Abstract
Purpose
To improve the outcome of fetuses with gastrochisis several studies evaluated prenatal predictors. But there are different guidelines established and therefore the prenatal care is not standardized. With our study we wanted to evaluate the outcome of fetuses with gastroschisis after modification of prenatal management strategies at the Department of Obstetrics and Gynecology of the University Hospital Münster.
Methods
In this explorative retrospective study of 39 fetuses with gastroschisis, we compare the clinical outcome between two management groups. In the first group (group 1, n = 14) prenatal indication for delivery was confirmed by a subjective evaluation of the small bowel diameter and the wall thickness without established cut-off values for these parameters. In the second group (group 2, n = 25) certain limits for the small bowel diameter (25 mm) and the wall thickness (2.5 mm) were used for fetal surveillance.
Results
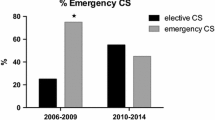
Noticeable differences between the two groups regarding birth weight, weight centile, arterial pH, small bowel diameter, wall thickness, adverse bowel condition and re-operations could not be observed. In group 2, delivery was earlier (p = 0.011), and a lower rate of prenatal complications was observed (p = 0.016).
Conclusion
To avoid adverse prenatal complications we recommend the observation of fetuses with gastroschisis by sonographic monitoring of the small bowel diameter and the wall thickness.

Similar content being viewed by others
References
Brown N, Nardi M, Greer RM, Petersen S, Thomas J, Gardener G et al (2014) Prenatal extra-abdominal bowel dilatation is a risk factor for intrapartum fetal compromise for fetuses with gastroschisis. Prenat Diagn. doi:10.1002/pd.4535 (Epub ahead of print)
Loane M, Dolk H, Bradbury I, EUROCAT Working Group (2007) Increasing prevalence of gastroschisis in Europe 1980–2002: a phenomenon restricted to younger mothers? Paediatr Perinat Epidemiol 21:363–369
Rasmussen SA, Frias JL (2008) Non-genetic risk factors for gastroschisis. Am J Med Genet C Semin Med Genet 15:199–212
Torfs CP, Velie EM, Oechsli FW, Bateson TF, Curry CJR (1994) A population based study of gastroschisis: demographic, pregnancy, and lifestyle risk factors. Teratology 50:44–53
Davis RP, Treadwell MC, Drongowski RA, Teitelbaum DH, Mychaliska GB (2009) Risk stratification in gastroschisis: can prenatal evaluation or early postnatal factors predict outcome? Pediatr Surg Int 25:319–325
Japaraj RP, Hockey R, Chan FY (2003) Gastroschisis: can prenatal sonography predict neonatal outcome? Ultrasound Obest Gynecol 21:329–333
Crawford RAF, Ryan G, Wright VM, Rodeck CH (1992) The importance of serial biophysical assessment of fetal wellbeing in gastroschisis. BJOG 99:899–902
Heinig J, Müller V, Schmitz R, Lohse K, Klockenbusch W, Steinhard J (2008) Sonographic assessment of the extra-abdominal fetal small bowel in gastroschisis: a retrospective longitudinal study in relation to prenatal complications. Prenat Diagn 28:109–114
Langer JC, Bell JG, Castillo RO, Crombleholme TM, Longaker MT, Duncan BW et al (1990) Etiology of intestinal damage in gastroschisis 2. Timing and reversibility of histological change, mucosal function, and contractility. J Pediatr Surg 25:1122–1126
Langer J, Khanna J, Caco C, Dykes EH, Nicolaides KH (1993) Prenatal diagnosis of gastroschisis: development of objective sonographic criteria for predicting outcome. Obstet Gynecol 81:53–54
Adra A, Landy H, Nahmias J, Gomez-Marin O (1996) The fetus with gastroschisis: impact of route of delivery and prenatal ultrasonography. Am J Obstet 174:540–546
Piper H, Jaksic (2006) The impact of prenatal bowel dilation on clinical outcomes in neonates with gastroschisis. J Pediatr Surg 41:897–900
Lato K, Poellmann M, Knippel AJ, Bizjak G, Stressig R, Hammer R et al (2013) Fetal gastroschisis: a comparison of second vs third-trimester bowel dilatation for predicting bowel atresia and neonatal outcomes. Ultraschall in Med 34(2):157–161
Kuleva M, Khen-Dunlop N, Dumez Y, Ville Y, Salomon LJ (2012) Is complex gastroschisis predictable by prenatal ultrasound?. BJOG 119:102–109
Durfee SM, Benson CB, Adams SR, Ecker J, House M, Jennings R et al (2013) Postnatal outcome of fetuses with the prenatal diagnosis of gastroschisis. J Ultrasound Med 32:407–412
Overton TG, Pierce MR, Gao H, Kurinczuk JJ, Spark P, Draper ES et al (2012) Antenatal management and outcome of gastroschisis in the UK. Prenat Diagn 32:1256–1262
Overcash RT, DeUgarte DA, Stephenson ML, Gutkin RM, Norton ME, Parmar S et al (2014) Factors associated with gastroschisis outcomes. Obstet Gynecol 124(3):551–557
Lepigeon K, Van Mieghem T, Vasseur Maurer S, Giannoni E, Baud D (2014) Gastroschisis—what should be told to parents? Prenat Diagn 34(4):316–326
Barseghyan K, Aghajanian P, Miller AD (2012) The prevalence of preterm births in pregnancies complicated with fetal gastroschisis. Arch Gynecol Obstet 286:889–892
Mesas Burgos C, Svenningsson A, Hammarqvist Vejde J, Granholm T, Connor P (2015) Outcomes in infants with prenatally diagnosed gastroschisis and planned preterm delivery. Pediatr Surg Int 31:1047–1053
R Core Team (2014) A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. www.R-project.org
Acknowledgments
None.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bauseler, A., Funke, K., Möllers, M. et al. Outcome of fetuses with gastroschisis after modification of prenatal management strategies. Arch Gynecol Obstet 294, 239–243 (2016). https://doi.org/10.1007/s00404-015-3961-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3961-1