Abstract
Purpose
Evaluation of the safety and efficacy of the use of polypropylene mesh for cystocele repair using minimally invasive technique.
Methods
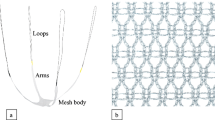
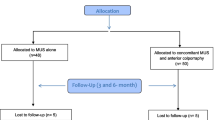
We retrospectively evaluated the perioperative events, short-term postoperative side-effects, and follow up for 152 patients who underwent repair for cystocele grade 2 or more using a polypropylene mesh. The repair was performed through a small anterior vaginal wall incision, with the arms of the mesh passed through a transobturator route using a corkscrew needle. Stress urinary incontinence (SUI) tests and the International Continence Society Pelvic Organ Prolapse Quantification (POP-Q) staging systems were documented before and after surgery.
Results
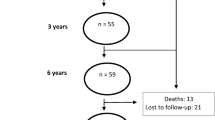
The average time and blood loss for the procedure were 18 min and 100 cc, respectively. Bladder injury and excess bleeding (>500 cc) occurred in one and two cases during the procedure, respectively. The early postoperative complications included pain (10.5 %), mesh erosion (1.3 %), fever (1.3 %), and urinary tract infection (7.9 %). Among the 122 patients who were followed up (median follow-up time, 18.2 months), the subjective and objective cure rates for the prolapse were 98 and 95 %, respectively. Complications during the follow up included mesh erosion (four cases) and persistent dyspareunia (four cases).
Conclusions
Cystocele repair with mesh placement through transobturator route can be considered a minimally invasive, promising method for the correction of cystocele and SUI based on the low rate of complications, the high rate of success, and the low incidence of recurrence.

Similar content being viewed by others
References
Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, Steegers-Theunissen RP, Burger CW, Vierhout ME (2009) The prevalence of pelvic organ prolapse symptoms and signs and the their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct 20:1037–1045
Comiter CV, Vasavada SP, Raz S (1999) Transvaginal culdosuspension: technique and results. Urology 54:819–822
Safir MH, Gousse AE, Rovner ES, Ginsberg DA, Raz S (1999) 4-Defect repair of grade 4 cystocele. J Urol 161:587–594
Moore RD, Miklos JR (2009) Vaginal repair of cystocele with anterior wall mesh via transobturator route: efficacy and complications with up to 3 years follow up. Adv Urol. doi:10.1155/2009/743831
Moore RD, Beyer RD, Jacoby K, Freedman SJ, McCammon KA, Gambla MT (2010) Prospective multicenter trial assessing type I, polypropylene mesh placed via transobturator route for the treatment of anterior vaginal prolapse with 2-year follow-up. Int Urogynecol J 21:545–552. doi:10.1007/s00192-009-1071-y
Withagen MI, Milani AL, den Boon J, Vervest MD, Vierhout ME (2011) Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized trial. Obstet Gynecol 117:242–250. doi:10.1097/AOG.0b013e318203e6a5
Moore RD, Miklos JR (2009) Vaginal mesh kits for pelvic organ prolapse, friend or foe: a comprehensive review. Sci World J 9:163–189
Sung VW, Rogers RG, Schaffer JI, Balk EM, Uhlig K, Lau J, Abed H, Wheeler TL 2nd, Morrill MY, Clemons JL, Rahn DD, Lukban JC, Lowenstein L, Kenton K, Young SB, Society of Gynecologic Surgeons Systematic Review Group (2008) Graft use in transvaginal pelvic organ prolapse repair: a systematic review. Obstet Gynecol 112:1131–1142. doi:10.1097/AOG.0b013e3181898ba9
Altman D, Falconer C (2007) Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol 109(2 Pt 1):303–308. doi:10.1097/01.AOG.0000250970.23128.63
Margulies RU, Lewicky-Gaupp C, DE Fenner, McGuire EJ, Clemens JQ, Delancy JO (2008) Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol 199:e1–e4. doi:10.1016/j.ajog.2008.07.049
Ridgeway B, Walters MD, Paraiso MF, Barber MD, McAchran SE, Goldman HB, Jelovsek JE (2008) Early experience with mesh excision for adverse outcomes after transvaginal mesh placement using prolapse kits. Am J Obstet Gynecol 199:e1–e7. doi:10.1016/j.ajog.2008.07.055
Iglesia CB, Sokol AL, Sokol ER, Kudish BI, Gutman RE, Peterson JL, Shott S (2010) Vaginal mesh for prolapse: a randomized controlled trial. Obstet Gynecol 116(2 Pt 1):293–303. doi:10.1097/AOG.0b013e3181e7d7f8
Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P (2011) Pelvic organ prolapse quantification system (POP-Q)––a new era in pelvic prolapse staging. J Med Life 4:75–81
Jacquetin B, Fatton B, Rosenthal C, Clavé H, Debodinance P, Hinoul P, Gauld J, Garbin O, Berrocal J, Villet R, Salet Lizée D, Cosson M (2010) Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 3-year prospective follow-up study. Int Urogynecol J 21(12):1455–1462. doi:10.1007/s00192-010-1223-1230
Vaiyapuri GR, Han HC, Lee LC, Tseng AL, Wong HF (2012) Retrospective study of transobturator polypropylene mesh kit for the management of pelvic organ prolapse. Singap Med J 53(10):664–670
Renaudie J, Brouziyne M, Priou G, Devoldère Marie G, de Tayrac R (2013) Safety and 12 months results on stage 3–4, cystocele repair by the vaginal route using a light weight mesh. Prog Urol 23:237–243
Eboue C, Marcus-Braun N, von Theobald P (2010) Cystocele repair by transobturator four arms mesh; monocentric experience of 123 patients. Int Urogynecol J 21:85–93
Borrell Palanca A, Chicote Pérez F, Queipo Zaragoza JA, Beltran Meseguer JF, Esteve Claramunt J, Pastor Sempere F (2004) Cystocele repair with a polypropylene mesh: our experience. Arch Esp Urol 57:391–396
Moore RD, Mitchell GK, Miklos JR (2012) Single-incision vaginal approach to treat cystocele and vault prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int Urogynecol J 23:85–91
Shek KL, Rane A, Goh J, Dietz HP (2009) Stress urinary incontinence after transobturator mesh for cystocele repair. Int Urogynecol J Pelvic Floor Dysfunct 20:421–425
Acknowledgments
The authors have no acknowledgements to report.
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samour, H., Abougamra, A. & Sabaa, H.A.M. Minimally invasive cystocele repair technique using a polypropylene mesh introduced with the transobturator route. Arch Gynecol Obstet 291, 79–84 (2015). https://doi.org/10.1007/s00404-014-3374-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3374-6