Abstract
Purpose
The prognostic value and clinicopathological significance of CD44 in ovarian cancer (OC) remain unclear. This meta-analysis, therefore, aims to evaluate the correlation between CD44 expression and OC.
Methods
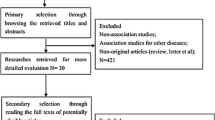
Studies published until March 2016 were searched in PubMed, EMBASE, and ISI Web of Knowledge databases. The odds ratio (OR) and the hazard ratio (HR) with 95 % confidence interval (CI) were used to assess the effects.
Results
Twenty-four studies that include 2267 OC patients were identified for the final analysis. Sixteen studies investigated the expression difference of CD44 standard (CD44s) in 1848 patients. Results showed that high CD44s expression is associated with chemoresistance (OR 5.94, 95 % CI 1.91–18.47) and short disease-free survival (DFS) time (HR 2.57, 95 % CI 1.34–4.91). In addition, CD44s expression is not associated with tumor differentiation grade, residual mass, lymphoid nodal metastasis, and overall survival (OS). Ten studies investigated the expression difference of CD44v6 in 724 patients. Results showed that the CD44v6 expression is not correlated with FIGO stage, tumor differentiation grade, lymphoid nodal metastasis, and OS.
Conclusion
High CD44s expression possibly indicates poor prognosis in OC patients given that high CD44s expression initiates chemotherapy resistance, although this expression pattern is not an independent predictive factor for OS. Meanwhile, high CD44s expression may be related to poor DFS of OC, but this relationship must be further confirmed. In addition, the result in which CD44v6 is not associated with OS of OC patients should be interpreted with caution.





Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1):7–30. doi:10.3322/caac.21332
Kipps E, Tan DS, Kaye SB (2013) Meeting the challenge of ascites in ovarian cancer: new avenues for therapy and research. Nat Rev Cancer 13(4):273–282. doi:10.1038/nrc3432
Winter WE 3rd, Maxwell GL, Tian C, Carlson JW, Ozols RF, Rose PG, Markman M, Armstrong DK, Muggia F, McGuire WP, Gynecologic Oncology Group S (2007) Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol Off J Am Soc Clin Oncol 25(24):3621–3627. doi:10.1200/JCO.2006.10.2517
Winter WE 3rd, Maxwell GL, Tian C, Sundborg MJ, Rose GS, Rose PG, Rubin SC, Muggia F, McGuire WP, Gynecologic Oncology G (2008) Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol Off J Am Soc Clin Oncol 26(1):83–89. doi:10.1200/JCO.2007.13.1953
Bogush TA, Popova AS, Dudko EA, Bogush EA, Tyulyandina AS, Tyulyandin SA, Davydov MI (2015) ERCC1 as a marker of ovarian cancer resistance to platinum drugs. Antibiot Khimioterapiia Antibiot Chemoterapy [sic]/Minist Med Mikrobiol Prom SSSR 60(3–4):42–50
Kim TH, Lee HH, Hwang JY, Kim JH, Jang WC, Lee A (2014) Genetic alteration in ovarian cancer. Arch Gynecol Obstet 290(5):827–830. doi:10.1007/s00404-014-3392-4
Rahman M, Deleyrolle L, Vedam-Mai V, Azari H, Abd-El-Barr M, Reynolds BA (2011) The cancer stem cell hypothesis: failures and pitfalls. Neurosurgery 68(2):531–545. doi:10.1227/NEU.0b013e3181ff9eb5 (discussion 545)
Jordan CT, Guzman ML, Noble M (2006) Cancer stem cells. N Engl J Med 355(12):1253–1261. doi:10.1056/NEJMra061808
Nguyen LV, Vanner R, Dirks P, Eaves CJ (2012) Cancer stem cells: an evolving concept. Nat Rev Cancer 12(2):133–143. doi:10.1038/nrc3184
Zoller M (2011) CD44: can a cancer-initiating cell profit from an abundantly expressed molecule? Nat Rev Cancer 11(4):254–267. doi:10.1038/nrc3023
Naor D, Sionov RV, Ish-Shalom D (1997) CD44: structure, function, and association with the malignant process. Adv Cancer Res 71:241–319
Volz Y, Koschut D, Matzke-Ogi A, Dietz MS, Karathanasis C, Richert L, Wagner MG, Mely Y, Heilemann M, Niemann HH, Orian-Rousseau V (2015) Direct binding of hepatocyte growth factor and vascular endothelial growth factor to CD44v6. Biosci Rep 35(4):e00236. doi:10.1042/BSR20150093
Preca BT, Bajdak K, Mock K, Sundararajan V, Pfannstiel J, Maurer J, Wellner U, Hopt UT, Brummer T, Brabletz S, Brabletz T, Stemmler MP (2015) A self-enforcing CD44s/ZEB1 feedback loop maintains EMT and stemness properties in cancer cells. Int J Cancer J Int Cancer 137(11):2566–2577. doi:10.1002/ijc.29642
Wu Y, Li Z, Zhang C, Yu K, Teng Z, Zheng G, Wang S, Liu Y, Cui L, Yu X (2015) CD44 family proteins in gastric cancer: a meta-analysis and narrative review. Int J Clin Exp Med 8(3):3595–3606
Li X, Ma X, Chen L, Gu L, Zhang Y, Zhang F, Ouyang Y, Gao Y, Huang Q, Zhang X (2015) Prognostic value of CD44 expression in renal cell carcinoma: a systematic review and meta-analysis. Sci Rep 5:13157. doi:10.1038/srep13157
Hu B, Luo W, Hu RT, Zhou Y, Qin SY, Jiang HX (2015) Meta-analysis of prognostic and clinical significance of CD44v6 in esophageal cancer. Medicine 94(31):e1238. doi:10.1097/MD.0000000000001238
Wojciechowski M, Krawczyk T, Smigielski J, Malinowski A (2015) CD44 expression in curettage and postoperative specimens of endometrial cancer. Arch Gynecol Obstet 291(2):383–390. doi:10.1007/s00404-014-3407-1
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16. doi:10.1186/1745-6215-8-16
Yorishima T, Nagai N, Ohama K (1997) Expression of CD44 alternative splicing variants in primary and lymph node metastatic lesions of gynecological cancer. Hiroshima J Med Sci 46(1):21–29
Darai E, Walker-Combrouze F, Fauconnier A, Madelenat P, Potet F, Scoazec JY (1998) Analysis of CD44 expression in serous and mucinous borderline tumours of the ovary: comparison with cystadenomas and overt carcinomas. Histopathology 32(2):151–159
Kayastha S, Freedman AN, Piver MS, Mukkamalla J, Romero-Guittierez M, Werness BA (1999) Expression of the hyaluronan receptor, CD44S, in epithelial ovarian cancer is an independent predictor of survival. Clin Cancer Res Off J Am Assoc Cancer Res 5(5):1073–1076
Saegusa M, Machida D, Hashimura M, Okayasu I (1999) CD44 expression in benign, premalignant, and malignant ovarian neoplasms: relation to tumour development and progression. J Pathol 189(3):326–337. doi:10.1002/(SICI)1096-9896(199911)189:3<326:AID-PATH425>3.0.CO;2-6
Schroder W, Rudlowski C, Biesterfeld S, Knobloch C, Hauptmann S, Rath W (1999) Expression of CD44(v5-10) splicing variants in primary ovarian cancer and lymph node metastases. Anticancer Res 19(5B):3901–3906
Afify AM, Ferguson AW, Davila RM, Werness BA (2001) Expression of CD44S and CD44v5 is more common in stage III than in stage I serous ovarian carcinomas. Appl Immunohistochem Mol Morphol AIMM/Off Publ Soc Appl Immunohistochem 9(4):309–314
Ross JS, Sheehan CE, Williams SS, Malfetano JH, Szyfelbein WM, Kallakury BV (2001) Decreased CD44 standard form expression correlates with prognostic variables in ovarian carcinomas. Am J Clin Pathol 116(1):122–128. doi:10.1309/KUK0-1M3D-LGNE-THXR
Rodriguez-Rodriguez L, Sancho-Torres I, Mesonero C, Gibbon DG, Shih WJ, Zotalis G (2003) The CD44 receptor is a molecular predictor of survival in ovarian cancer. Med Oncol 20(3):255–263. doi:10.1385/MO:20:3:255
Sillanpaa S, Anttila MA, Voutilainen K, Tammi RH, Tammi MI, Saarikoski SV, Kosma VM (2003) CD44 expression indicates favorable prognosis in epithelial ovarian cancer. Clinical Cancer Res Off J Am Assoc Cancer Res 9(14):5318–5324
Qu JY, Li S, Lin H, Wu JB, Wang YQ (2004) Relationship between expression of hyaluronan and pathologic features of ovarian adenocarcinoma. Ai zheng Aizheng Chin J Cancer 23(2):177–180
Zagorianakou N, Stefanou D, Makrydimas G, Zagorianakou P, Briasoulis E, Karavasilis B, Agnantis NJ (2004) CD44s expression, in benign, borderline and malignant tumors of ovarian surface epithelium. Correlation with p53, steroid receptor status, proliferative indices (PCNA, MIB1) and survival. Anticancer Res 24(3a):1665–1670
Hong SC, Song JY, Lee JK, Lee NW, Kim SH, Yeom BW, Lee KW (2006) Significance of CD44v6 expression in gynecologic malignancies. J Obstet Gynaecol Res 32(4):379–386. doi:10.1111/j.1447-0756.2006.00422.x
Steffensen KD, Alvero AB, Yang Y, Waldstrom M, Hui P, Holmberg JC, Silasi DA, Jakobsen A, Rutherford T, Mor G (2011) Prevalence of epithelial ovarian cancer stem cells correlates with recurrence in early-stage ovarian cancer. J Oncol 2011:620523. doi:10.1155/2011/620523
Zhou DX, Liu YX, Xue YH (2012) Expression of CD44v6 and Its Association with Prognosis in Epithelial Ovarian Carcinomas. Pathol Res Int 2012:908206. doi:10.1155/2012/908206
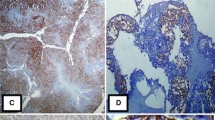
Hu Z, Gao J, Zhang D, Liu Q, Yan L, Gao L, Liu J, Liu D, Zhang S, Lin B (2013) High expression of Lewis y antigen and CD44 is correlated with resistance to chemotherapy in epithelial ovarian cancers. PLoS One 8(2):e57250. doi:10.1371/journal.pone.0057250
Shi J, Zhou Z, Di W, Li N (2013) Correlation of CD44v6 expression with ovarian cancer progression and recurrence. BMC Cancer 13:182. doi:10.1186/1471-2407-13-182
Ryabtseva OD, Lukianova NY, Shmurakov YA, Polishchuk LZ, Antipova SV (2013) Significance of adhesion molecules expression for estimation of serous ovarian cancer prognosis. Exp Oncol 35(3):211–218
Zhang J, Chang B, Liu J (2013) CD44 standard form expression is correlated with high-grade and advanced-stage ovarian carcinoma but not prognosis. Hum Pathol 44(9):1882–1889. doi:10.1016/j.humpath.2013.02.016
Wang A, Lu L, Wang Y, Sun Y, Zhang Y, Guo C, Gu Y, Liu A (2014) Expression and clinicopathologic significance of CD44v6/CD24 in ovarian serous carcinomas. Zhonghua bing li xue za zhi Chin J Pathol 43(1):20–24
Wang H, Tan M, Zhang S, Li X, Gao J, Zhang D, Hao Y, Gao S, Liu J, Lin B (2015) Expression and significance of CD44, CD47 and c-met in ovarian clear cell carcinoma. Int J Mol Sci 16(2):3391–3404. doi:10.3390/ijms16023391
Tjhay F, Motohara T, Tayama S, Narantuya D, Fujimoto K, Guo J, Sakaguchi I, Honda R, Tashiro H, Katabuchi H (2015) CD44 variant 6 is correlated with peritoneal dissemination and poor prognosis in patients with advanced epithelial ovarian cancer. Cancer Sci 106(10):1421–1428. doi:10.1111/cas.12765
Zhu LC, Gao J, Hu ZH, Schwab CL, Zhuang HY, Tan MZ, Yan LM, Liu JJ, Zhang DY, Lin B (2015) Membranous expressions of Lewis y and CAM-DR-related markers are independent factors of chemotherapy resistance and poor prognosis in epithelial ovarian cancer. Am J Cancer Res 5(2):830–843
Bonneau C, Rouzier R, Geyl C, Cortez A, Castela M, Lis R, Darai E, Touboul C (2015) Predictive markers of chemoresistance in advanced stages epithelial ovarian carcinoma. Gynecol Oncol 136(1):112–120. doi:10.1016/j.ygyno.2014.10.024
Elzarkaa AA, Sabaa BE, Abdelkhalik D, Mansour H, Melis M, Shaalan W, Farouk M, Malik E, Soliman AA (2016) Clinical relevance of CD44 surface expression in advanced stage serous epithelial ovarian cancer: a prospective study. J Cancer Res Clin Oncol. doi:10.1007/s00432-016-2116-5
Nagano O, Saya H (2004) Mechanism and biological significance of CD44 cleavage. Cancer Sci 95(12):930–935
Toole BP (2004) Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer 4(7):528–539. doi:10.1038/nrc1391
Lundell BI, McCarthy JB, Kovach NL, Verfaillie CM (1997) Activation of beta1 integrins on CML progenitors reveals cooperation between beta1 integrins and CD44 in the regulation of adhesion and proliferation. Leukemia 11(6):822–829
Lesley J, English NM, Gal I, Mikecz K, Day AJ, Hyman R (2002) Hyaluronan binding properties of a CD44 chimera containing the link module of TSG-6. J Biol Chem 277(29):26600–26608. doi:10.1074/jbc.M201068200
Fehon RG, McClatchey AI, Bretscher A (2010) Organizing the cell cortex: the role of ERM proteins. Nat Rev Mol Cell Biol 11(4):276–287. doi:10.1038/nrm2866
Mashayekhi F, Aryaee H, Mirzajani E, Yasin AA, Fathi A (2015) Soluble CD44 concentration in the serum and peritoneal fluid samples of patients with different stages of endometriosis. Arch Gynecol Obstet 292(3):641–645. doi:10.1007/s00404-015-3654-9
Xu H, Tian Y, Yuan X, Liu Y, Wu H, Liu Q, Wu GS, Wu K (2016) Enrichment of CD44 in basal-type breast cancer correlates with EMT, cancer stem cell gene profile, and prognosis. OncoTargets Ther 9:431–444. doi:10.2147/OTT.S97192
Liu Y, Wu Y, Gu S, Sun Z, Rui Y, Wang J, Lu Y, Li H, Xu K, Sheng P (2014) Prognostic role of CD44 expression in osteosarcoma: evidence from six studies. Diagn Pathol 9:140. doi:10.1186/1746-1596-9-140
Morrison R, Schleicher SM, Sun Y, Niermann KJ, Kim S, Spratt DE, Chung CH, Lu B (2011) Targeting the mechanisms of resistance to chemotherapy and radiotherapy with the cancer stem cell hypothesis. J Oncol 2011:941876. doi:10.1155/2011/941876
Acknowledgments
This study was funded by the National Natural Science Foundation of China (Grant Number: 81571411).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
L. Zhao and C. Gu contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
404_2016_4137_MOESM2_ESM.tif
Supplementary material 2 (TIFF 3783 kb) Supplementary Fig. 1 Forest plots showing the association between CD44s expression and clinicopathological parameters of patients with ovarian cancer. “a” represents CD44s expression and FIGO stage; “b” represents CD44s expression and tumor differentiation grade; “c” represents CD44s expression and tumor residual mass; “d” represents CD44s expression and lymphoid nodal metastasis; “e” represents CD44s expression and recurrence
404_2016_4137_MOESM3_ESM.tif
Supplementary material 3 (TIFF 1925 kb) Supplementary Fig. 2 Forest plots showing the association between CD44v6 expression and clinicopathological parameters of patients with ovarian cancer. “a” represents CD44v6 expression and FIGO stage; “b” represents CD44v6 expression and tumor differentiation grade; “c” represents CD44v6 expression and lymphoid nodal metastasis
404_2016_4137_MOESM4_ESM.tif
Supplementary material 4 (TIFF 1811 kb) Supplementary Fig. 3 Forest plots showing the association of CD44 expression and OS of patients with ovarian cancer. “a” represents CD44s expression and OS; “b” represents CD44v6 expression and OS
Rights and permissions
About this article
Cite this article
Zhao, L., Gu, C., Huang, K. et al. The prognostic value and clinicopathological significance of CD44 expression in ovarian cancer: a meta-analysis. Arch Gynecol Obstet 294, 1019–1029 (2016). https://doi.org/10.1007/s00404-016-4137-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4137-3