Abstract
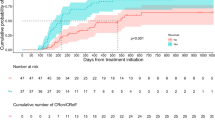
During the last decade, successfully treatment of patients diagnosed with pemphigus vulgaris (PV) with rituximab (RTX) was reported by several authors. The present study has been designed to compare the clinical outcomes and RTX-related side effects between the two groups of early treated (≤ 6 months) and lately treated PV (> 6 months) patients with RTX. We did a retrospective study between Oct 2014 and Jun 2016 to compare the short-term efficacy and safety of RTX in PV diagnosed patients. The primary and secondary endpoints were complete/partial remission of disease and safely tapering of corticosteroids without disease relapse, respectively. Among the 250 RTX exposed PV patients in the selected period, 107 were successfully followed for the mean 19.71 ± 16.78 months. Twenty-four and eighty three have categorized as the early (≤ 6 months after diagnosis) or lately (> 6 months after diagnosis) RTX-treated patients, respectively. A higher rate of complete remission, longer time lasting remission phase, and a lower number of adjuvants were associated with early RTX treatment. Early treatment with RTX might be associated with improvement of clinical effects, but does not seems to be safer than lately RTX therapy. Those in the early treated group may not only have a higher chance to achieve complete remission, but also experience a longer time of disease remission with lower cumulative doses of adjuvant therapy.



Similar content being viewed by others
References
Abasq C, Mouquet H, Gilbert D, Tron F, Grassi V, Musette P, Joly P (2009) ELISA testing of anti-desmoglein 1 and 3 antibodies in the management of pemphigus. Arch Dermatol 145:529–535. https://doi.org/10.1001/archdermatol.2009.9
Ahmed AR, Nguyen T, Kaveri S, Spigelman ZS (2016) First line treatment of pemphigus vulgaris with a novel protocol in patients with contraindications to systemic corticosteroids and immunosuppressive agents: Preliminary retrospective study with a seven year follow-up. Int Immunopharmacol 34:25–31. https://doi.org/10.1016/j.intimp.2016.02.013
Anandan V, Jameela WA, Sowmiya R, Kumar MMS, Lavanya P (2017) Rituximab: a magic bullet for pemphigus. J Clin Diagn Res 11:WC01–WC06. https://doi.org/10.7860/JCDR/2017/21868.9717
Balighi K, Sakhi RS, Daneshpazhooh M, Mahmoudi H, Teimourpour A, Tavakolpour S (2018) Anti-desmoglein-1 levels as predictor of prednisolone tapering in pemphigus vulgaris patients treated with rituximab. Dermatol Ther. https://doi.org/10.1111/dth.12671
Cianchini G, Corona R, Frezzolini A, Ruffelli M, Didona B, Puddu P (2007) Treatment of severe pemphigus with rituximab: report of 12 cases and a review of the literature. Arch Dermatol 143:1033–1038. https://doi.org/10.1001/archderm.143.8.1033
Di Zenzo G, Amber KT, Sayar BS, Muller EJ, Borradori L (2016) Immune response in pemphigus and beyond: progresses and emerging concepts. Semin Immunopathol 38:57–74. https://doi.org/10.1007/s00281-015-0541-1
Feldman RJ (2015) Paradoxical worsening of pemphigus vulgaris following rituximab therapy. Br J Dermatol 173:858–859. https://doi.org/10.1111/bjd.13823
Ingen-Housz-Oro S, Valeyrie-Allanore L, Cosnes A, Ortonne N, Hue S, Paul M, Wolkenstein P, Chosidow O (2015) First-line treatment of pemphigus vulgaris with a combination of rituximab and high-potency topical corticosteroids. JAMA Dermatol 151:200–203. https://doi.org/10.1001/jamadermatol.2014.2421
Joly P, Maho-Vaillant M, Prost-Squarcioni C, Hebert V, Houivet E, Calbo S, Caillot F, Golinski ML, Labeille B, Picard-Dahan C, Paul C, Richard M-A, Bouaziz JD, Duvert-Lehembre S, Bernard P, Caux F, Alexandre M, Ingen-Housz-Oro S, Vabres P, Delaporte E, Quereux G, Dupuy A, Debarbieux S, Avenel-Audran M, D’Incan M, Bedane C, Bénéton N, Jullien D, Dupin N, Misery L, Machet L, Beylot-Barry M, Dereure O, Sassolas B, Vermeulin T, Benichou J, Musette P First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial. Lancet 389:2031–2040. https://doi.org/10.1016/S0140-6736(17)30070-3
Lunardon L, Tsai KJ, Propert KJ, Fett N, Stanley JR, Werth VP, Tsai DE, Payne AS (2012) Adjuvant rituximab therapy of pemphigus: a single-center experience with 31 patients. Arch Dermatol 148:1031–1036. https://doi.org/10.1001/archdermatol.2012.1522
Mouquet H, Musette P, Gougeon ML, Jacquot S, Lemercier B, Lim A, Gilbert D, Dutot I, Roujeau JC, D’Incan M, Bedane C, Tron F, Joly P (2008) B-cell depletion immunotherapy in pemphigus: effects on cellular and humoral immune responses. J Invest Dermatol 128:2859–2869. https://doi.org/10.1038/jid.2008.178
Murrell DF, Dick S, Ahmed AR, Amagai M, Barnadas MA, Borradori L, Bystryn JC, Cianchini G, Diaz L, Fivenson D, Hall R, Harman KE, Hashimoto T, Hertl M, Hunzelmann N, Iranzo P, Joly P, Jonkman MF, Kitajima Y, Korman NJ, Martin LK, Mimouni D, Pandya AG, Payne AS, Rubenstein D, Shimizu H, Sinha AA, Sirois D, Zillikens D, Werth VP (2008) Consensus statement on definitions of disease, end points, and therapeutic response for pemphigus. J Am Acad Dermatol 58:1043–1046. https://doi.org/10.1016/j.jaad.2008.01.012
Pollmann R, Schmidt T, Eming R, Hertl M (2018) Pemphigus: a comprehensive review on pathogenesis, clinical presentation and novel therapeutic approaches. Clin Rev Allergy Immunol 54:1–25. https://doi.org/10.1007/s12016-017-8662-z
Rosenbach M, Murrell DF, Bystryn JC, Dulay S, Dick S, Fakharzadeh S, Hall R, Korman NJ, Lin J, Okawa J, Pandya AG, Payne AS, Rose M, Rubenstein D, Woodley D, Vittorio C, Werth BB, Williams EA, Taylor L, Troxel AB, Werth VP (2009) Reliability and convergent validity of two outcome instruments for pemphigus. J Invest Dermatol 129:2404–2410. https://doi.org/10.1038/jid.2009.72
Sharma VK, Bhari N, Gupta S, Sahni K, Khanna N, Ramam M, Sethuraman G (2016) Clinical efficacy of rituximab in the treatment of pemphigus: a retrospective study. Indian J Dermatol Venereol Leprol 82:389–394. https://doi.org/10.4103/0378-6323.174379
Stasi R, Cooper N, Del Poeta G, Stipa E, Laura Evangelista M, Abruzzese E, Amadori S (2008) Analysis of regulatory T-cell changes in patients with idiopathic thrombocytopenic purpura receiving B cell-depleting therapy with rituximab. Blood 112:1147–1150. https://doi.org/10.1182/blood-2007-12-129262
Tavakolpour S (2017) Current and future treatment options for pemphigus: is it time to move towards more effective treatments? Int Immunopharmacol 53:133–142. https://doi.org/10.1016/j.intimp.2017.10.027
Tavakolpour S, Mahmoudi H, Balighi K, Abedini R, Daneshpazhooh M (2018) Sixteen-year history of rituximab therapy for 1085 pemphigus vulgaris patients: a systematic review. Int Immunopharmacol 54:131–138. https://doi.org/10.1016/j.intimp.2017.11.005
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study approved by research ethics committees in the Tehran University of Medical Sciences.
Rights and permissions
About this article
Cite this article
Balighi, K., Daneshpazhooh, M., Mahmoudi, H. et al. Comparing early and late treatments with rituximab in pemphigus vulgaris: which one is better?. Arch Dermatol Res 311, 63–69 (2019). https://doi.org/10.1007/s00403-018-1881-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-018-1881-1