Abstract
Purpose
The aim of this meta-analysis was to evaluate the risk of chromosomal abnormalities in fetuses with congenital heart disease (CHD).
Methods
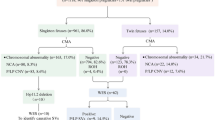
Four literature databases were searched until 17th January 2022 using the relevant medical subject heading terms, word variants, and keywords for “congenital heart defect, fetal, and chromosomal abnormalities”. The prevalence of overall chromosomal abnormality, aneuploidy, 22q11 deletion, other copy number variants (CNVs), and variants of unknown significance (VOUS) was analyzed.
Results
45 studies met the inclusion criteria for the analysis. The pooled proportion of overall chromosomal abnormalities, aneuploidy, 22q11 deletion, and other CNVs in fetuses with CHD was 23% (95% CI: 20–26%), 19% (95% CI, 16–22%), 2% (95% CI, 2–3%), and 4% (95% CI, 3–5%), respectively. The incidence of overall chromosomal abnormalities, aneuploidy, and other CNVs in non-isolated CHD was higher than in isolated CHD, with odds ratios of 3.08, 3.45, and 4.02, respectively. The incidence of overall chromosomal abnormalities in septal defects was higher than in conotruncal defects and other defects, with odds ratios of 1.60 and 3.61, respectively. In addition, the pooled proportion of VOUS in CHD was 4%.
Conclusion
CHD is commonly associated with chromosomal abnormalities. If karyotyping or fluorescence in situ hybridization is normal, chromosomal microarray should be performed to look for submicroscopic abnormalities, especially in fetuses with non-isolated CHD and septal defects.





Similar content being viewed by others
Data availability
The datasets supporting the conclusions of this article are included within the article and its additional files. Further inquiries can be directed to the corresponding author.
References
Liu Y, Chen S, Zühlke L, Black GC, Choy MK, Li N, Keavney BD (2019) Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol 48:455–463
Qiu X, Weng Z, Liu M, Chen X, Wu Q, Ling W, Ma H, Huang H, Lin Y (2020) Prenatal diagnosis and pregnancy outcomes of 1492 fetuses with congenital heart disease: role of multidisciplinary-joint consultation in prenatal diagnosis. Sci Rep 10:7564
Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM, Savage M, Platt LD, Saltzman D, Grobman WA, Klugman S, Scholl T, Simpson JL, McCall K, Aggarwal VS, Bunke B, Nahum O, Patel A, Lamb AN, Thom EA, Beaudet AL, Ledbetter DH, Shaffer LG, Jackson L (2012) Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med 367:2175–2184
Costain G, Silversides CK, Bassett AS (2016) The importance of copy number variation in congenital heart disease. NPJ Genom Med 1:16031
Levy B, Wapner R (2018) Prenatal diagnosis by chromosomal microarray analysis. Fertil Steril 109:201–212
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P (2015) NewcastleOttawa Scale for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Accessed 20 November 2015]
Higgins JPT, Green S (2009) Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration 2009.www.cochranehandbook.org. [Accessed 10 December 2016].
Efthimiou O (2018) Practical guide to the meta-analysis of rare events. Evid Based Ment Health 21:72–76
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Simonyi A, Eros FR, Hajdu J, Beke A (2021) Effectiveness of fetal ultrasound diagnostics in cardiac malformations and association with polyhydramnios and oligohydramnios. Quant Imaging Med Surg 11:2994–3004
Huang J, Deng X, Wang Y, Tang N, Zeng D (2020) Analysis of copy number variations by low-depth whole-genome sequencing in fetuses with congenital cardiovascular malformations. Cytogenet Genome Res 160:643–649
Luo X, Zhu H, Wang L, Xiao B, Fan Y, Ye H, Ying X, Qiu W, Zhang H, Han L, Gu X, Yu Y, Wang L (2021) Chromosomal microarray analysis in fetuses with high-risk prenatal indications: a retrospective study in China. Taiwan J Obstet Gynecol 60:299–304
Chang CS, Hong SY, Kim SY, Kim YM, Sung JH, Choi SJ, Oh SY, Roh CR, Song J, Huh J, Kang IS (2021) Prevalence of associated extracardiac anomalies in prenatally diagnosed congenital heart diseases. PLoS ONE 16:e0248894
Mone F, Stott BK, Hamilton S, Seale AN, Quinlan-Jones E, Allen S, Hurles ME, McMullan DJ, Maher ER, Kilby MD (2021) The diagnostic yield of prenatal genetic technologies in congenital heart disease: a prospective cohort study. Fetal Diagn Ther 5:1–8
Evans WN, Ruben J (2021) Acherman, Humberto Restrepo, advanced maternal age and critical congenital cardiac malformations in Nevada. Progr Pediat Cardiol. 62:101385
Qiao F, Wang Y, Zhang C, Zhou R, Wu Y, Wang C, Meng L, Mao P, Cheng Q, Luo C, Hu P, Xu Z (2021) Comprehensive evaluation of genetic variants using chromosomal microarray analysis and exome sequencing in fetuses with congenital heart defect. Ultrasound Obstet Gynecol 58:377–387
Pavlicek J, Gruszka T, Polanska S, Dolezalkova E, Matura D, Spacek R, Simetka O, Salounova D, Kacerovsky M (2020) Parents’ request for termination of pregnancy due to a congenital heart defect of the fetus in a country with liberal interruption laws. J Matern Fetal Neonatal Med 33:2918–2926
Han B, Li Y, Tang Y, Qu X, Wang F, Song H, Xu Y (2019) Clinical analysis of prenatal ultrasound diagnosis of fetal cardiovascular malformations in the first and second trimesters of pregnancy: a CARE-compliant article. Medicine 98:e16822
Song T, Wan S, Li Y, Xu Y, Dang Y, Zheng Y, Li C, Zheng J, Chen B, Zhang J (2019) Detection of copy number variants using chromosomal microarray analysis for the prenatal diagnosis of congenital heart defects with normal karyotype. J Clin Lab Anal 33:e22630
Sagi-Dain L, Maya I, Reches A, Frumkin A, Grinshpun-Cohen J, Segel R, Manor E, Khayat M, Tenne T, Banne E, Shalata A, Yonath H, Berger R, Singer A, Ben-Shachar S (2018) Chromosomal microarray analysis results from pregnancies with various ultrasonographic anomalies. Obstet Gynecol 132:1368–1375
Cai M, Huang H, Su L, Lin N, Wu X, Xie X, An G, Li Y, Lin Y, Xu L (2018) Fetal congenital heart disease: Associated anomalies, identification of genetic anomalies by single-nucleotide polymorphism array analysis, and postnatal outcome. Medicine 97:e13617
Liu L, Wang HD, Cui CY, Yao HM, Huang L, Li T, Fan TB, Peng BT, Zhang LZ (2018) Investigating the characteristics of echocardiogram, surgical treatment, chromosome and prognosis for fetal right heart enlargement: A STROBE-compliant article. Medicine 97:e13307
Luo S, Meng D, Li Q, Hu X, Chen Y, He C, Xie B, She S, Li Y, Fu C (2018) Genetic testing and pregnancy outcome analysis of 362 fetuses with congenital heart disease identified by prenatal ultrasound. Arq Bras Cardiol 111:571–577
Xia Y, Yang Y, Huang S, Wu Y, Li P, Zhuang J (2018) Clinical application of chromosomal microarray analysis for the prenatal diagnosis of chromosomal abnormalities and copy number variations in fetuses with congenital heart disease. Prenat Diagn 38:406–413
Turan S, Asoglu MR, Gabbay-Benziv R, Doyle L, Harman C, Turan OM (2018) Yield rate of chromosomal microarray analysis in fetuses with congenital heart defects. Eur J Obstet Gynecol Reprod Biol 221:172–176
Sukenik-Halevy R, Sukenik S, Koifman A, Alpert Y, Hershkovitz R, Levi A, Biron-Shental T (2016) Clinical aspects of prenatally detected congenital heart malformations and the yield of chromosomal microarray analysis. Prenat Diagn 36:1185–1191
Zhu X, Li J, Ru T, Wang Y, Xu Y, Yang Y, Wu X, Cram DS, Hu Y (2016) Identification of copy number variations associated with congenital heart disease by chromosomal microarray analysis and next-generation sequencing. Prenat Diagn 36:321–327
Bensemlali M, Bajolle F, Ladouceur M, Fermont L, Lévy M, Le Bidois J, Salomon LJ, Bonnet D (2016) Associated genetic syndromes and extracardiac malformations strongly influence outcomes of fetuses with congenital heart diseases. Arch Cardiovasc Dis 109:330–336
Fesslova’ V, Brankovic J, Boschetto C, Masini A, Prandstraller D, Perolo A, Ventriglia F, Macerola S, Crepaz R, Romeo C, De Luca F, Previtera A, Errico G (2015) Fetal Study Group of Italian Society of Pediatric Cardiology. Changed outcomes of fetuses with congenital heart disease: new Italian Multicentre study. J Cardiovasc Med 16:568–575
Mone F, Walsh C, Mulcahy C, McMahon CJ, Farrell S, MacTiernan A, Segurado R, Mahony R, Higgins S, Carroll S, McParland P, McAuliffe FM (2015) Prenatal detection of structural cardiac defects and presence of associated anomalies: a retrospective observational study of 1262 fetal echocardiograms. Prenat Diagn 35:577–582
Zhang J, Ma D, Wang Y, Cao L, Wu Y, Qiao F, Liu A, Li L, Lin Y, Liu G, Liu C, Hu P, Xu Z (2015) Analysis of chromosome 22q11 copy number variations by multiplex ligation-dependent probe amplification for prenatal diagnosis of congenital heart defect. Mol Cytogenet 8:100
Lv W, Wang S (2014) Detection of chromosomal abnormalities and the 22q11 microdeletion in fetuses with congenital heart defects. Mol Med Rep 10:2465–2470
Mademont-Soler I, Morales C, Soler A, Martínez-Crespo JM, Shen Y, Margarit E, Clusellas N, Obón M, Wu BL, Sánchez A (2013) Prenatal diagnosis of chromosomal abnormalities in fetuses with abnormal cardiac ultrasound findings: evaluation of chromosomal microarray-based analysis. Ultrasound Obstet Gynecol 41:375–382
Bao B, Wang Y, Hu H, Yao H, Li Y, Tang S, Zheng L, Xu Y, Liang Z (2013) Karyotypic and molecular genetic changes associated with fetal cardiovascular abnormalities: results of a retrospective 4-year ultrasonic diagnosis study. Int J Biol Sci 9:463–471
Acevedo-Gallegos S, García M, Benavides-Serralde A, Camargo-Marín L, Aguinaga-Ríos M, Ramírez-Calvo J, Velázquez-Torres B, Gallardo-Gaona J, Guzmán-Huerta M (2013) Association between selected structural defects and chromosomal abnormalities. Rev Invest Clin 65:248–254
Hartman RJ, Rasmussen SA, Botto LD, Riehle-Colarusso T, Martin CL, Cragan JD, Shin M, Correa A (2011) The contribution of chromosomal abnormalities to congenital heart defects: a population-based study. Pediatr Cardiol 32:1147–1157
Clur SA, Van Brussel PM, Mathijssen IB, Pajkrt E, Ottenkamp J, Bilardo CM (2011) Audit of 10 years of referrals for fetal echocardiography. Prenat Diagn 31:1134–1140
Bellucco FT, Belangero SI, Farah LM, Machado MV, Cruz AP, Lopes LM, Lopes MA, Zugaib M, Cernach MC, Melaragno MI (2010) Investigating 22q11.2 deletion and other chromosomal aberrations in fetuses with heart defects detected by prenatal echocardiography. Pediatr Cardiol 31:1146–1150
Hsiao SM, Wu MH, Jou HJ, Lee CN, Shyu MK, Shih JC, Hsieh FJ (2007) Outcome for fetuses with prenatally detected congenital heart disease and cardiac arrhythmias in Taiwan. J Formos Med Assoc 106:423–431
Tegnander E, Williams W, Johansen OJ, Blaas HG, Eik-Nes SH (2006) Prenatal detection of heart defects in a non-selected population of 30,149 fetuses–detection rates and outcome. Ultrasound Obstet Gynecol 27:252–265
Li H, Wei J, Ma Y, Shang T (2005) Prenatal diagnosis of congenital fetal heart abnormalities and clinical analysis. J Zhejiang Univ Sci B 6:903–906
Moore JW, Binder GA, Berry R (2004) Prenatal diagnosis of aneuploidy and deletion 22q11.2 in fetuses with ultrasound detection of cardiac defects. Am J Obstet Gynecol 191:2068–2073
Boldt T, Andersson S, Eronen M (2002) Outcome of structural heart disease diagnosed in utero. Scand Cardiovasc J 36:73–79
Bronshtein M, Zimmer EZ (2002) The sonographic approach to the detection of fetal cardiac anomalies in early pregnancy. Ultrasound Obstet Gynecol 19:360–365
Mirlesse V, Cruz A, Le Bidois J, Diallo P, Fermont L, Kieffer F, Magny JF, Jacquemard F, Levy R, Voyer M, Daffos F (2001) Perinatal management of fetal cardiac anomalies in a specialized obstetric-pediatrics center. Am J Perinatol 18:363–371
Manji S, Roberson JR, Wiktor A, Vats S, Rush P, Diment S, Van Dyke DL (2001) Prenatal diagnosis of 22q11.2 deletion when ultrasound examination reveals a heart defect. Genet Med 3:65–66
Eronen M (1997) Outcome of fetuses with heart disease diagnosed in utero. Arch Dis Child Fetal Neonatal Ed 77:F41–F46
Respondek ML, Binotto CN, Smith S, Donnenfeld A, Weil SR, Huhta JC (1994) Extracardiac anomalies, aneuploidy and growth retardation in 100 consecutive fetal congenital heart defects. Ultrasound Obstet Gynecol 4:272–278
Achiron R, Rotstein Z, Lipitz S, Mashiach S, Hegesh J (1994) First-trimester diagnosis of fetal congenital heart disease by transvaginal ultrasonography. Obstet Gynecol 84:69–72
Brown DL, Emerson DS, Shulman LP, Doubilet PM, Felker RE, Van Praagh S (1993) Predicting aneuploidy in fetuses with cardiac anomalies: significance of visceral situs and noncardiac anomalies. J Ultrasound Med 12:153–161
Smythe JF, Copel JA, Kleinman CS (1992) Outcome of prenatally detected cardiac malformations. Am J Cardiol 69:1471–1474
Callan NA, Maggio M, Steger S, Kan JS (1991) Fetal echocardiography: indications for referral, prenatal diagnoses, and outcomes. Am J Perinatol 8:390–394
Copel JA, Cullen M, Green JJ, Mahoney MJ, Hobbins JC, Kleinman CS (1988) The frequency of aneuploidy in prenatally diagnosed congenital heart disease: an indication for fetal karyotyping. Am J Obstet Gynecol 158:409–413
Wolter A, Markert N, Wolter JS, Kurkevych A, Degenhardt J, Ritgen J, Stressig R, Enzensberger C, Bedei I, Vorisek C, Schenk J, Graupner O, Khalil M, Thul J, Jux C, Axt-Fliedner R (2021) Natural history of pulmonary atresia with intact ventricular septum (PAIVS) and critical pulmonary stenosis (CPS) and prediction of outcome. Arch Gynecol Obstet 304:81–90
Zaidi S, Brueckner M (2017) Genetics and Genomics of Congenital Heart Disease. Circ Res 120:923–940
Salzer-Sheelo L, Polak U, Barg A, Kahana S, Yacobson S, Agmon-Fishman I, Klein C, Matar R, Rurman-Shahar N, Sagi-Dain L, Basel-Salmon L, Maya I, Sukenik-Halevy R (2022) Prenatal and postnatal chromosomal microarray analysis in 885 cases of various congenital heart defects. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-021-06366-3. (Advance online publication)
Jansen FA, Blumenfeld YJ, Fisher A, Cobben JM, Odibo AO, Borrell A, Haak MC (2015) Array comparative genomic hybridization and fetal congenital heart defects: a systematic review and meta-analysis. Ultrasound Obstet Gynecol 45:27–35
Hou HT, Chen HX, Wang XL, Yuan C, Yang Q, Liu ZG, He GW (2020) Genetic characterisation of 22q11.2 variations and prevalence in patients with congenital heart disease. Arch Dis Child 105:367–374
Hureaux M, Guterman S, Hervé B, Till M, Jaillard S, Redon S, Valduga M, Coutton C, Missirian C, Prieur F, Simon-Bouy B, Beneteau C, Kuentz P, Rooryck C, Gruchy N, Marle N, Plutino M, Tosca L, Dupont C, Puechberty J, Schluth-Bolard C, Salomon L, Sanlaville D, Malan V, Vialard F (2019) Chromosomal microarray analysis in fetuses with an isolated congenital heart defect: a retrospective, nationwide, multicenter study in France. Prenat Diagn 39:464–470
Maran S, Faten SA, Lim SE, Lai KS, Ibrahim WPW, Ankathil R, Gan SH, Tan HL (2020) Screening of 22q11.2DS using multiplex ligation-dependent probe amplification as an alternative diagnostic method. Biomed Res Int 2020:6945730
Nagy O, Szakszon K, Biró BO, Mogyorósy G, Nagy D, Nagy B, Balogh I, Ujfalusi A (2019) Copy number variants detection by microarray and multiplex ligation-dependent probe amplification in congenital heart diseases. J Biotechnol 299:86–95
Recker F, Weber EC, Strizek B, Geipel A, Berg C, Gembruch U (2022) Management and outcome of prenatal absent pulmonary valve syndrome. Arch Gynecol Obstet. https://doi.org/10.1007/s00404-022-06397-4. (Advance online publication)
Abel JS, Berg C, Geipel A, Gembruch U, Herberg U, Breuer J, Brockmeier K, Gottschalk I (2021) Prenatal diagnosis, associated findings and postnatal outcome of fetuses with truncus arteriosus communis (TAC). Arch Gynecol Obstet 304:1455–1466
Darbar D (2021) Unraveling the genomic basis of congenital heart disease. J Clin Investig 131:e145377
Hsiao CH, Chen JS, Shiao YM, Chen YJ, Chen CH, Chu WC, Wu YC (2022) Prenatal diagnosis using chromosomal microarray analysis in high-risk pregnancies. J Clin Med 11:3624
Orlando V, Alesi V, Di Giacomo G, Canestrelli M, Calacci C, Nardone AM, Calvieri G, Liambo MT, Sallicandro E, Di Tommaso S, Di Gregorio MG, Corrado F, Barrano G, Niceta M, Dallapiccola B, Novelli A (2021) Clinical application of easychip 8×15K platform in 4106 pregnancies without ultrasound anomalies. Reprod Sci 28:1142–1149
Funding
This work was supported by the Qihang Fund of Fujian Medical University [grant number 2020QH2039] and the Collaborative Innovation Center of Maternal and Child Health Service Technology from Fujian Medical College [grant number XJM1802].
Author information
Authors and Affiliations
Contributions
All authors had full access to all of the data in this study and take responsibility for the integrity of the data and the accuracy of the data analysis. HW: was involved in study design, search in databases, analysis, and interpretation of data, manuscript drafting, and critical discussion. GL: was involved in the study design, critical discussion, and revising of the manuscript. XL: was involved in searching databases and analyzing and interpreting data. SH: was involved in data extraction and statistical analysis. BD: was involved in the search for databases and manuscript drafting. YY: was involved in statistical analysis and study supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare. The authors have no ethical conflicts to disclose. It is a meta-analysis and all references are published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Lin, X., Lyu, G. et al. Chromosomal abnormalities in fetuses with congenital heart disease: a meta-analysis. Arch Gynecol Obstet 308, 797–811 (2023). https://doi.org/10.1007/s00404-023-06910-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06910-3