Abstract
Purpose
Sexual violence is a global health problem. We aimed to evaluate the association between self-reported history of sexual violence and parturients’ health behaviors, focusing on routine gynecological care, and mental well-being.
Methods
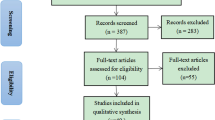
This was a retrospective questionnaire-based study, including mothers of newborns delivered at the “Soroka” University Medical Center (SUMC). Participants were asked to complete three validated questionnaires, including: screening for sexual violence history (SES), post-traumatic stress disorder (PDS) and post-partum depression (EPDS). Additionally, a demographic, pregnancy and gynecological history data questionnaire was completed, and medical record summarized. Multiple analyses were performed, comparing background and outcome variables across the different SES severity levels. Multivariable regression models were constructed, while adjusting for confounding variables.
Results
The study included 210 women. Of them, 26.3% (n = 57) reported unwanted sexual encounter, 23% (n = 50) reported coercion, 1.8% (n = 4) assault and attempted rape, and 1.4% (n = 3) reported rape. A significant association was found between sexual violence history and neglected gynecological care, positive EPDS screening, and reporting experiencing sexual trauma. Several multivariable regression models were constructed, to assess independent associations between sexual violence history and gynecological health-care characteristics, as well as EPDS score. Sexual violence history was found to be independently and significantly associated with a negative relationship with the gynecologist, avoidance of gynecological care, sub-optimal routine gynecological follow-up, and seeking a gynecologist for acute symptoms (adjusted OR = 0.356; 95% CI 0.169–0.749, adjusted OR = 0.369; 95% CI 0.170–0.804, adjusted OR = 2.255; 95% CI 1.187–4.283, and adjusted OR = 2.113; 95% CI 1.085–4.111, respectively), as well as with the risk of post-partum depression (adjusted OR = 4.46; 95% CI 2.03–9.81). All models adjusted for maternal age and ethnicity.
Conclusion
Sexual violence history is extremely common among post-partum women. It is independently associated with post-partum depression, neglected gynecological care, a negative relationship with the gynecologist, and with reporting of experiencing sexual trauma. Identifying populations at risk and taking active measures, may reduce distress and improve emotional well-being and family function.
Similar content being viewed by others
Data availability
All are available.
References
Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R (2002) World report on violence and health. World Health Organization, Geneva
Garcia-Moreno C, Zimmerman C, Morris-Gehring A, Heise L, Amin A, Abrahams N et al (2015) Addressing violence against women: a call to action. Lancet 385(9978):1685–1695
Tavara L (2006) Sexual violence. Best Pract Res Clin Obstet Gynaecol 20(3):395–408
Garcia-Moreno C, Pallitto C, Devries K, Stöckl H, Watts C, Abrahams N et al (2013) Global and regional estimates of violence against women. World Health Organization, Italy
Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S (2009) Burden and consequences of child maltreatment in high-income countries. Lancet 373(9657):68–81
Jones JS, Alexander C, Wynn BN, Rossman L, Dunnuck C (2009) Why women don’t report sexual assault to the police: the influence of psychosocial variables and traumatic injury. J Emerg Med 36(4):417–424
Ministry of public security of Israel (2014) National Violence Index.
Moor A (2009) Prevalence of exposure to sexual violence among women in Israel: preliminary assessment. Social Issues Israel 7:46–65
Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Chen J, Stevens MR (2011) The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta
OECD (2011) Compendium of OECD Well-Being Indicators. OECD
United Nations Office on Drugs and Crime (UNODC) (2011) PRINCIPLES AND FRAMEWORK FOR AN INTERNATIONAL CLASSIFICATION OF CRIMES FOR STATISTICAL PURPOSES REPORT OF THE UNODC/UNECE TASK FORCE ON CRIME CLASSIFICATION
Belik SL, Stein MB, Asmundson GJ, Sareen J (2009) Relation between traumatic events and suicide attempts in Canadian military personnel. Can J Psychiatry 54(2):93–104
Australian Institute of Health and Welfare (AIHW) (2018) Family, domestic and sexual violence in Australia. AIHW, Canberra
Jina R, Thomas LS (2013) Health consequences of sexual violence against women. Best Pract Res Clin Obstet Gynaecol 27(1):15–26
Sharman LS, Douglas H, Price E, Sheeran N, Dingle GA (2018) Associations between unintended pregnancy, domestic violence, and sexual assault in a population of Queensland women. Psychiatr Psychol Law 26(4):541–552
Mark H, Bitzker K, Klapp BF, Rauchfuss M (2008) Gynaecological symptoms associated with physical and sexual violence. J Psychosom Obstet Gynaecol 29(3):164–172
McCall-Hosenfeld JS, Liebschutz JM, Spiro A, Seaver MR (2009) Sexual assault in the military and its impact on sexual satisfaction in women veterans: a proposed model. J Womens Health (Larchmt) 18(6):901–909
Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN et al (2010) Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clin Proc 85(7):618–629
Weitlauf JC, Finney JW, Ruzek JI, Lee TT, Thrailkill A, Jones S, Frayna SM (2008) Distress and pain during pelvic examinations: effect of sexual violence. Obstet Gynecol 112(6):1343–1350
ACOG Committee (2018) ACOG committee opinion No. 755: well-woman visit. Obstetrics Gynecol 132(4):1084–1085
Kirkham C, Harris S, Grzybowski S (2005) Evidence-based prenatal care: part I. General prenatal care and counseling issues. Am Fam Physician 71(7):1307–1316
Kirkham C, Harris S, Grzybowski S (2005) Evidence-based prenatal care: part II. Third-trimester care and prevention of infectious diseases. Am Fam Physician 71(8):1555–1560
Lukasse M, Henriksen L, Vangen S, Schei B (2012) Sexual violence and pregnancy-related physical symptoms. BMC Pregnancy Childbirth 12:83
Henriksen L, Schei B, Vangen S, Lukasse M (2014) Sexual violence and mode of delivery: a population-based cohort study. BJOG 121(10):1237–1244
Gisladottir A, Harlow BL, Gudmundsdottir B, Bjarnadottir RI, Jonsdottir E, Aspelund T et al (2014) Risk factors and health during pregnancy among women previously exposed to sexual violence. Acta Obstet Gynecol Scand 93(4):351–358
Gisladottir A, Luque-Fernandez MA, Harlow BL, Gudmundsdottir B, Jonsdottir E, Bjarnadottir RI et al (2016) Obstetric outcomes of mothers previously exposed to sexual violence. PLoS ONE 11(3):e0150726
Rich-Edwards JW, James-Todd T, Mohllajee A, Kleinman K, Burke A, Gillman MW, Wright RJ (2011) Lifetime maternal experiences of abuse and risk of pre-natal depression in two demographically distinct populations in Boston. Int J Epidemiol 40(2):375–384
Leeners B, Stiller R, Block E, Gorres G, Rath W (2010) Pregnancy complications in women with childhood sexual abuse experiences. J Psychosom Res 69(5):503–510
Leeners B, Stiller R, Block E, Gorres G, Rath W, Tschudin S (2013) Prenatal care in adult women exposed to childhood sexual abuse. J Perinat Med 41(4):365–374
Yampolsky L, Lev-Wiesel R, Ben-Zion IZ (2010) Child sexual abuse: is it a risk factor for pregnancy? J Adv Nurs 66(9):2025–2037
Guintivano J, Manuck T, Meltzer-Brody S (2018) Predictors of postpartum depression: a comprehensive review of the last decade of evidence. Clin Obstet Gynecol 61(3):591–603
Wosu AC, Gelaye B, Williams MA (2015) History of childhood sexual abuse and risk of prenatal and postpartum depression or depressive symptoms: an epidemiologic review. Arch Womens Ment Health 18(5):659–671
Rogathi JJ, Manongi R, Mushi D, Rasch V, Sigalla GN, Gammeltoft T et al (2017) Postpartum depression among women who have experienced intimate partner violence: a prospective cohort study at Moshi, Tanzania. J Affect Disord 218:238–245
Wu Q, Chen HL, Xu XJ (2012) Violence as a risk factor for postpartum depression in mothers: a meta-analysis. Arch Womens Ment Health 15(2):107–114
Merrick J, Al-Krenawi A, Elbedour S (2013) Bedouin Health: perspectives from Israel. Nova Biomedical, New York
DellaPergola S (2016) World Jewish Population, 2015. In: Dashefsky A, Sheskin I (eds) American Jewish Year Book 2015. American Jewish Year Book, vol 115. Springer, Cham
Stavsky M, Robinson R, Sade MY, Krymko H, Zalstein E, Ioffe V, Novack V, Levitas A (2017) Elevated birth prevalence of conotruncal heart defects in a population with high consanguinity rate. Cardiol Young 27(1):109–116
Koss MP, Oros CJ (1982) Sexual Experiences Survey: a research instrument investigating sexual aggression and victimization. J Consult Clin Psychol 50(3):455–457
Foa EB, Cashman L, Jaycox L, Perry K (1997) The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Psychol Assess 9(4):445–451
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry 150:782–786
Grekin R, O’Hara MW (2014) Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev 34(5):389–401
Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I (2013) Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. J Midwifery Womens Health 58(1):57–68
Hilden M, Sidenius K, Langhoff-Roos J, Wijma B, Schei B (2003) Women’s experiences of the gynecologic examination: factors associated with discomfort. Acta Obstet Gynecol Scand 82(11):1030–1036
Güneş G, Karaçam Z (2017) The feeling of discomfort during vaginal examination, history of abuse and sexual abuse and post-traumatic stress disorder in women. J Clin Nurs 26(15–16):2362–2371
Resnick HS, Acierno R, Kilpatrick DG (1997) Health impact of interpersonal violence. 2: medical and mental health outcomes. Behav Med 23(2):65–78
Golding JM, Cooper ML, George LK (1997) Sexual assault history and health perceptions: seven general population studies. Health Psychol 16(5):417–425
Tsai J (2019) Resistance and surrender—remembering to bow to strength. Not Power N Engl J Med 380(5):412–413
Cadman L, Waller J, Ashdown-Barr L, Szarewski A (2012) Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plann Reprod Health Care 38(4):214–220
Mazor E, Sheiner E, Wainstock T, Attias M, Walfisch A (2019) The association between depressive state and maternal cognitive function in postpartum women. Am J Perinatol 36(3):285–290
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TR: Project development, Data Collection, Data management, Data analysis, Manuscript writing. AW: Project development, Data analysis, Manuscript editing. ES: Project development, Manuscript editing. LAE: Data Collection. SZ: Data Collection. AA: Data Collection. TW: Data analysis, Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local institutional ethical review board (SUMC IRB).
Consent to participate
All women provided oral and written consent to participate in the study.
Consent for publication
All authors consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Razi, T., Walfisch, A., Sheiner, E. et al. #metoo? The association between sexual violence history and parturients’ gynecological health and mental well-being. Arch Gynecol Obstet 304, 385–393 (2021). https://doi.org/10.1007/s00404-021-05977-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-021-05977-0