Abstract
Purpose
Although pregnancy and childbirth are physiological processes they may be associated with pelvic floor disorders. The aim of this study was to evaluate the influence of pelvic floor muscle training on postpartum pelvic floor and sexual function of primiparous.
Methods
This is a randomized prospective study including 300 primiparous women. Due to the dropout 200 women were analyzed. Inclusion criteria were the delivery of the first, mature baby, the ability to speak and understand German. The participants were evaluated by clinical examinations and questionnaires after 6 and 12 months postpartum. After 6 months, the women were randomized in two groups. Compared to the control group the intervention groups participated in 45-min pelvic floor muscle training and pelvic floor perception once a week over 6 weeks.
Results
The results of the questionnaires showed no significant differences between the groups after 12 months. A significant stronger pelvic floor muscle strength was found for the intervention group after 12 months. The improvement of the pelvic floor and sexual function over the time showed a significant improvement in both groups.
Conclusion
Supervised pelvic floor muscle training did not improve both the pelvic floor and the female sexual function in comparison to the control group. After 12 months, the pelvic floor and sexual function improved significant in all women.
Trial registration
German Clinical Trials Register (DRKS00024725), retrospectively registrated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although pregnancy and childbirth are physiological processes, they may be associated with potential physical problems. It is known that up to 42% parous women suffer of urinary incontinence (UI), in primiparous 12–35% are affected by flatal incontinence and up to 9.5% are involuntary losing formed stool years after delivery [1]. Besides, two thirds of parous women have anatomical evidence of pelvic organ prolapse [2], however the majority of these women are asymptomatic [3]. Another important topic during and after pregnancy is the change in sexual life. This still seems to be a taboo topic as it is not regularly integrated in the gynecological checkups. Therefore the validated Female Sexual Function Index (FSFI) questionnaire is a great tool to advance research in this topic [4]. Many postpartum problems originate from pelvic floor disorders. The question arises whether pelvic floor muscle training (PFMT) has an influence on the sexual and the pelvic floor function. Martinez et al. 2014 stated, that women with stronger pelvic floor muscles have better sexual function, though the mechanism by which this is achieved is not clearly understood [5]. The systematic review of Ferreira et al. concludes that most studies indicated an improvement of at least one sexual variable due to PFMT [6]. Out of the included studies Citak et al. found positive effects of PFMT 4 months postpartum in primiparous women on the female sexual function as well has on the pelvic floor muscle [7].
The effect of PFMT on urinary and fecal continence postpartum is controversially discussed. The Cochrane analysis of Woodley et al. demonstrated that antenatal conducted PFMT reduced the risk in continent women of becoming incontinent in pregnancy and later. However, PFMT carried out antenatally or postpartum in incontinent women could not prove efficiency [1].
To gain more knowledge of the influence of PFMT on the pelvic floor and sexual function, this randomized study was conducted. The goal was to find ways to help affected women, breaking taboo topics and highlighting the importance of health care workers to speak about these topics.
Material and methods
Ethical board approval and registration
This study was approved by the ethics committee Ulm, Germany (377/16) and registered in German Clinical Trials Register (DRKS00024725). Informed consent was obtained from all participants.
Study design, participants
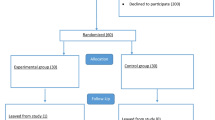
All primiparous, who delivered in our hospital between 2018—2019, were asked to take part. Women were informed about the study by a doctor using written and verbal information. Inclusion criteria were primiparous with a term baby and the ability to speak German fluently. Exclusion criteria were secondipara or above, a premature delivery and language barriers. Due to the new approach of this study, no comparable studies were found to carry out a reliable power analysis. Recruitment was stopped when the number of 300 women were included (Fig. 1). The participants were evaluated by examinations and questionnaires (see Examination, Questionnaire) at 6 (T1) and 12 (T2) months postpartum. The women were instructed to carry out the planed postnatal gymnastic to represent reality. At T1, the women were randomized in two groups (see Randomization, Intervention). At T1 200, at T2 164 women participated (Fig. 1). Reasons for the loos to follow-up were moves, limited time, fear of the corona virus, corona infection, other illnesses and no interest. The primary outcome was the effect of PFMT on the FSFI and the Pelvic floor questionnaire for pregnant women and women after childbirth (PFQ). Secondary outcomes were the influence of the PFMT on the grade of prolapse, the pelvic floor muscle contraction and the effect of time between 6 and 12 months.
Examination
Participants at 6 and 12 months postpartum received questionnaires and underwent a gynecologic examination. This included a speculum examination to evaluate the degree of the prolapse with the pelvic organ prolapse quantification system (POP-Q, [8]). The POP-Q staging is rated from 0 (no prolapse) to 4 (total prolapse). An evaluation of pelvic floor contraction was conducted using the Oxford Score [9]. A modified Oxford Score from 1 (no contraction), 2 (weak), 3 (moderate), 4 (good) to 5 (strong) was used. Four gynecologists specialized in urogynecology performed alternately the examination.
Questionnaires
Women received the German FSFI-d and the PFQ
FSFI-d
The FSFI-d is the German version of the FSFI questionnaire; a 19-item English questionnaire including the domains desire, arousal, lubrication, orgasm, satisfaction, pain. Each domain has a maximum value of 6. The FSFI total score ranges from 2 to 36 [4, 10]. 15 of the items contain a zero option to indicate either “no sexual activity” (12 items) or “did not attempt intercourse” (3 items). The absence of sexual activity or intercourse is not attributable to sexual dysfunction. The incorrect use of the zero category in calculating FSFI domains, except desire, and the total score would underestimate women’s sexual functioning scores [11]. All scores, except desire, were excluded for these women in the analysis. A total score ≤ 26.55 is indicative for female sexual dysfunction (FSD) [12]. Therefore, in both groups, the proportion of FSD was evaluated
PFQ
The PFQ consisting of question regarding the delivery, demographic data and 42 specific questions. These specific questions counted in the score and encompassing the four areas of bladder-, anal-, prolapse- and sexual function [13]. The four areas were scaled from 0 (no dysfunction) to 10 (maximal dysfunction). The areas were summated, giving a total score of 0–40.
Randomization and intervention
A block randomization in two groups, IG—and CG, took place after 6 months. The randomization was prepared in advance with sealed envelopes for a target size of 300 participants. These were opened in the presence of the participants after the examination. The IG comprised weekly, 45-min pelvic floor training for 6 weeks, in groups of ten women instructed by professional pelvic floor physiotherapists. The training included pelvic floor perception based on the Franklin-Method and pelvic floor muscle training. The Franklin-Method uses mental images in combination of physical training. The participants in the IG were asked to do the exercise daily. The CG was asked to do the exercises they had learned in the postnatal gymnastic daily. Out of the IG, 12 women did not take part in the professional pelvic floor training. They were excluded for the statistical analyses.
Statistical analysis
Statistical analysis was carried out using IBM SPSS Statistics V26. Quantitative data were represented by min, max, median, interquartile range, or mean and standard deviation. Comparisons between IG and CG were analyzed by Man-Whitney U or t-test, improvement over time between groups was reported by the corresponding differences and analyzed by repeated measurement design. Qualitative data were examined by Chi Square test with Fisher’s exact method in case of expected cell frequency below 5. McNemar test was used for comparison over time. No missing data were imputed resulting in different number of cases in the tests.
Results
Study population
Figure 1 shows the number of participants and the lost to follow-up. Table 1 shows the demographic characteristics. The two groups were balanced with no significant differences regarding the demographic factors, examination findings and the questionnaires. Regarding sexual intercourse no significant difference was shown between the groups at T1. The analyses between the lost to follow-ups between T1 and T2 showed no significant difference for demographic factors, examination findings and the FSFI score. The lost to follow-ups had a significant better PFQ total score (p = 0.004).
Intervention
18% of the women in the IG did not take part. 6% of the women joined 17%, 2% joined 33%, 74% joined ≥ 50% of training. Those with \(\le \) 50% adherence (with one exception) had a bladder score \(\le \) 1.75 at T1. Furthermore, all participants who had a bladder score > 1.75 at T1 attended > 50% of appointments (except the same one exception) (Fig. 2). There was a significant correlation between an initially higher bladder score and therapy adherence (p = 0.025; Fig. 2).
Participants with a bladder score > 1.75 after 6 months out of the PFQ* attended more than 50% of the appointments. Participants out of the interventions group with additional pelvic floor muscle training and a therapy adherence < 50% had a bladder score (with one exception) < 1.75. Significant correlation (r = 0.231) between an initially higher bladder score after 6 months and therapy adherence in % (p = 0.025). *Pelvic floor questionnaire for pregnant women and women after childbirth
Group comparisons at T2
At T1, 77% of the IG and 73% of the CG had sexual intercourse. At T2, 82% of the women in the control group (CG), 86% of the participants in the intervention group (IG) were included.
Table 2 demonstrates the differences of the FSFI (T2-T1) and the PFQ (T1-T2) over time for each group and compares them. None of the domains were found to be significantly set apart. The POP-Q score showed no significant difference for both groups (IG: p = 0.053; CG: p = 0.545; group comparison p = 0.281). A significant higher Oxford score was found for the IG (IG p = 0.005; CG p = 0.111; group comparison p = 0.018; Table 3). Frequency of sexual intercourse after 12 months showed a significant change in the IG, and a positive trend in the CG. The group comparison was not 55.
Improvement over the time
Both groups showed a significant improvement in the FSFI scores over time. The IG demonstrated a significant improvement over time of the total score (p = 0.001), the domains desire (p = 0.000), arousal (p = 0 0.043), lubrication (p = 0.002), orgasm (p = 0.010), pain (p = 0.000). Only satisfaction was not significant (p = 0.153). The following results were found for the CG: Total score (p = 0.000; Fig. 3), the domains desire (p = 0.000), arousal (p = 0.001), lubrication (p = 0.000), orgasm (p = 0.012), satisfaction (p = 0.005), pain (p = 0.000). Regarding the question whether there is sexual intercourse no significant difference could be shown over time.
In respect to the PFQ except for the bladder score, all scores were significant improving over the time. IG: total score (p = 0.000; Fig. 3), bladder score (p = 0.354), anal score (p = 0.005), prolapse score (p = 0.005), sexual score (p = 0.000). CG: total score (p = 0.000), bladder score (p = 0.051), anal score (p = 0.002), prolapse score (p = 0.001), sexual score (p = 0.000).
Regarding the examination the POP-Q score showed a positive trend over time, however no significant change in both groups and in the group comparison (IG: p = 0.053; CG: 0.545; group comparison p = 0.281; Table 3). A significant higher Oxford score was found for the IG after 12 months (IG p = 0.005; CG p = 0.111; group comparison p = 0.018; Table 3).
FSD
The proportion of participants with a FSFI total score ≤ 26.55 did not differ between the groups at T1 (p = 0.926). A risk for FSD was identified in 42.9% of CG and 43.2% of IG. After intervention 11.9% of the CG and 22.7% of the IG were indicative for FSD (Table 3). The proportion of participants with FSD did not differ significantly between the groups after intervention (p = 0.186). In both groups, there was a significant improvement over time (CG p = 0.001, IG p = 0.049; Table 3).
Discussion
The demographic and clinical characteristics were similar in the IG and CG indicating a balanced study population, which is an important foundation to compare these groups. Comparing this collective with the data of Metz et al. a better initial bladder function could be shown, which might be due to the high number of women with the ability to voluntarily contract the pelvic floor muscle [13]. An in-ability to voluntarily contract the pelvic floor muscle goes along with pelvic floor dysfunctions [13].
The main question of this study is the influence of additional PFMT on the sexual and pelvic floor function. Interestingly, participants with a worse bladder score showed a higher therapy adherence. This could be explained due to a higher initial level of suffering.
In the main domains of the FSFI and the PFQ no significant differences could be shown between the groups. This is in accordance with other studies [14,15,16]. Ahlund et al. randomized 100 primiparous women in home-base PFMT between 3–9 months after delivery. Both groups were re-examined and assessed 9 months postpartum. No differences between these groups were found, both groups showed a significantly better muscle strength after the intervention time [15]. Other studies demonstrated a positive effect of PFMT on the sexual function [6, 17, 18] as well as on the pelvic floor function [16, 19]. The results of our study could be explained by the socio-demographic characteristics of the subjects: highly motivated participants, recruited from a clinic with high socio-economic status. As Baumann et al. stated, both social influences and motivation could be important determinants of adherence to training [20]. It is known, that independent practice in addition to the exercise lessons improves the effectiveness of the postnatal gymnastics [21]. The CG was most likely well motivated and probably adhered to their learned PFMT to the same extent as the IG.
The additional PFMT had a significant effect on the strength of the pelvic floor muscles in this study. However, no association between a stronger pelvic floor muscle and a better sexual function, as demonstrated by Martinez et al., could been shown [5]. It should be mentioned that the Oxford Score, as well as the Ortiz scale used by Martinez et al., are subjectively ascertained parameters [5]. Elenskaia et al. stated that the pelvic floor weakens temporarily after childbirth, but contractility appears to recover by 1 year irrespective of the mode of delivery [22].
The frequency of sexual intercourse over time increased significantly in the IG and tendentiously but not significantly in the CG. However, the comparison between the groups on T2 was not significant. Overall about 50% had regular sexual activity at T2, which highlights the importance of time and the ability to talk about problems regarding this topic during the PFMT.
A significant improvement of pelvic floor and sexual function over the time could be shown in both study groups in almost all domains. This is in line with the studies of Ahlund et al. and Elenskaia et al. [15, 22]. These significant improvement over time can be seen in context with the normal reparative process, the adaption to a live with a baby, the influence of the estrogen level due to 5ation as well as the probably highly motivated participants, who carried out PFMT regularly. This is important for counseling couples antenatally; thus averting many problems in the postnatal period as pelvic floor disorders can have a detrimental effect on a woman’s quality of life.
The bladder score showed no significant improvement over the time. It is known that the strength of the pelvic floor muscles decrease during pregnancy and in the first months after childbirth due to hormonal and anatomical changes, which could lead to UI [23]. The Cochrane analyses of Woodley et al. demonstrated that it is uncertain whether a population-based approach for delivering postnatal PFMT is effective in reducing UI. It should be mentioned that the included studies were not large and most had design problems including limited details to the PFMT, the randomization and poor reporting of the measurements. Uncertainty surrounds the effects of PFMT as a treatment for UI in antenatal and postnatal women, while it is accepted to be effective in mid-life women [1, 24]. Hilde et al. 2013 found, that PFMT does not decrease UI prevalence 6 months after delivery in primiparous women [25]. These data are in line with our findings. The following factors might have an influence. Our study population was not separated for risk factors regarding UI and it seems questionable to compare women after delivery, with those in their mid-life age.
Up to two-thirds of postpartum women have a FSD during the first year after delivery [26, 27]. In this study collective, up to one half of the participants had a risk for FSD, however, after 12 months 22.7% in the IG and 11.9% in the CG suffered from residual FSD. This highlights the importance of time. Our results seem better than those reported in the literature, which may be explained by a better open communication about sexuality in both groups as part of the present study.
Nevertheless, there are limitations. There was a low consistent participation and no control of the regularity of the daily training. A training diary would have been necessary. The CG received no instructions, only the request to continue the exercises as before to simulate the reality. The meta-analysis of García-Sánchez et al. recommends programs which should last 6–12 weeks, with more than three sessions weekly and a length less than 45 min to get the best effect of PFMT on UI [28]. Programs more than three times a week are difficult to implement for mothers with small children. Therefore, the participants were asked to continue doing the learned exercise daily. The clinical examination was conducted by four specialized gynecologists; however, an inter-rater reliability was not raised. Another limitation regards the loos to follow-up, with a high number of participants missing in the final analysis, and the time of the follow-ups. This study should have been ideally carried over a longer time to examine long-term outcome.
In summary supervised PFMT improved the pelvic floor muscle strength but did not improve both the pelvic floor and the female sexual function. Further long-term studies are necessary to evaluate the effect of strict PFMT on the pelvic and sexual function. After 12 months the pelvic floor and the sexual function improved significant in all women highlighting the importance of time in pelvic floor recovery. An open communication about this improvement already antenatally could probably prevent problems for the affected women.
Abbreviations
- FSFI:
-
Female sexual function index
- PFQ:
-
Pelvic floor questionnaire for pregnant women and women after childbirth
- PFMT:
-
Pelvic floor muscle training
- POP-Q:
-
Pelvic organ prolapse quantification system
- FSD:
-
Female sexual dysfunction
- IG:
-
Intervention group
- CG:
-
Control group
- UI:
-
Urinary incontinence
References
Woodley SJ, Lawrenson P, Boyle R et al (2020) Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 92:909. https://doi.org/10.1002/14651858.CD007471.pub4
Bump RC, Norton PA (1998) Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 25:723–746. https://doi.org/10.1016/s0889-8545(05)70039-5
Swift SE, Tate SB, Nicholas J (2003) Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol 189:372 7 discussion-377 9. https://doi.org/10.1067/s0002-9378(03)00698-7
Berner MM, Kriston L, Zahradnik HP et al (2004) Überprüfung der Gültigkeit und Zuverlässigkeit des deutschen Female Sexual Function Index (FSFI-d). Geburtsh Frauenheilk 64:293–303. https://doi.org/10.1055/s-2004-815815
Martinez CS, Ferreira FV, Castro AAM, Gomide LB (2014) Women with greater pelvic floor muscle strength have better sexual function. Acta Obstet Gynecol Scand 93:497–502. https://doi.org/10.1111/aogs.12379
Ferreira CHJ, Dwyer PL, Davidson M et al (2015) Does pelvic floor muscle training improve female sexual function? A systematic review. Int Urogynecol J 26:1735–1750. https://doi.org/10.1007/s00192-015-2749-y
Citak N, Cam C, Arslan H et al (2010) Postpartum sexual function of women and the effects of early pelvic floor muscle exercises. Acta Obstet Gynecol Scand. https://doi.org/10.3109/00016341003801623
Persu C, Chapple CR, Cauni V et al (2011) Pelvic organ prolapse quantification system (POP-Q)—a new era in pelvic prolapse staging. J Med Life 4:75–81
Isherwood PJ, Rane A (2000) Comparative assessment of pelvic floor strength using a perineometer and digital examination. BJOG 107:1007–1011. https://doi.org/10.1111/j.1471-0528.2000.tb10404.x
Rosen C, Brown J, Heiman S, Leib R (2000) The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208. https://doi.org/10.1080/009262300278597
Meston CM, Freihart BK, Handy AB et al (2019) Scoring and interpretation of the FSFI: what can be learned from 20 years of use? J Sex Med. https://doi.org/10.1016/j.jsxm.2019.10.007
Wiegel M, Meston C, ROSEN R, (2005) The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 31:1–20. https://doi.org/10.1080/00926230590475206
Metz M, Junginger B, Henrich W, Baessler K (2017) Development and validation of a questionnaire for the assessment of pelvic floor disorders and their risk factors during pregnancy and post partum. Geburtsh Frauenheilk 77:358–365. https://doi.org/10.1055/s-0043-102693
Kolberg MT, Hilde G, Jensen JS et al (2016) Effect of postpartum pelvic floor muscle training on vaginal symptoms and sexual dysfunction—secondary analysis of a randomised trial. BJOG 123:634–642. https://doi.org/10.1111/1471-0528.13823
Åhlund S, Nordgren B, Wilander E-L et al (2013) Is home-based pelvic floor muscle training effective in treatment of urinary incontinence after birth in primiparous women? A randomized controlled trial. Acta Obstet Gynecol Scand 92:909–915. https://doi.org/10.1111/aogs.12173
Harvey M-A (2003) Pelvic floor exercises during and after pregnancy: a systematic review of their role in preventing pelvic floor dysfunction. J Obstet Gynaecol Can 25:487–498. https://doi.org/10.1016/s1701-2163(16)30310-3
Hadizadeh-Talasaz Z, Sadeghi R, Khadivzadeh T (2019) Effect of pelvic floor muscle training on postpartum sexual function and quality of life: a systematic review and meta-analysis of clinical trials. Taiwan J Obstet Gynecol 58:737–747. https://doi.org/10.1016/j.tjog.2019.09.003
del Carmen C-F, Aibar-Almazán A, Martínez-Amat A et al (2020) Effects of physical exercise on sexual function and quality of sexual life related to menopausal symptoms in peri- and postmenopausal women: a systematic review. IJERPH 17:2680. https://doi.org/10.3390/ijerph17082680
Kahyaoglu Sut H, Balkanli Kaplan P (2016) Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and the postpartum period. Neurourol Urodyn 35:417–422. https://doi.org/10.1002/nau.22728
Bauman AE, Sallis JF, Dzewaltowski DA, Owen N (2002) Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med 23:5–14. https://doi.org/10.1016/s0749-3797(02)00469-5
Mørkved S, Bø K (1996) The effect of post-natal exercises to strengthen the pelvic floor muscles. Acta Obstet Gynecol Scand 75:382–385. https://doi.org/10.3109/00016349609033336
Elenskaia K, Thakar R, Sultan AH et al (2011) The effect of pregnancy and childbirth on pelvic floor muscle function. Int Urogynecol J 22:1421–1427. https://doi.org/10.1007/s00192-011-1501-5
Soave I, Scarani S, Mallozzi M et al (2019) Pelvic floor muscle training for prevention and treatment of urinary incontinence during pregnancy and after childbirth and its effect on urinary system and supportive structures assessed by objective measurement techniques. Arch Gynecol Obstet 299:609–623. https://doi.org/10.1007/s00404-018-5036-6
Dumoulin C, Cacciari LP, Hay-Smith EJC (2018) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 10:CD005654. https://doi.org/10.1002/14651858.CD005654.pub4
Hilde G, Stær-Jensen J, Siafarikas F et al (2013) Postpartum pelvic floor muscle training and urinary incontinence. Obstet Gynecol 122:1231–1238. https://doi.org/10.1097/AOG.0000000000000012
Rezaei N, Azadi A, Sayehmiri K, Valizadeh R (2017) Postpartum sexual functioning and its predicting factors among iranian women. Malays J Med Sci 24:94–103. https://doi.org/10.21315/mjms2017.24.1.10
Khajehei M, Doherty M, Tilley PJM, Sauer K (2015) Prevalence and risk factors of sexual dysfunction in postpartum Australian women. J Sex Med 12:1415–1426. https://doi.org/10.1111/jsm.12901
García-Sánchez E, Ávila-Gandía V, López-Román J et al (2019) What pelvic floor muscle training load is optimal in minimizing urine loss in women with stress urinary incontinence? A systematic review. IJERPH. https://doi.org/10.3390/ijerph16224358
Acknowledgements
The authors would like to thank the participants, the physiotherapists and the Department of Obstetrics and Gynecology in Ulm for the financial support.
Funding
Open Access funding enabled and organized by Projekt DEAL. The clinic provided the finances for the additional pelvic floor muscle training included in this study.
Author information
Authors and Affiliations
Contributions
MD, SS designed and supervised the project; conducted the examinations; wrote the article. MH, MU coordinated the appointments; conducted the examinations and collected the data. JS performed the statistical analysis and revised the manuscript. BH revised the manuscript, edited language. WJ revised the manuscript, edited language and supported the work financially.
Corresponding author
Ethics declarations
Competing interests
All authors declare that they have no conflict of interest.
Ethics approval
The study was performed in line with the principles of the Declaration of Helsinki and approved by the ethics committee of the University of Ulm, Germany (377/16). It was registered in German Clinical Trials Register (DRKS00024725).
Consent to participate
Informed consent was obtained from all participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schütze, S., Heinloth, M., Uhde, M. et al. The effect of pelvic floor muscle training on pelvic floor function and sexuality postpartum. A randomized study including 300 primiparous. Arch Gynecol Obstet 306, 785–793 (2022). https://doi.org/10.1007/s00404-022-06542-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06542-z