Abstract
Purpose
This systematic review and meta-analysis aimed to evaluate the safety of outpatient and inpatient Unicompartmental Knee Arthroplasty (UKA) based on the incidence of adverse events.
Method
A systematic search of the literature was performed in October 2022 on PubMed, Web of Science, Cochrane library, and Embase. The Meta package for R was used to perform the meta-analysis.
Result
Five studies with a total of 26,301 patients were included. 5813 patients (22.1%) were treated with outpatient UKA, and 20,488 patients (77.9%) were treated with inpatient UKA. There were no statistically significant differences in the incidence of total complications (RR = 1.36, 95% CI = 0.64–2.89, Z = 0.79, P = 0.43), readmission (RR = 1.02, 95% CI = 0.40–2.60, Z = 0.05, P = 0.96), and venous thrombosis (RR = 1.43, 95% CI = 0.96–2.11, Z = 1.78, P = 0.08). Incidence rates were lower in outpatient UKA regarding urinary tract infection (RR = 1.48, 95% CI = 1.07–2.04, Z = 2.40, P = 0.02), pulmonary embolus (RR = 7.48, 95% CI = 1.80–31.17, Z = 2.76, P < 0.01), and transfusion (RR = 2.77, 95% CI = 1.63–4.71, Z = 3.78, P < 0.01).
Conclusion
In summary, outpatient UKA shows lower incidences of hospital-acquired complications such urinary tract infection, pulmonary embolus, and transfusion. It's worth noting that the incidences of total complications, readmission, and venous thrombosis in outpatient UKA were not higher than the incidences of inpatient UKA, suggestting that outpatient UKA can be considered a safe alternative to inpatient UKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) is becoming an increasingly popular procedure for unicompartmental knee osteoarthritis [1,2,3]. Traditionally, UKA was considered an inpatient procedure, while recently several studies have reported that outpatient UKA is feasible [4,5,6,7].
Outpatient UKA is considered beneficial to reduce the risk of hospital-acquired infections, start early rehabilitation in a familiar environment, and improve patient satisfaction, besides, outpatient UKA can be an attractive option to reduce the economic burden on the healthcare systems [8,9,10,11].
It is unclear which of these two procedures is clinically superior and safer. The purpose of this study was to synthesize the current literature and provide further data regarding the safety of outpatient and inpatient UKA.
Materials and methods
According to PRISMA guidelines, this meta-analysis was conducted.
Search strategy
Potentially relevant articles were identified through searches in PubMed, Web of Science, Cochrane library, Embase, and Google Scholar from inception to October 2022. The keywords “unicompartmental arthroplasty”, “outpatient” and “inpatient” combined using Boolean logic were used to conduct the search. The reference lists of retrieved articles were also searched for additional studies.
Inclusion criteria
Studies were considered eligible if they met all of the following criteria: (1) the patients were treated with primary UKA; (2) The study was designed to compare outcomes of outpatient and inpatient UKA; (3) reporting at least one of the following outcomes: total complications, readmission, urinary tract infection, pulmonary embolism, venous thrombosis, and erythrocyte transfusion. Total complications were defined as various adverse events occurring in patients postoperatively, such as surgical complications, infections, bleeding, nerve injuries, and others.
Exclusive criteria
The following articles were excluded from the search: (1) duplicate articles or articles with overlapping data; (2) case reports, conference reports, systematic reviews, and meta-analyses; (3) article is not written in English.
Data extraction
A pair of independent reviewers screened titles/abstracts and relevant full-text studies, in case of disagreement, a third investigator was consulted. The following information was extracted from studies: the author’s name, year of publication, study type, patient demographics, and the indicators of adverse events, including total complications, readmission, urinary tract infection, pulmonary embolism, venous thrombosis, and transfusion.
Quality assessment
The quality of the study was assessed using the Newcastle–Ottawa Scale (NOS). For each observational study, a score of 0–9 was assigned. A study with a score > 6 was considered high quality.
Data analysis and statistical methods
The statistical analysis was performed using the R package “meta”. The I2 test and the Q test were used to assess heterogeneity between the included studies. If there was heterogeneity (p < 0.05 or I2 > 50%), we used a random-effects model, otherwise, we used a fixed-effects model. We presented mean differences (MDs) and 95% confidence intervals (CIs) for continuous outcomes. For dichotomous variables, risk ratios (RRs) with 95% CIs were calculated.
Results
Search results
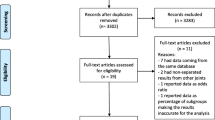
A total of 183 studies were identified through the search strategy. After removing duplicates, 140 studies remained. Then, a total of 113 studies were excluded based on their titles and abstracts. Eventually, 5 studies were eligible for data extraction and meta-analysis (Fig. 1).
Characteristics of the included studies
A total of 26,301 patients were included in our analysis. 5813 patients (22.1%) were treated with outpatient UKA, and 20,488 patients (77.9%) were treated with inpatient UKA. Patient demographic characteristics are presented in Table 1.
Total complications
Three studies were enrolled to compare the incidence of total complications between outpatient and inpatient UKA. As shown in Table 2, significant heterogeneity existed among studies and a random effect model was employed (P < 0.01, I2 = 79%). As shown in Fig. 2, there were no statistically significant differences in the incidence rate of total complications between outpatient and inpatient UKA. The results of the sensitivity analysis suggested that the result was unstable. Meanwhile, there was no obvious publication bias observed in the funnel plot and Egger’s test (t = 0.30, P = 0.82).
Readmission
Three studies were enrolled to compare the incidence of readmission between outpatient and inpatient UKA. Significant heterogeneity existed among studies and a random effect model was employed (P < 0.01, I2 = 83%). As shown in Fig. 3, there were no statistically significant differences in the incidence rate of readmission between outpatient and inpatient UKA. The results of the sensitivity analysis suggested that the result was unstable. Meanwhile, there was no obvious publication bias observed in the funnel plot and Egger’s test (t = 0.26, P = 0.84).
Venous thrombosis
Three studies were enrolled to compare the incidence of venous thrombosis between outpatient and inpatient UKA. There was no significant heterogeneity existing among studies and a fixed effect model was employed (P = 0.70, I2 = 0%). As shown in Fig. 4, there were no statistically significant differences in the incidence rate of venous thrombosis between outpatient and inpatient UKA. The results of the sensitivity analysis suggested that the result was unstable. Meanwhile, there was no obvious publication bias observed in the funnel plot and Egger’s test (t = 0.15, P = 0.90).
Urinary tract infection
Four studies were enrolled to compare the incidence of urinary tract infection between outpatient and inpatient UKA. There was no significant heterogeneity existing among studies and a fixed effect model was employed (P = 0.10, I2 = 52%). As shown in Fig. 5, the incidence rate of urinary tract infection was lower in outpatient. The results of the sensitivity analysis suggested that the result was stable and reliable. Meanwhile, there was no obvious publication bias observed in the funnel plot and Egger’s test (t = 1.96, P = 0.19).
Pulmonary embolus
Three studies were enrolled to compare the incidence of pulmonary embolus between outpatient and inpatient UKA. There was no significant heterogeneity existing among studies and a fixed effect model was employed (P = 0.65, I2 = 0%). As shown in Fig. 6, the incidence rate of pulmonary embolus was lower in outpatient. The results of the sensitivity analysis suggested that the result was stable and reliable. Meanwhile, there was no obvious publication bias observed in the funnel plot and Egger’s test (t = 0.16, P = 0.90).
Transfusion
Three studies were enrolled to compare the incidence of transfusion between outpatient and inpatient UKA. There was no significant heterogeneity existing among studies and a fixed effect model was employed (P = 0.20, I2 = 38%). As shown in Fig. 7, the incidence rate of transfusion was lower in outpatient. The results of the sensitivity analysis suggested that the result was stable and reliable. Meanwhile, there was no obvious publication bias observed in the funnel plot and Egger’s test (t = 2.00, P = 0.29).
Discussion
To our knowledge, this is the first systematic review and meta-analysis to evaluate the safety of outpatient UKA. Previous studies showed that outpatient total knee arthroplasty (TKA) is a safe and effective procedure, which prompted the implementation of outpatient UKA [12,13,14]. Our study demonstrates that outpatient UKA shows lower incidences of hospital-acquired complications and can be considered as a safe alternative to inpatient UKA.
In fact, outpatient UKA has been performed more frequently and at a lower cost in recent years [15,16,17,18]. In a study conducted by Bosch et al, the PearlDiver database was employed and a total of 9121 patients were treated with UKA from 2007 to 2016, Meanwhile, the authors pointed out that the costs of outpatient UKA were significantly lower than the costs of inpatient UKA [6]. Similarly, Richter et al. noted that the medical costs of outpatient UKA averaged $20,500, while the medical costs of inpatient UKA averaged $46,845, in other words, almost 50% cost savings were achieved by outpatient UKA [8].
With the rising incidence of outpatient UKA, studies confirming the safety of outpatient UKA were necessary. In a study conducted by Hur et al., the patients undergoing UKA from 2005 to 2018 were reviewed, the patients were divided into an early cohort (from 2005 to 2015) and a late cohort (from 2016 to 2018), and there were lower incidence rates of surgical-site infection in inpatient UKA compared with outpatient UKA in the early cohort, in contrast, there were lower incidence rates of any complication in outpatient UKA compared with inpatient UKA in the late cohort, which indicated an improvement in quality of outpatient UKA over time [19]. Similarly, in a study conducted by Bovonratwet et al., 568 outpatient and 5312 inpatient UKA cases were reviewed, and there were no significant differences in any perioperative complications or any postoperative complications between the outpatient and inpatient cohorts [20].
In our study, outpatient UKA had lower incidences compared to inpatient UKA regarding urinary tract infection, transfusion, and pulmonary embolism. In fact, outpatient UKA may adhere to stricter patient selection criteria, primarily targeting younger individuals with fewer complications. In the study by Bovonratwet et al., the mean age of the outpatient UKA was 62.9 years, whereas the mean age of the inpatient UKA was 63.7 years [20]. Edward et al. pointed out that a higher prevalence of comorbidities such as diabetes mellitus, hypertension, chronic obstructive pulmonary disease, and hypoalbuminemia among inpatient UKA [19]. Furthermore, early ambulation and non-general anesthesia such as spinal anesthesia are frequently preferred in outpatient UKA due to the shorter hospital stay. Lei et al. pointed out that early ambulation within 24 h after TKA was associated with lower incidences of deep vein thrombosis (DVT) and pulmonary infection [21]. Although their study targeted patients with TKA, it is reasonable to expect that early ambulation has implications for complications of UKA. On the other hand, Edward et al. reported that the incidence of regional anesthesia in inpatient UKA was 32.5%, lower than the incidence of 32.9% in outpatient UKA from 2005 to 2015. Additionally, from 2016 to 2018, the incidence of regional anesthesia in inpatient UKA was 44.3%, also lower than the incidence of 46.8% in outpatient UKA [19]. Lu et al. observed that within the cohort of patients undergoing UKA, those who received general anesthesia experienced longer operative time and higher incidences of DVT and postoperative superficial infections in comparison to those who received spinal anesthesia [22]. Furtherly, Held et al. emphasized the effect of operative time on postoperative complications after UKA, they noted that surgical times longer than 2 h for primary UKA increase the risk of surgical site infection, reoperation, and blood transfusion [23].
Our study has several limitations. First, this meta-analysis only included 5 studies and the sample size of patients was relatively small, which was detrimental to strong conclusions. Second, according to the sensitivity analysis, the combined results of total complications, readmission, and venous thrombosis were unstable. Third, due to the limitations of the included studies, specific details about the duration of follow-up were not consistently reported, further studies were needed to provide insights into the issues.
In summary, outpatient UKA shows lower incidences of hospital-acquired complications such urinary tract infection, pulmonary embolus, and transfusion. It's worth noting that the incidences of total complications, readmission, and venous thrombosis in outpatient UKA were not higher than the incidences of inpatient UKA, suggestting that outpatient UKA can be considered a safe alternative to inpatient UKA.
Data Availability
All relevant data are reported within this manuscript, additional information will be available upon request to the corresponding author.
Code availability
All computer codes required to generate these results will be available upon request to the corresponding author.
References
Huiyong D, Nan Z, Diyang Z et al (2021) More anterior contact position in patients with fixed-bearing unicompartmental knee arthroplasty during daily activities than wear simulator. Front Bioeng Biotechnol 9:666435
Riddle DL, Jiranek WA, McGlynn FJ (2008) Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty 23(3):408–412
Gang Xi, Hao-Hao W, Hao Li et al (2022) Short-term outcomes of Oxford unicompartmental knee arthroplasty with coronal subluxation of the knee: a retrospective case-control study. J Orthopaed Traumatol 23(1):6
Berger RA, Kusuma SK, Sanders SA et al (2009) The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res 467(6):1443–1449
Beard DJ, Murray DW, Rees JL et al (2002) Accelerated recovery for unicompartmental knee replacement–a feasibility study. Knee 9(3):221–224
Bosch Liam C, Bala A, DenduluriSahitya K et al (2020) Reimbursement and complications in outpatient vs inpatient unicompartmental arthroplasty. J Arthroplast. 35(6):86–91
Ford MC, Walters JD, Mulligan RP et al (2020) Safety and cost-effectiveness of outpatient unicompartmental knee arthroplasty in the ambulatory surgery center: a matched cohort study. Orthop Clin North Am 51(1):1–5
Richter DL, Diduch DR (2017) Cost comparison of outpatient versus inpatient unicompartmental knee arthroplasty. Orthop J Sports Med 5(3):2325967117694352
Cody JP, Pfefferle KJ, Ammeen DJ et al (2018) Is outpatient unicompartmental knee arthroplasty safe to perform at an ambulatory surgery center? A comparative study of early post-operative complications. J Arthroplasty 33(3):673–676
Jaibaji M, Volpin A, Haddad FS et al (2020) Is outpatient arthroplasty safe? A systematic review. J Arthroplasty. 35(7):1941–1949
Arndt Kristine B, Varnum C, Lindberg-Larsen M et al (2022) Readmissions and mortality after outpatient vs inpatient unicompartmental knee arthroplasty in Denmark—A propensity score matched study of 5,384 procedures. Knee 38:50–55
Husted C, Gromov K, Hansen Helle K et al (2020) Outpatient total hip or knee arthroplasty in ambulatory surgery center versus arthroplasty ward: a randomized controlled trial. Acta Orthopaed. 91(1):42–47
Kolisek FR, McGrath MS, Jessup NM et al (2009) Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res 467(6):1438–1442
Kirill G, Per K-A, Peter R et al (2017) Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop 88(5):516–521
Hoorntje A, Koenraadt Koen LM, BoevéMargreet G et al (2017) Outpatient unicompartmental knee arthroplasty: who is afraid of outpatient surgery? Knee Surg Sports Traumatol Arthrosc 25(3):759–766
Cross MB, Berger R (2014) Feasibility and safety of performing outpatient unicompartmental knee arthroplasty. Int Orthopaed. 38(2):443–447
Pollock M, Somerville L, Firth A et al (2016) Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: a systematic review of the literature. JBJS Rev 4:12
KortNanne P, Bemelmans Yoeri FL, SchotanusMartijn GM (2017) Outpatient surgery for unicompartmental knee arthroplasty is effective and safe. Knee Surg Sports Traumatol Arthrosc 25(9):2659–2667
Hur Edward S, Serino J, Bohl Daniel D et al (2021) Fewer adverse events following outpatient compared with inpatient unicompartmental knee arthroplasty. J Bone Joint Surg Am 103(22):2096–2104
Bovonratwet P, Ondeck NT, Tyagi V et al (2017) Outpatient and inpatient unicompartmental knee arthroplasty procedures have similar short-term complication profiles. J Arthroplasty. 32(10):2935–2940
Lei YT, Xie JW, Huang Q et al (2021) Benefits of early ambulation within 24 h after total knee arthroplasty: a multicenter retrospective cohort study in China. Mil Med Res 8(1):17
Lu Y, Cregar WM, Goodloe JB et al (2020) General anesthesia leads to increased adverse events compared with spinal anesthesia in patients undergoing unicompartmental knee arthroplasty. J Arthroplasty 35(8):2002–2008
Held MB, Boddapati V, Sarpong NO et al (2021) Operative duration and short-term postoperative complications after unicompartmental knee arthroplasty. J Arthroplasty 36(3):905–909
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the Beijing‐Tianjin‐Hebei Cooperative Basic Research Program (21JCZXJC00030).
Author information
Authors and Affiliations
Contributions
DSC and JWZ were responsible for study concept and writing the article. and LL were responsible for screened the abstracts and reviewed the article. JWZ and TFW was responsible for reviewing and writing the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This kind of study does not require ethical approval.
Informed consent
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, JW., Wang, TF., Chen, DS. et al. Safety evaluation of outpatient vs inpatient unicompartmental knee arthroplasty: a systematic review and meta-analysis. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05446-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05446-8