Abstract
Purpose
To contribute to establishing donor selection criteria based on our experience with two successful living-donor human uterus transplantations (UTx) and an aborted attempt.
Methods
This interventional study included three patients with uterine agenesis, aged 23, 34, and 23 years, scheduled for UTx, and their uterus-donating mothers, aged 46, 61, and 46 years, respectively. Interventions included preoperative investigations, donor surgery, back-table preparation, and recipient surgery. Preoperative imaging, surgical data, histopathology, menstrual pattern, and uterine blood flow were the main outcome measures.
Results
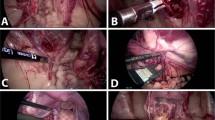
In the first case (46-year-old mother/23-year-old daughter), donor/recipient surgery took 12.12/5.95 h. Regular spontaneous menstruations started 6-week post-transplantation, continuing at 24–28-day intervals throughout the 6-month observation period. Repeated follow-up cervical biopsies showed no signs of rejection. In the second case (61-year-old donor), surgery lasted 13.10 h; attempts to flush the retrieved uterus failed due to extreme resistance of the left uterine artery (UA) and inability to perfuse the right UA. Transplantation was aborted to avoid graft vessel thrombosis or insufficient blood flow during potential pregnancy. Histopathology revealed intimal fibrosis and initial sclerosis (right UA), extensive intimal fibrosis (parametric arterial segments), and subtotal arterial stenosis (myometrial vascular network). In the third case (46-year-old mother/23-year-old daughter), donor/recipient surgery took 9.05/4.52 h. Menstruations started 6-week post-transplantation. Repeated cervical biopsies showed no signs of rejection during the initial 12-week follow-up period.
Conclusions
Meticulous preoperative evaluation of potential living uterus donors is essential. This may include selective contrast-enhanced UA angiograms and limitation of donor age, at least in donors with risk factors for atherosclerosis.
Clinical trial registration
ClinicalTrials.gov Identifier: NCT03048396.



Similar content being viewed by others
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- AUFI:
-
Absolute uterine factor infertility
- BMI:
-
Body mass index
- CMV:
-
Cytomegalovirus
- CT:
-
Computed tomography
- EBV:
-
Epstein Barr virus
- HbA1c:
-
Glycated hemoglobin
- HC2:
-
Hybrid Capture 2
- HDL:
-
High-density lipoprotein
- HLA:
-
Human leukocyte antigen
- HPV:
-
Human papilloma virus
- HRT:
-
Hormone replacement therapy
- HTK:
-
Histidine-tryptophan-ketoglutarate (solution)
- IFCC:
-
International Federation for Clinical Chemistry
- IVF:
-
In vitro fertilization
- LDL:
-
Low-density lipoprotein
- MRA:
-
Magnetic resonance angiography
- MRKHS:
-
Mayer–Rokitansky–Küster–Hauser syndrome
- Pap:
-
Papanicolaou (smear)
- UA:
-
Uterine artery
- UTx:
-
Uterus transplantation
References
Lefkowitz A, Edwards M, Balayla J (2012) The montreal criteria for the ethical feasibility of uterine transplantation. Transpl Int 25(4):439–447. https://doi.org/10.1111/j.1432-2277.2012.01438.x
Milliez J (2009) Uterine transplantation FIGO Committee for the Ethical Aspects of Human Reproduction and Women’s Health. Int J Gynaecol Obstet 106(3):270. https://doi.org/10.1016/j.ijgo.2009.03.045
Akhi SN, Diaz-Garcia C, El-Akouri RR, Wranning CA, Mölne J, Brännström M (2013) Uterine rejection after allogeneic uterus transplantation in the rat is effectively suppressed by tacrolimus. Fertil Steril 99(3):862–870. https://doi.org/10.1016/j.fertnstert.2012.11.002
Brännström M, Diaz-Garcia C, Hanafy A, Olausson M, Tzakis A (2012) Uterus transplantation: animal research and human possibilities. Fertil Steril 97(6):1269–1276. https://doi.org/10.1016/j.fertnstert.2012.04.001
Diaz-Garcia C, Akhi SN, Martinez-Varea A, Brännström M (2013) The effect of warm ischemia at uterus transplantation in a rat model. Acta Obstet Gynecol Scand 92(2):152–159. https://doi.org/10.1111/aogs.12027
Diaz-Garcia C, Johannesson L, Shao R, Bilig H, Brännström M (2014) Pregnancy after allogeneic uterus transplantation in the rat: perinatal outcome and growth trajectory. Fertil Steril 102(6):1545–1552 e1541. https://doi.org/10.1016/j.fertnstert.2014.09.010
Tryphonopoulos P, Tzakis AG, Tekin A, Johannesson L, Rivas K, Morales PR, Wagner J, Mölne J, Enskog A, Diaz-Garcia C, Dahm-Kähler P, Berho M, Zimberg S, Falcone T, Ruiz P, Olausson M, Brännström M (2014) Allogeneic uterus transplantation in baboons: surgical technique and challenges to long-term graft survival. Transplantation 98(5):e51–56. https://doi.org/10.1097/TP.0000000000000322
Brännström M, Johannesson L, Dahm-Kähler P, Enskog A, Mölne J, Kvarnström N, Diaz-Garcia C, Hanafy A, Lundmark C, Marcickiewicz J, Gäbel M, Groth K, Akouri R, Eklind S, Holgersson J, Tzakis A, Olausson M (2014) First clinical uterus transplantation trial: a six-month report. Fertil Steril 101(5):1228–1236. https://doi.org/10.1016/j.fertnstert.2014.02.024
McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, Nicholl J, Balliol C, Aronson JK, Barkun JS, Blazeby JM, Boutron IC, Campbell WB, Clavien PA, Cook JA, Ergina PL, Feldman LS, Flum DR, Maddern GJ, Nicholl J, Reeves BC, Seiler CM, Strasberg SM, Meakins JL, Ashby D, Black N, Bunker J, Burton M, Campbell M, Chalkidou K, Chalmers I, de Leval M, Deeks J, Ergina PL, Grant A, Gray M, Greenhalgh R, Jenicek M, Kehoe S, Lilford R, Littlejohns P, Loke Y, Madhock R, McPherson K, Meakins J, Rothwell P, Summerskill B, Taggart D, Tekkis P, Thompson M, Treasure T, Trohler U, Vandenbroucke J (2009) No surgical innovation without evaluation: the IDEAL recommendations. Lancet 374(9695):1105–1112. https://doi.org/10.1016/S0140-6736(09)61116-8
Brännström M, Johannesson L, Bokstrom H, Kvarnström N, Mölne J, Dahm-Kähler P, Enskog A, Milenkovic M, Ekberg J, Diaz-Garcia C, Gäbel M, Hanafy A, Hagberg H, Olausson M, Nilsson L (2015) Livebirth after uterus transplantation. Lancet 385(9968):607–616. https://doi.org/10.1016/S0140-6736(14)61728-1
Brännström M, Bokström H, Dahm-Kähler P, Diaz-Garcia C, Ekberg J, Enskog A, Hagberg H, Johannesson L, Kvarnström N, Mölne J, Olausson M, Olofsson JI, Rodriguez-Wallberg K (2016) One uterus bridging three generations: first live birth after mother-to-daughter uterus transplantation. Fertil Steril 106(2):261–266. https://doi.org/10.1016/j.fertnstert.2016.04.001
Mölne J, Broecker V, Ekberg J, Nilsson O, Dahm-Kähler P, Brännström M (2016) Monitoring of human uterus transplantation with cervical biopsies: a provisional scoring system for rejection. Am J Transplant. https://doi.org/10.1111/ajt.14135
Brännström M (2015) The Swedish uterus transplantation project: the story behind the Swedish uterus transplantation project. Acta Obstet Gynecol Scand 94(7):675–679. https://doi.org/10.1111/aogs.12661
Brännström M (2015) Uterus transplantation. Curr Opin Organ Transplant 20(6):621–628. https://doi.org/10.1097/MOT.0000000000000246
Testa G, Koon EC, Johannesson L (2017) Living donor uterus transplant and surrogacy: ethical analysis according to the principle of equipoise. Am J Transplant 17(4):912–916. https://doi.org/10.1111/ajt.14086
Nadalin S, Capobianco I, Königsrainer I, Harder B, Königsrainer A (2015) Living liver donor: indications and technical aspects. Chirurg 86(6):609–621. https://doi.org/10.1007/s00104-015-0017-9
Järvholm S, Johannesson L, Brannström M (2015) Psychological aspects in pre-transplantation assessments of patients prior to entering the first uterus transplantation trial. Acta Obstet Gynecol Scand 94(10):1035–1038. https://doi.org/10.1111/aogs.12696
Brucker SY, Gegusch M, Zubke W, Rall K, Gauwerky JF, Wallwiener D (2008) Neovagina creation in vaginal agenesis: development of a new laparoscopic Vecchietti-based procedure and optimized instruments in a prospective comparative interventional study in 101 patients. Fertil Steril 90(5):1940–1952. https://doi.org/10.1016/j.fertnstert.2007.08.070
Flyckt RL, Farrell RM, Perni UC, Tzakis AG, Falcone T (2016) Deceased donor uterine transplantation: innovation and adaptation. Obstet Gynecol 128(4):837–842. https://doi.org/10.1097/AOG.0000000000001617
Erman Akar M, Ozkan O, Aydinuraz B, Dirican K, Cincik M, Mendilcioglu I, Simsek M, Gunseren F, Kocak H, Ciftcioglu A, Gecici O, Ozkan O (2013) Clinical pregnancy after uterus transplantation. Fertil Steril 100(5):1358–1363. https://doi.org/10.1016/j.fertnstert.2013.06.027
Fageeh W, Raffa H, Jabbad H, Marzouki A (2002) Transplantation of the human uterus. Int J Gynaecol Obstet 76(3):245–251
Testa G, Koon EC, Johannesson L, McKenna GJ, Anthony T, Klintmalm GB, Gunby RT, Warren AM, Putman JM, dePrisco G, Mitchell JM, Wallis K, Olausson M (2017) Living donor uterus transplantation: a single center’s observations and lessons learned from early setbacks to technical success. Am J Transplant. https://doi.org/10.1111/ajt.14326
Arnal JF, Laurell H, Fontaine C, Billon A, Calippe B, Lenfant F, Gourdy P (2009) Estrogen receptor actions on vascular biology and inflammation: implications in vascular pathophysiology. Climacteric 12(Suppl 1):12–17
Hodis HN, Mack WJ (2014) Hormone replacement therapy and the association with coronary heart disease and overall mortality: clinical application of the timing hypothesis. J Steroid Biochem Mol Biol 142:68–75. https://doi.org/10.1016/j.jsbmb.2013.06.011
Rhee SY, Kim YS (2015) Peripheral arterial disease in patients with type 2 diabetes mellitus. Diabetes Metab J 39(4):283–290. https://doi.org/10.4093/dmj.2015.39.4.283
Cheezum MK, Kim A, Bittencourt MS, Kassop D, Nissen A, Thomas DM, Nguyen B, Glynn RJ, Shah NR, Villines TC (2017) Association of tobacco use and cessation with coronary atherosclerosis. Atherosclerosis 257:201–207. https://doi.org/10.1016/j.atherosclerosis.2016.11.016
Bohlin KS, Ankardal M, Stjerndahl JH, Lindkvist H, Milsom I (2016) Influence of the modifiable life-style factors Body Mass Index and smoking on the outcome of hysterectomy. Acta Obstet Gynecol Scand 95(1):65–73. https://doi.org/10.1111/aogs.12794
Kahn J, Grupp U, Rotzinger R, Kaul D, Schäfer ML, Streitparth F (2014) CT for evaluation of potential renal donors—how does iterative reconstruction influence image quality and dose? Eur J Radiol 83(8):1332–1336. https://doi.org/10.1016/j.ejrad.2014.05.004
Borell U, Fernström I, Westman A (1953) Hormonal influence on the uterine arteries; an arteriographic study in the human. Acta Obstet Gynecol Scand 32(3):271–284
Hugues C, Le Bras Y, Coatleven F, Brun JL, Trillaud H, Grenier N, Cornelis F (2015) Vascular uterine abnormalities: comparison of imaging findings and clinical outcomes. Eur J Radiol 84(12):2485–2491. https://doi.org/10.1016/j.ejrad.2015.10.005
Author information
Authors and Affiliations
Contributions
SYB: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. MB: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. FAT: data collection or management, data analysis, and manuscript writing/editing. KR: data collection or management, data analysis, and manuscript writing/editing. KN: data collection or management, and manuscript writing/editing. MN: data collection or management, and manuscript writing/editing. NK: data collection or management, and manuscript writing/editing. PD-K: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. DW: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. All other authors: performance of the research and critical revision of the draft manuscript. All authors: final approval of the manuscript version to be published.
Corresponding author
Ethics declarations
Funding
There was no funding for the present work.
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. All patients gave their written informed consent for publication.
Rights and permissions
About this article
Cite this article
Brucker, S.Y., Brännström, M., Taran, FA. et al. Selecting living donors for uterus transplantation: lessons learned from two transplantations resulting in menstrual functionality and another attempt, aborted after organ retrieval. Arch Gynecol Obstet 297, 675–684 (2018). https://doi.org/10.1007/s00404-017-4626-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4626-z