risk of delivering a low birthweight or small for gestational age infant compared to women with the intermediate or greatest reduction [31]. This may explain the negative association between late maternal hemoglobin and birthweight from our study—there was an approximate 1 g/dL mean drop in maternal hemoglobin from 13 to 28 weeks’ gestation (Table 2) which may have resulted in a suboptimal plasma volume expansion in our women throughout their pregnancies. It must be noted that there were significant differences between our own study and that of Jwa et al. The latter study had a Japanese cohort of women and maternal hemoglobin was collected at three timepoints in pregnancy in comparison to two timepoints in our own study [31]. Participants in the current study had optimal hemoglobin levels; however, further work in cohorts with suboptimal hemoglobin status is warranted. Additionally, our cohort was unique in that all of our women had previously given birth to a macrosomic infant and were thus more prone to delivering infants with larger birthweights in subsequent pregnancies based on both genetic and environmental factors.
Research has shown an association between maternal iron deficiency, maternal anemia and larger placental weights [28, 35]. Hemoglobin concentrations < 9 g/dL have been associated with the largest placental weights [14]. The mechanisms behind this association are not fully understood but studies have postulated a compensatory placental hypertrophy in response to maternal anemia [29]. We know that there is an upregulation of placental iron transport proteins such as ferroportin in placentas of anaemic mothers [36]. We also know that there is increased expression of angiogenic proteins such as vascular endothelial growth factor in the placentas of anaemic mothers which may be responsible for the hypertrophic placental response to maternal anemia [37]. On the other hand, high maternal hemoglobin concentrations have been associated with low placental weight [14]. It has been suggested that high hemoglobin concentrations may cause blood hyperviscosity, vascular occlusion and capillary congestion that may result in reduced availability of oxygen in the intervillous space and thereby suboptimal placental growth [14, 30]. Mitsuda et al. found a U-shaped relationship between maternal hemoglobin concentration and placental weight [29]. Placental weights decreased with increasing serum hemoglobin concentrations up to 12 g/dL and then increased thereafter [29]. In our study, mean hemoglobin concentrations at 28 week’s gestation were just below 12 g/dL (Table 2) which may explain our finding of a negative relationship between late maternal hemoglobin and placental weight (Table 5).
This study had a number of strengths. To our knowledge it is the first study of its kind to specifically look at the association between maternal full blood count indices and fetal growth trajectories. Several important confounders such as randomised control trial group, maternal age, body mass index, supplement use and socioeconomic status were included in regression analyses. All of these confounders have known associations with fetal and neonatal measures of growth. This study had a number of limitations. All women analysed as part of this study had previously given birth to a macrosomic infant. This makes it more difficult to relate the findings to the general pregnant population. While nutritional supplement intake was recorded, the supplement name was not so it is not known if supplements containing iron were consumed by women participating in this study. The current study includes FBC data only—inclusion of other biomarkers of iron status, such as serum ferritin and serum transferrin receptor, would facilitate a more complete analysis of the interplay between iron intakes, hemoglobin and fetal growth. The use of linear regression models in our study failed to address the possibility of potential non-linear relationships for our cohort—other studies have shown a non-linear relationship between maternal hemoglobin concentration and placental weight and birthweight [29]. Lastly, the trajectories used in this analysis were exploratory and need careful replication or refinement in similar populations.
Conclusion
Dietary intakes of iron, folate and vitamin B12 showed no association with fetal AC and EFW growth trajectory classes, birthweight or placental weight. Lower maternal hemoglobin concentrations at 28 weeks’ gestation were associated with faster rates of fetal growth and larger placental weights and birthweights. These findings may be due to biochemical responses in the placenta to lower oxygen states, physiological protective expansions in plasma volume later in pregnancy and potentially greater consumption of maternal iron and hemoglobin by fetuses on accelerated growth trajectories.
Data availability
The authors confirm that all relevant data supporting the findings of this study are included within the paper. Any additional data required may be requested from the corresponding author.
Abbreviations
- AC:
-
Abdominal circumference
- DRI:
-
Dietary reference intakes
- EFW:
-
Estimated fetal weight
- FBC:
-
Full blood count
- ROLO:
-
Randomised cOntrol trial of LOw glycaemic index diet in pregnancy to prevent macrosomia
- UK:
-
United Kingdom
References
World Health Organization (2017) Nutritional anaemias: tools for effective prevention and control. https://www.who.int/publications/i/item/9789241513067. Accessed 02 Dec 2022
Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, Peña-Rosas JP, Bhutta ZA, Ezzati M (2013) Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health 1:e16-25. https://doi.org/10.1016/s2214-109x(13)70001-9
Alwan NA, Hamamy H (2015) Maternal iron status in pregnancy and long-term health outcomes in the offspring. J Pediatr Genet 4:111–123. https://doi.org/10.1055/s-0035-1556742
Pavord S, Daru J, Prasannan N, Robinson S, Stanworth S, Girling J, Committee BSH (2020) UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol 188:819–830. https://doi.org/10.1111/bjh.16221
Food Safety Authority of Ireland (2011) Scientific recommendations for a national infant feeding policy, 2nd edition. http://www.hdl.handle.net/10147/253492. Accessed 02 Dec 2022
Freeman VE, Mulder J, van’t Hof MA, Hoey HM, Gibney MJ (1998) A longitudinal study of iron status in children at 12, 24 and 36 months. Public Health Nutr 1:93–100. https://doi.org/10.1079/phn19980015
Tamura T, Goldenberg RL, Hou J, Johnston KE, Cliver SP, Ramey SL, Nelson KG (2002) Cord serum ferritin concentrations and mental and psychomotor development of children at five years of age. J Pediatr 140:165–170. https://doi.org/10.1067/mpd.2002.120688
Finkelstein JL, Layden AJ, Stover PJ (2015) Vitamin B-12 and perinatal health. Adv Nutr 6:552–563. https://doi.org/10.3945/an.115.008201
Molloy AM, Kirke PN, Brody LC, Scott JM, Mills JL (2008) Effects of folate and vitamin B12 deficiencies during pregnancy on fetal, infant, and child development. Food Nutr Bull 29:S101-111. https://doi.org/10.1177/15648265080292S114. (discussion S112-105)
Rogne T, Tielemans MJ, Chong MF, Yajnik CS, Krishnaveni GV, Poston L, Jaddoe VW, Steegers EA, Joshi S, Chong YS, Godfrey KM, Yap F, Yahyaoui R, Thomas T, Hay G, Hogeveen M, Demir A, Saravanan P, Skovlund E, Martinussen MP, Jacobsen GW, Franco OH, Bracken MB, Risnes KR (2017) Associations of maternal vitamin B12 concentration in pregnancy with the risks of preterm birth and low birth weight: a systematic review and meta-analysis of individual participant data. Am J Epidemiol 185:212–223. https://doi.org/10.1093/aje/kww212
Di Renzo GC, Fonseca E, Gratacos E, Hassan S, Kurtser M, Malone F, Simpson SNKNNSHYCFVBECMMHMHYVGVJL (2019) Good clinical practice advice: Iron deficiency anemia in pregnancy. Int J Gynaecol Obstet 144:322–324. https://doi.org/10.1002/ijgo.12740
World Health Organization (2012) Guideline: daily iron and folic acid supplementation in pregnant women. https://www.ncbi.nlm.nih.gov/books/NBK132263/. Accessed 02 Dec 2022
Food Safety Authority of Ireland (2012) Best practice for infant feeding in Ireland: from pre-conception through the first year of an infant’s life. http://www.hdl.handle.net/10147/252765. Accessed 02 Dec 2022
Larsen S, Bjelland EK, Haavaldsen C, Eskild A (2016) Placental weight in pregnancies with high or low hemoglobin concentrations. Eur J Obstet Gynecol Reprod Biol 206:48–52. https://doi.org/10.1016/j.ejogrb.2016.08.039
Dewey KG, Oaks BM (2017) U-shaped curve for risk associated with maternal hemoglobin, iron status, or iron supplementation. Am J Clin Nutr 106:1694S-1702S. https://doi.org/10.3945/ajcn.117.156075
Committee on Medical Aspects of Food and Nutrition Policy, Public Health England (1991) Dietary reference values—a guide. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/743790/Dietary_Reference_Values_-_A_Guide__1991_.pdf. Accessed 02 Dec 2022
Health Service Executive (2021) B vitamins and folic acid. https://www.2.hse.ie/conditions/vitamins-and-minerals/b-vitamins-and-folic-acid/. Accessed 28 Aug 2022
Health Service Executive (2021) Iron. https://www2.hse.ie/conditions/vitamins-and-minerals/iron/. Accessed 28 Aug 2022
Prevention CfDCa (2022) Folic Acid. National center on birth defects and developmental disabilities, centers for disease control and prevention. https://www.cdc.gov/ncbddd/folicacid/about.html. Accessed 28 Aug 2022
Walsh JM, McGowan CA, Mahony R, Foley ME, McAuliffe FM (2012) Low glycaemic index diet in pregnancy to prevent macrosomia (ROLO study): randomised control trial. BMJ 345:e5605. https://doi.org/10.1136/bmj.e5605
Horan MK, McGowan CA, Gibney ER, Donnelly JM, McAuliffe FM (2014) Maternal diet and weight at 3 months postpartum following a pregnancy intervention with a low glycaemic index diet: results from the ROLO randomised control trial. Nutrients 6:2946–2955. https://doi.org/10.3390/nu6072946
Lewis SM (2006) Chapter 2—Reference ranges and normal values. In: Lewis SM, Bain BJ, Bates I (eds) Dacie and lewis practical haematology, 10th edn. Churchill Livingstone, Philadelphia, pp 11–24. https://doi.org/10.1016/B0-44-306660-4/50006-4
McCance RA, Widdowson EM (2002) The Composition of Foods. Royal Society of Chemistry. https://www.books.google.ie/books?id=ALDkOIwZod8C. Accessed 02 Dec 2022
Bartels HC, O’Connor C, Segurado R, Mason O, Mehegan J, Geraghty AA, O’Brien E, Walsh J, McAuliffe F (2020) Fetal growth trajectories and their association with maternal and child characteristics. J Matern Fetal Neonatal Med 33:2427–2433. https://doi.org/10.1080/14767058.2018.1554041
Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK (1985) Estimation of fetal weight with the use of head, body, and femur measurements–a prospective study. Am J Obstet Gynecol 151:333–337. https://doi.org/10.1016/0002-9378(85)90298-4
Biro G, Hulshof KF, Ovesen L, Amorim Cruz JA, Group E (2002) Selection of methodology to assess food intake. Eur J Clin Nutr 56(Suppl 2):S25-32. https://doi.org/10.1038/sj.ejcn.1601426
Figueiredo ACMG, Gomes-Filho IS, Silva RB, Pereira PPS, Mata FAFD, Lyrio AO, Souza ES, Cruz SS, Pereira MG (2018) Maternal anemia and low birth weight: a systematic review and meta-analysis. Nutrients 10:601. https://doi.org/10.3390/nu10050601
Godfrey KM, Redman CW, Barker DJ, Osmond C (1991) The effect of maternal anaemia and iron deficiency on the ratio of fetal weight to placental weight. Br J Obstet Gynaecol 98:886–891. https://doi.org/10.1111/j.1471-0528.1991.tb13510.x
Mitsuda N, NA J-P, Eitoku M, Maeda N, Fujieda M, Suganuma N, Kamijima M, Yamazaki S, Kishi R, Yaegashi N, Hashimoto K, Mori C, Ito S, Yamagata Z, Inadera H, Nakayama T, Iso H, Shima M, Kurozawa Y, Suganuma N, Kusuhara K, Katoh T (2020) Association between maternal hemoglobin concentration and placental weight to birthweight ratio: the Japan environment and children’s study (JECS). Placenta 101:132–138. https://doi.org/10.1016/j.placenta.2020.09.014
Koller O, Sandvei R, Sagen N (1980) High hemoglobin levels during pregnancy and fetal risk. Int J Gynaecol Obstet 18:53–56. https://doi.org/10.1002/j.1879-3479.1980.tb00241.x
Jwa SC, Fujiwara T, Yamanobe Y, Kozuka K, Sago H (2015) Changes in maternal hemoglobin during pregnancy and birth outcomes. BMC Pregnancy Childbirth 15:80. https://doi.org/10.1186/s12884-015-0516-1
Hays PM, Cruikshank DP, Dunn LJ (1985) Plasma volume determination in normal and preeclamptic pregnancies. Am J Obstet Gynecol 151:958–966. https://doi.org/10.1016/0002-9378(85)90675-1
Salas SP, Rosso P, Espinoza R, Robert JA, Valdés G, Donoso E (1993) Maternal plasma volume expansion and hormonal changes in women with idiopathic fetal growth retardation. Obstet Gynecol 81:1029–1033
Whittaker PG, Macphail S, Lind T (1996) Serial hematologic changes and pregnancy outcome. Obstet Gynecol 88:33–39. https://doi.org/10.1016/0029-7844(96)00095-6
Beischer NA, Sivasamboo R, Vohra S, Silpisornkosal S, Reid S (1970) Placental hypertrophy in severe pregnancy anaemia. J Obstet Gynaecol Br Commonw 77:398–409. https://doi.org/10.1111/j.1471-0528.1970.tb03541.x
Venkata Surekha M, Sujatha T, Gadhiraju S, Kotturu SK, Siva Prasad M, Sarada K, Bhaskar V, Uday Kumar P (2020) Effect of maternal iron deficiency anaemia on the expression of iron transport proteins in the third trimester placenta. Fetal Pediatr Pathol. https://doi.org/10.1080/15513815.2020.1725942
Venkata Surekha M, Singh S, Sarada K, Sailaja G, Balakrishna N, Srinivas M, Uday Kumar P (2019) Study on the effect of severity of maternal iron deficiency anemia on regulators of angiogenesis in placenta. Fetal Pediatr Pathol 38:361–375. https://doi.org/10.1080/15513815.2019.1587120
Funding
Open Access funding provided by the IReL Consortium. The ROLO study was funded by the Health Research Board of Ireland, with additional financial support from the National Maternity Hospital, Dublin Medical Fund. None of the funding sources had a role in the ROLO trial design or in this manuscript preparation.
Author information
Authors and Affiliations
Contributions
DJR: Data collection, Data Analysis, Manuscript Writing. MC: Project Development, Data Analysis, Manuscript Editing. LMO: Project Development, Data Analysis, Manuscript Editing. CMM: Project Development, Manuscript Editing. HCB: Project Development, Manuscript Editing. CY: Data Management, Manuscript Editing. RS: Data Management, Data Analysis. JM: Data Management. FMM: Project Development, Project Supervision, Manuscript Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rooney, D.J., Conway, M., O’Keeffe, L.M. et al. Dietary intakes of iron, folate, and vitamin B12 during pregnancy and correlation with maternal hemoglobin and fetal growth: findings from the ROLO longitudinal birth cohort study. Arch Gynecol Obstet 309, 183–193 (2024). https://doi.org/10.1007/s00404-023-06916-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06916-x