Abstract
Purpose
The physiological changes during pregnancy can significantly alter antiepileptic drug (AED)’s absorption, distribution, metabolism and elimination, thus influencing their plasma concentration. Considering that the risks of using old and new AEDs during pregnancy are still debated, our aim is to review the available evidence on this topic.
Methods
Narrative overview, synthesizing the findings of literature retrieved from searches of computerized databases.
Results
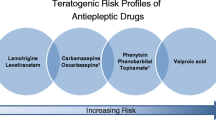
The old AEDs generation (benzodiazepines, phenytoin, carbamazepine, phenobarbital and valproic acid) is teratogenic: minor congenital malformations, such as facial dysmorphism and other anomalies, occur in 6–20 % of infants exposed to AEDs in utero; this value is two times greater than the value reported in the general population. Major congenital malformations (MCM) such as cleft lip and cleft palate, heart defects (atrial septal defect, Fallot’s tetralogy, ventricular septal defect, aortic coarctation, patent ductus arteriosus, and pulmonary stenosis) and urogenital anomalies were estimated to be 4–6 % of infants born from mothers treated with AEDs, compared to 2–3 % of the general population.
Conclusion
It is essential to inform women treated with AED that planning pregnancy is necessary, when possible. The problems related to antiepileptic therapy and the possibilities of prenatal diagnosis should be accurately discussed with the patient, when possible before pregnancy: individual circumstances, desire to have children, severity of epilepsy, risks of seizures, family history of congenital malformations and all other potential risk factors must be considered, involving the patient in shared clinical decision-making.


Similar content being viewed by others
References
Care NCC for P (2004) The diagnosis and management of the epilepsies in adults and children in primary and secondary care
Ngugi AK, Kariuki SM, Bottomley C et al (2011) Incidence of epilepsy: a systematic review and meta-analysis. Neurology 77:1005–1012. doi:10.1212/WNL.0b013e31822cfc90
Hirtz D, Thurman DJ, Gwinn-Hardy K et al (2007) How common are the “common” neurologic disorders? Neurology 68:326–337. doi:10.1212/01.wnl.0000252807.38124.a3
Maiga Y, Napon C, Kuate Tegueu C et al (2010) Epilepsy and women’s life: particularities of their management. Literature review. Mali Med 25:1–9
Fisher RS, Van Emde Boas W, Blume W et al (2005) Epileptic seizures and epilepsy: definitions proposed by the international league against epilepsy (ILAE) and the international bureau for epilepsy (IBE). Epilepsia 46:470–472. doi:10.1111/j.0013-9580.2005.66104.x
Hauser WA, Annegers JF, Rocca WA (1996) Descriptive epidemiology of epilepsy: contributions of population-based studies from Rochester, Minnesota. Mayo Clin Proc 71:576–586. doi:10.4065/71.6.576
Berg AT, Shinnar S (1991) The risk of seizure recurrence following a first unprovoked seizure: a quantitative review. Neurology 41:965–972. doi:10.1212/WNL.41.7.965
Hauser WA, Rich SS, Lee JR et al (1998) Risk of recurrent seizures after two unprovoked seizures. N Engl J Med 338:429–434. doi:10.1097/00007611-199806000-00028
Robson S, Hunter S, Boys R, Dunlop W (1989) Serial study of factors influencing changes in cardiac output during human pregnancy. Am J Physiol 256:H1060–H1065
Clark SL, Cotton DB, Lee W et al (1989) Central hemodynamic assessment of normal term pregnancy. Am J Obstet Gynecol 161:1439–1442. doi:10.1097/00132586-199102000-00026
Messmer K, Kemming G (2006) Clinical hemodilution. Blood Substit. pp 178–187
American College of Obstetricians and Gynecologists (2008) ACOG practice bulletin no. 95: anemia in pregnancy. Obs Gynecol 112:201–207. doi:10.1097/AOG.0b013e3181809c0d
Davison JM, Dunlop W (1980) Renal hemodynamics and tubular function in normal human pregnancy. Kidney Int 18:152–161
Hegewald MJ, Crapo RO (2011) Respiratory physiology in pregnancy. Clin Chest Med 32:1–13. doi:10.1016/j.ccm.2010.11.001
McAuliffe F, Kametas N, Costello J et al (2002) Respiratory function in singleton and twin pregnancy. BJOG Int J Obstet Gynaecol 109:765–769. doi:10.1111/j.1471-0528.2002.01515.x
Fisher RS, Roberts GS, Grabowski CJ, Cohen S (1978) Altered lower esophageal sphincter function during early pregnancy. Gastroenterology 74:1233–1237
Vellacott ID, Cooke EJ, James CE (1988) Nausea and vomiting in early pregnancy. Int J Gynaecol Obstet 27:57–62. doi:10.1016/0020-7292(88)90088-4
Parry E, Shields R, Turnbull AC (1970) The effect of pregnancy on the colonic absorption of sodium, potassium and water. J Obstet Gynaecol Br Commonw 77:616–619. doi:10.1111/j.1471-0528.1970.tb03579.x
Everson GT (1998) Liver problems in pregnancy: distinguishing normal from abnormal hepatic changes. Medscape Womens Health 3:3
Celik H, Tosun M, Cetinkaya MB et al (2009) Markedly elevated serum alkaline phosphatase level in an uncomplicated pregnancy. J Matern Fetal Neonatal Med 22:705–707. doi:10.1080/14767050802702323
Chrousos GP (1995) The hypothalamic-pituitary-adrenal axis and immune-mediated inflammation. N Engl J Med 332:1351–1362. doi:10.1056/NEJM199505183322008
Petraglia F, Potter E, Cameron VA et al (1993) Corticotropin-releasing factor-binding protein is produced by human placenta and intrauterine tissues. J Clin Endocrinol Metab 77:919–924
Petraglia F, Florio P, Nappi C, Genazzani AR (1996) Peptide signaling in human placenta and membranes: autocrine, paracrine, and endocrine mechanisms. Endocr Rev 17:156–186. doi:10.1210/er.17.2.156
Borthen I, Eide MG, Veiby G et al (2009) Complications during pregnancy in women with epilepsy: population-based cohort study. BJOG Int J Obstet Gynaecol 116:1736–1742. doi:10.1111/j.1471-0528.2009.02354.x
Rating D, Nau H, Jäger-Roman E et al (1982) Teratogenic and pharmacokinetic studies of primidone during pregnancy and in the offspring of epileptic women. Acta Paediatr Scand 71:301–311
Teramo K, Hiilesmaa V, Bardy A, Saarikoski S (1979) Fetal heart rate during a maternal grand mal epileptic seizure. J Perinat Med 7:3–6. doi:10.1515/jpme.1979.7.1.3
Bardy AH, Hiilesmaa VK, Teramo K, Granström ML (1981) Teratogenic risks of antiepileptic drugs. Br Med J (Clin Res Ed) 283:1405–1406. doi:10.1136/bmj.283.6303.1405-d
Battino D, Tomson T, Bonizzoni E et al (2013) Seizure control and treatment changes in pregnancy: observations from the EURAP epilepsy pregnancy registry. Epilepsia 54:1621–1627. doi:10.1111/epi.12302
Olafsson E, Hallgrimsson JT, Hauser WA et al (1998) Pregnancies of women with epilepsy: a population-based study in Iceland. Epilepsia 39:887–892
Richmond JR, Krishnamoorthy P, Andermann E, Benjamin A (2004) Epilepsy and pregnancy: an obstetric perspective. Am J Obstet Gynecol 190:371–379. doi:10.1016/j.ajog.2003.09.020
Borthen I, Eide MG, Daltveit AK, Gilhus NE (2011) Obstetric outcome in women with epilepsy: a hospital-based, retrospective study. BJOG Int J Obstet Gynaecol 118:956–965. doi:10.1111/j.1471-0528.2011.03004.x
Harden CL, Meador KJ, Pennell PB et al (2009) Management issues for women with epilepsy-focus on pregnancy (an evidence-based review): II. Teratogenesis and perinatal outcomes. Epilepsia 50:1237–1246. doi:10.1111/j.1528-1167.2009.02128.x
Kelly VM, Nelson LM, Chakravarty EF (2009) Obstetric outcomes in women with multiple sclerosis and epilepsy. Neurology 73:1831–1836. doi:10.1212/WNL.0b013e3181c3f27d
Veiby G, Daltveit AK, Engelsen BA, Gilhus NE (2009) Pregnancy, delivery, and outcome for the child in maternal epilepsy. Epilepsia 50:2130–2139. doi:10.1111/j.1528-1167.2009.02147.x
Viinikainen K, Heinonen S, Eriksson K, Kälviäinen R (2006) Community-based, prospective, controlled study of obstetric and neonatal outcome of 179 pregnancies in women with epilepsy. Epilepsia 47:186–192. doi:10.1111/j.1528-1167.2006.00386.x
Hvas CL, Henriksen TB, Ostergaard JR, Dam M (2000) Epilepsy and pregnancy: effect of antiepileptic drugs and lifestyle on birthweight. BJOG 107:896–902
Gerli S, Favilli A, Giordano C et al (2013) Single indications of induction of labor with prostaglandins and risk of cesarean delivery: a retrospective cohort study. J Obstet Gynaecol Res 39:926–931. doi:10.1111/jog.12000
Favilli A, Acanfora MM, Bini V et al (2013) Single indication of labor induction with prostaglandins: is advanced maternal age a risk factor for cesarean section? A matched retrospective cohort study. J Matern Fetal Neonatal Med 26:665–668. doi:10.3109/14767058.2012.746658
Zahn CA, Morrell MJ, Collins SD et al (1998) Management issues for women with epilepsy: a review of the literature. Neurology 51:949–956. doi:10.1212/WNL.51.4.949
Lundgren EM, Tuvemo T (2008) Effects of being born small for gestational age on long-term intellectual performance. Best Pract Res Clin Endocrinol Metab 22:477–488. doi:10.1016/j.beem.2008.01.014
Mawer G, Briggs M, Baker GA et al (2010) Pregnancy with epilepsy: obstetric and neonatal outcome of a controlled study. Seizure 19:112–119. doi:10.1016/j.seizure.2009.11.008
Meador KJ, Pennell PB, Harden CL et al (2008) Pregnancy registries in epilepsy: a consensus statement on health outcomes. Neurology 71:1109–1117. doi:10.1212/01.wnl.0000316199.92256.af
Patsalos PN, Berry DJ, Bourgeois BFD et al (2008) Antiepileptic drugs—best practice guidelines for therapeutic drug monitoring: a position paper by the subcommission on therapeutic drug monitoring, ILAE commission on therapeutic strategies. Epilepsia 49:1239–1276. doi:10.1111/j.1528-1167.2008.01561.x
Brodtkorb E, Reimers A (2008) Seizure control and pharmacokinetics of antiepileptic drugs in pregnant women with epilepsy. Seizure 17:160–165. doi:10.1016/j.seizure.2007.11.015
Pennell PB (2003) Antiepileptic drug pharmacokinetics during pregnancy and lactation. Neurology 61:S35–S42. doi:10.1212/WNL.61.6_suppl_2.S35
Battino D, Avanzini G, Bossi L et al (1983) Plasma levels of primidone and its metabolite phenobarbital: effect of age and associated therapy. Ther Drug Monit 5:73–79. doi:10.1097/00007691-198303000-00006
Costantine MM (2014) Physiologic and pharmacokinetic changes in pregnancy. Front Pharmacol. doi:10.3389/fphar.2014.00065
Reisinger TL, Newman M, Loring DW et al (2013) Antiepileptic drug clearance and seizure frequency during pregnancy in women with epilepsy. Epilepsy Behav 29:13–18. doi:10.1016/j.yebeh.2013.06.026
Morrell MJ, Giudice L, Flynn KL et al (2002) Predictors of ovulatory failure in women with epilepsy. Ann Neurol 52:704–711. doi:10.1002/ana.10391
Drislane FW, Coleman AE, Schomer DL et al (1994) Altered pulsatile secretion of luteinizing hormone in women with epilepsy. Neurology 44:306–310. doi:10.1212/WNL.44.2.306
Meo R, Bilo L, Nappi C et al (1993) Derangement of the hypothalamic GnRH pulse generator in women with epilepsy. Seizure 2:241–252. doi:10.1016/S1059-1311(05)80134-7
Murialdo G, Galimberti CA, Magri F et al (1997) Menstrual cycle and ovary alterations in women with epilepsy on antiepileptic therapy. J Endocrinol Invest 20:519–526
Verrotti A, D’Egidio C, Mohn A et al (2011) Antiepileptic drugs, sex hormones, and PCOS. Epilepsia 52:199–211. doi:10.1111/j.1528-1167.2010.02897.x
Herzog AG, Seibel MM, Schomer DL et al (1986) Reproductive endocrine disorders in men with partial seizures of temporal lobe origin. Arch Neurol 43:347–350. doi:10.1001/archneur.1986.00520040035015
Morrell MJ, Flynn KL, Seale CG et al (2001) Reproductive dysfunction in women with epilepsy: antiepileptic drug effects on sex-steroid hormones. CNS Spectr 6(771–772):783–786
Fenwick PB, Toone BK, Wheeler MJ et al (1985) Sexual behaviour in a centre for epilepsy. Acta Neurol Scand 71:428–435
Thomas SV, Nair RR, Jose M, Sarma PS (2009) Risk of major congenital malformations in the offsprings of women with epilepsy is not related to family history. Epilepsy Res 83:52–57. doi:10.1016/j.eplepsyres.2008.09.002
Wide K, Winbladh B, Källén B (2004) Major malformations in infants exposed to antiepileptic drugs in utero, with emphasis on carbamazepine and valproic acid: a nation-wide, population-based register study. Acta Paediatr 93:174–176. doi:10.1080/08035250310021118
Kelly TE (1984) Teratogenicity of anticonvulsant drugs. I: review of the literature. Am J Med Genet 19:413–434
Daly LE, Kirke PN, Molloy A et al (1995) Folate levels and neural tube defects. Implications for prevention. JAMA 274:1698–1702. doi:10.1001/jama.274.21.1698
Czeizel AE, Dudás I, Paput L, Bánhidy F (2011) Prevention of neural-tube defects with periconceptional folic acid, methylfolate, or multivitamins? Ann Nutr Metab 58:263–271. doi:10.1159/000330776
Kishi T, Fujita N, Eguchi TA, Ueda K (1997) Mechanism for reduction of serum folate by antiepileptic drugs during prolonged therapy. J Neurol Sci 145:109–112. doi:10.1016/S0022-510X(96)00256-0
Yoo JH, Hong SB (1999) A common mutation in the methylenetetrahydrofolate reductase gene is a determinant of hyperhomocysteinemia in epileptic patients receiving anticonvulsants. Metabolism 48:1047–1051. doi:10.1016/S0026-0495(99)90204-4
Verrotti A, Pascarella R, Trotta D et al (2000) Hyperhomocysteinemia in children treated with sodium valproate and carbamazepine. Epilepsy Res 41:253–257. doi:10.1016/S0920-1211(00)00150-9
Dean JC, Moore SJ, Osborne A et al (1999) Fetal anticonvulsant syndrome and mutation in the maternal MTHFR gene. Clin Genet 56:216–220. doi:10.1034/j.1399-0004.1999.560306.x
Gaily E, Granström ML, Hiilesmaa V, Bardy A (1988) Minor anomalies in offspring of epileptic mothers. J Pediatr 112:520–529
Koch S, Lösche G, Jager-Romän E et al (1992) Major and minor birth malformations and antiepileptic drugs. Neurology 42:83–88
Omtzigt JG, Los FJ, Grobbee DE et al (1992) The risk of spina bifida aperta after first-trimester exposure to valproate in a prenatal cohort. Neurology 42:119–125
Gilboa SM, Broussard CS, Devine OJ et al (2011) Influencing clinical practice regarding the use of antiepileptic medications during pregnancy: modeling the potential impact on the prevalences of spina bifida and cleft palate in the United States. Am J Med Genet Part C Semin Med Genet 157:234–246. doi:10.1002/ajmg.c.30306
Holmes LB, Harvey EA, Coull BA et al (2001) The teratogenicity of anticonvulsant drugs. N Engl J Med 344:1132–1138. doi:10.1097/00006254-200109000-00006
Matalon S, Schechtman S, Goldzweig G, Ornoy A (2002) The teratogenic effect of carbamazepine: a meta-analysis of 1255 exposures. Reprod Toxicol 16:9–17. doi:10.1016/S0890-6238(01)00199-X
Artama M, Auvinen A, Raudaskoski T et al (2005) Antiepileptic drug use of women with epilepsy and congenital malformations in offspring. Neurology 64:1874–1878. doi:10.1212/01.WNL.0000163771.96962.1F
Hernandez-Diaz S, Smith CR, Shen A et al (2011) Comparative safety of anticonvulsants during pregnancy: seizures or major malformations. Pharmacoepidemiol Drug Saf 20:S11
Hunt SJ, Craig JJ, Morrow JI (2009) Increased frequency of isolated cleft palate in infants exposed to lamotrigine during pregnancy. Neurology 72:1108. doi:10.1212/01.wnl.0000346463.44116.56
Holmes LB (2011) Controls for pregnancy registries. Birth Defects Res Part A Clin Mol Teratol 91:386
Tomson T, Perucca E, Battino D (2004) Navigating toward fetal and maternal health: the challenge of treating epilepsy in pregnancy. Epilepsia 45:1171–1175. doi:10.1111/j.0013-9580.2004.15104.x
Morrow JI, Russell AJ, Irwin B et al (2004) The safety of antiepileptic drugs in pregnancy: results of the UK epilepsy and pregnancy register. Epilepsia 45(Suppl 3):57
Dansky LV, Andermann E, Rosenblatt D, Sherwin AL (1987) Anticonvulsants, folate levels, and pregnancy outcome: a prospective study. Ann Neurol 21:176–182. doi:10.1002/ana.410210210
Cunnington MC, Weil JG, Messenheimer JA et al (2011) Final results from 18 years of the international lamotrigine pregnancy registry. Neurology 76:1817–1823. doi:10.1212/WNL.0b013e31821ccd18
Kaneko S, Battino D, Andermann E et al (1999) Congenital malformations due to antiepileptic drugs. Epilepsy Res 33:145–158. doi:10.1016/S0920-1211(98)00084-9
Kaaja E, Kaaja R, Hiilesmaa V (2003) Major malformations in offspring of women with epilepsy. Neurology 60:575–579. doi:10.1212/WNL.61.11.1631-a
Vajda FJE, Hitchcock A, Graham J et al (2006) Foetal malformations and seizure control: 52 months data of the Australian pregnancy registry. Eur J Neurol 13:645–654. doi:10.1111/j.1468-1331.2006.01359.x
Barrett C, Richens A (2003) Epilepsy and pregnancy: report of an epilepsy research foundation workshop. Epilepsy Res 52:147–187
Inoyama K, Meador KJ (2015) Cognitive outcomes of prenatal antiepileptic drug exposure. Epilepsy Res 114:89–97. doi:10.1016/j.eplepsyres.2015.04.016
Nakken KO, Lillestølen KM, Brodtkorb E et al (2014) Antiepileptika og medfødte misdannelser. Tidsskr den Nor Laegeforening 134:1239–1242. doi:10.4045/tidsskr.13.1349
Sabers A (2009) Influences on seizure activity in pregnant women with epilepsy. Epilepsy Behav 15:230–234. doi:10.1016/j.yebeh.2009.03.031
Hui ACF, Yeung HM (2001) Avoiding pitfalls in the management of epilepsy. Hong Kong Pract 23:246–250
Crawford P (2005) Best practice guidelines for the management of women with epilepsy. Epilepsia 46:117–124. doi:10.1111/j.1528-1167.2005.00323.x
Perucca E, Battino D, Tomson T (2014) Gender issues in antiepileptic drug treatment. Neurobiol Dis. doi:10.1016/j.nbd.2014.05.011
Bajcar JM, Kennie N, Einarson TR (2005) Collaborative medication management in a team-based primary care practice: an explanatory conceptual framework. Res Soc Adm Pharm 1:408–429. doi:10.1016/j.sapharm.2005.06.003
Nulman I, Laslo D, Koren G (1999) Treatment of epilepsy in pregnancy. Drugs 57:535–544. doi:10.2165/00003495-199957040-00006
Luef G (2009) Female issues in epilepsy: a critical review. Epilepsy Behav 15:78–82. doi:10.1016/j.yebeh.2009.02.023
Choulika S, Grabowski E, Holmes LB (2004) Is antenatal vitamin K prophylaxis needed for pregnant women taking anticonvulsants? Am J Obstet Gynecol 190:882–883. doi:10.1016/j.ajog.2004.01.041
Kaaja E, Kaaja R, Matila R, Hiilesmaa V (2002) Enzyme-inducing antiepileptic drugs in pregnancy and the risk of bleeding in the neonate. Neurology 58:549–553. doi:10.1212/WNL.58.4.549
Pack AM (2006) Therapy insight: clinical management of pregnant women with epilepsy. Nat Clin Pract Neurol 2:190–200. doi:10.1038/ncpneuro0153
Öhman I, Vitols S, Luef G et al (2002) Topiramate kinetics during delivery, lactation, and in the neonate: preliminary observations. Epilepsia 43:1157–1160. doi:10.1046/j.1528-1157.2002.12502.x
Johannessen SI, Helde G, Brodtkorb E (2005) Levetiracetam concentrations in serum and in breast milk at birth and during lactation. Epilepsia 46:775–777. doi:10.1111/j.1528-1167.2005.54804.x
Öhman I, Vitols S, Tomson T (2005) Pharmacokinetics of gabapentin during delivery, in the neonatal period, and lactation: does a fetal accumulation occur during pregnancy? Epilepsia 46:1621–1624. doi:10.1111/j.1528-1167.2005.00251.x
Pashley S, O’Donoghue MF (2009) The safety of anti-epileptic drug regimens: a qualitative study of factors determining the success of counselling women before conception. J Fam Plann Reprod Health Care 35:153–156. doi:10.1783/147118909788708002
McAuley JW, Patankar C, Lang C, Prasad M (2012) Evaluating the concerns of pregnant women with epilepsy: a focus group approach. Epilepsy Behav 24:246–248. doi:10.1016/j.yebeh.2012.03.014
Hart LA, Sibai BM (2013) Seizures in pregnancy: epilepsy, eclampsia, and stroke. Semin Perinatol 37:207–224. doi:10.1053/j.semperi.2013.04.001
Robinson JN, Cleary-Goldman J (2008) Chapter 16 management of epilepsy and pregnancy. An obstetrical perspective. Int Rev Neurobiol 83:273–282. doi:10.1016/S0074-7742(08)00016-0
Pickrell WO, Elwyn G, Smith PEM (2015) Shared decision-making in epilepsy management. Epilepsy Behav. doi:10.1016/j.yebeh.2015.01.033
Vitagliano A, Quaranta M, Noventa M, Gizzo S (2015) “Empiric” inositol supplementation in normal-weight non insulin resistant women with polycystic ovarian disease: from the absence of benefit to the potential adverse effects. Arch Gynecol Obstet 291:955–957. doi:10.1007/s00404-015-3662-9
Noventa M, Vitagliano A, Quaranta M et al (2015) Preventive and therapeutic role of dietary inositol supplementation in periconceptional period and during pregnancy: a summary of evidences and future applications. Reprod Sci. doi:10.1177/1933719115594018
Patrelli TS, Dall’Asta A, Gizzo S et al (2012) Calcium supplementation and prevention of preeclampsia: a meta-analysis. J Matern Neonatal Med 25:1–5. doi:10.3109/14767058.2012.715220
Cetin I, Berti C, Calabrese S (2009) Role of micronutrients in the periconceptional period. Hum Reprod Update 16:80–95. doi:10.1093/humupd/dmp025
Gizzo S, Patrelli TS, Rossanese M et al (2013) An update on diabetic women obstetrical outcomes linked to preconception and pregnancy glycemic profile: a systematic literature review. Sci World J 2013:254901. doi:10.1155/2013/254901
Gizzo S, Noventa M, Di Gangi S et al (2015) Could molecular assessment of calcium metabolism be a useful tool to early screen patients at risk for pre-eclampsia complicated pregnancy? Proposal and rationale. Clin Chem Lab Med 53:975–979. doi:10.1515/cclm-2014-0693
Gizzo S, Noventa M, Anis O et al (2014) Pharmacological anti-thrombotic prophylaxis after elective caesarean delivery in thrombophilia unscreened women: should maternal age have a role in decision making? J Perinat Med 42:339–347. doi:10.1515/jpm-2013-0160
Gizzo S, Patrelli TS, Di Gangi S et al (2013) Which uterotonic is better to prevent the postpartum hemorrhage? Latest news in terms of clinical efficacy, side effects, and contraindications: a systematic review. Reprod Sci 20:1011–1019. doi:10.1177/1933719112468951
Gizzo S, Noventa M, Fagherazzi S et al (2014) Update on best available options in obstetrics anaesthesia: perinatal outcomes, side effects and maternal satisfaction. Fifteen years systematic literature review. Arch Gynecol Obstet 290:21–34. doi:10.1007/s00404-014-3212-x
Gizzo S, Di Gangi S, Saccardi C et al (2012) Epidural analgesia during labor: impact on delivery outcome, neonatal well-being, and early breastfeeding. Breastfeed Med 7:262–268. doi:10.1089/bfm.2011.0099
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All Authors have no proprietary, financial, professional or other personal interest of any nature in any product, service or company. The Authors alone are responsible for the content and writing of the paper.
Rights and permissions
About this article
Cite this article
Laganà, A.S., Triolo, O., D’Amico, V. et al. Management of women with epilepsy: from preconception to post-partum. Arch Gynecol Obstet 293, 493–503 (2016). https://doi.org/10.1007/s00404-015-3968-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3968-7