Abstract
Purpose
Arthroscopic reconstruction techniques for higher-grade posterolateral corner (PLC) injuries (Fanelli Type B, PoLIS LI-B) have not yet been validated in clinical studies. The open reconstruction technique described by Arciero is well-established and showed good restoration of joint stability in previous studies. This study aimed to compare clinical outcomes of this established open surgery technique to a newly developed arthroscopic technique in a prospective randomized clinical trial.
Methods
Between 2019 and 2021, this study focused on chronic high-grade PLC injuries (Fanelli Type B, PoLIS LI-B). Group A consisted of patients treated with conventional open surgery following Arciero’s technique, while Group B included patients treated with Arciero’s arthroscopic technique. All cases underwent additional PCL reconstruction. After a minimum 12-month follow-up, clinical scores and objective stability assessments were compared between the groups.
Results
In total, 26 (group A 12, group B 14) eligible patients with a mean follow-up of 14.9 ± 7.2 months were evaluated in the present study. Knee stability and patient-reported outcome scores (PROMS) were significantly improved when comparing pre- and post-operative values (p < 0.0001). No clinically relevant differences in PROMS (Lysholm: A 83.9 ± 11.4 vs. B 85.3 ± 13.8; IKDC: A 76.91 ± 12.6 vs. B 76.8 ± 15.7) were shown in both groups. Additionally, no statistically significant differences were detected between groups with respect to external rotation, range of motion and instrumental stability testing. Arthroscopic reconstruction showed significantly shorter operation time (p = 0.0109). There were no clinical failures or neurovascular complications of the surgical procedures.
Conclusion
Both surgical techniques for isolated chronic PLC Fanelli Type B injuries significantly improved the knee stability, were equivalent with respect to PROMs and led to good clinical results. However, arthroscopic PLC reconstruction was associated with a shorter surgery time compared to open PLC reconstruction. Therefore, arthroscopic PLC reconstruction may be a viable option in the hands of an experienced surgeon.
Level of evidence
Prospective cohort study, II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The posterolateral corner (PLC) consists primarily of the lateral collateral ligament (LCL) and the popliteus complex (PTC), which includes the popliteus muscle tendon (PLT) unit and the arcuate complex. The arcuate complex is formed by the popliteofibular ligament (PFL), the fabellofibular ligament and the popliteomeniscal fibers. Functionally, the popliteus complex serves as the most important static and dynamic stabilizer against external tibial rotation and posterior translation [1,2,3], whereas the LCL primarily provides stability against varus forces [4]. For posterolateral rotational instability (PLRI), Fanelli et al. [5] described a type B injury pattern marked by increased external rotation (ER), slight varus relaxation, and excessive posterior laxity, indicative of damage to PLT, PFL, LCL, and PCL. Weiler et al. [6], in a subsequent development, introduced the Posterolateral Instability Score (PoLIS) aligned with the aforementioned injury pattern, specifically PoLIS LI-B, presenting an innovative framework for evaluating injury severity and surgical decision-making.
Many arthroscopic reconstruction techniques have been proposed for restoring stability while utilizing the benefits of arthroscopic compared to open surgeries [7]. An arthroscopic approach can offer a better visualization of anatomic landmarks, avoid surgical morbidity and iatrogenic neurovascular injury, and provide the possibility of simultaneous arthroscopic PLC and PCL reconstruction [8,9,10]. In a biomechanical study arthroscopic anatomic reconstruction of the PLC restored nearly normal stability of the knee [11]. Novel arthroscopic techniques for anatomical reconstruction in higher-grade instabilities (Fanelli Type B) based on Arciero’s and LaPrade’s procedures, have been described by Frings et al., and Kolb et al. [12, 13]. Recently, both arthroscopic procedures were clinically compared for the treatment of type B injuries with promising results, showing sufficient restoration of posterolateral rotational instability, varus instability and posterior drawer through both techniques [14].
To our knowledge, no study has compared the clinical outcomes between arthroscopic and open PLC reconstruction in patients with Fanelli type B injuries. The aim of this study was to compare the arthroscopic anatomical PLC reconstruction technique described by Frings et al. [12] with the open conventional technique described by Arciero [15]. We hypothesized that both procedures could equally provide sufficient restoration of posterior, lateral, and external rotational stability and a comparable clinical outcome.
Materials and methods
Patient population
The study design was approved by the local ethics committee and an informed consent was obtained by each patient (2021-100677-BO-ff). All patients were informed about the available treatment options and provided their preoperative agreement to undergo the procedure explained to them.
A prospective study included 26 patients with high-grade posterolateral corner injuries (Fanelli Type B, PoLIS LI-B [6]) between 2019 and 2021. These injuries were treated either arthroscopically with reconstruction according to Frings et al. [12] (Group A) or open with Arciero’s conventional technique [15] (Group B).
Only patients presenting with chronic injuries (> 6 weeks), a combination of varus and posterolateral instability and additional posterior instability due to injury to the posterior cruciate ligament were included (see Fig. 1). The primary diagnosis was made by imaging (MRI, stress radiographs) and physical examination to assess ligamentous instability. Exclusion criteria were patient age under 18, obese patients (grade II according to WHO definition with BMI > 35 km/m2), coronal and sagittal malalignment, peroneal nerve injuries, higher- or lower-grade posterolateral corner injuries, additional ligamentous injury (Anterior cruciate ligament, Medial ligament complex) and additional affected structures (e.g. biceps femoris muscle, tendon rupture, iliotibial band injury and fractures at lower extremity).
Preoperative clinical testing
The preoperative examination included ROM, Varus stress test, the posterior drawer test, and assessments of internal and ER at 30° and 90° of knee flexion (Dial test). The Dial test was considered positive at 30° if there was ≥ 10° more ER on the injured side, and positive at 90° if this side-to-side difference remained or increased. Additionally, clinical examination was conducted to assess lateral gapping by applying varus stress at full extension and 20°–30° of flexion. The clinical degree of varus instability was qualitatively compared with the contralateral side using the Hughston classification (negative, grade I - mildly positive, grade II - positive, grade III - severely positive) [16]. Only patients with a positive dial test at both knee flexion angles and mild varus gapping (mildly positive) were included (Fanelli B). Stability testing was conducted in pre-examination and during the anaesthetic examination.
Surgical management
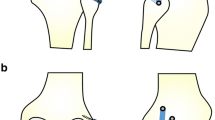
The type of surgical procedure was determined by block randomization. Initially, a brief arthroscopy was performed to rule out meniscal tears and any associated chondral lesions. Meniscal repair was possible in all cases. The arthroscopic anatomical reconstruction procedure introduced by Frings et al. [12] (Group A) and Arciero’s open technique [15] (Group B) were described in detail before. Arciero’s technique is a fibula-based technique with an anatomic transfibular tunnel placement, from anterolateral to posteromedial, in accordance with the native functional anatomy of the LCL and PLT (Figs. 2 and 3).
Schematic drawing of Arciero’s fibula-based, single-graft reconstruction technique for posterolateral corner reconstruction in posterior (A) and lateral view (B) modified from Weiss et al. [14]
Intraoperative situs showing Arciero’s open technique for a 23-year-old patient who presented 7 weeks after a bike accident with a torn PCL and femoral avulsion of PLT, resulting in posterolateral rotational instability (Fanelli B). (A) The fibula head (FH) was shuttled with a suture. The peroneal nerve (PN) was exposed and marked with a vessel loop. (B) Two guidewires are introduced into the femoral native origins of the popliteus tendon (PLT) and lateral collateral ligament (LCL). (C) An autologous gracilis tendon graft is shuttled into the fibula head drilling canal and fixated with an interference screw. (D) The graft after fixation in the LCL and PLT tunnel
In addition, PCL reconstruction was arthroscopically performed during the same procedure. Hamstring tendon autografts were used in all cases. The duration of surgery was evaluated (starting from skin incision, including tendon harvest and all arthroscopic procedures until skin closure).
Rehabilitation
Peripheral nerve block anesthesia was used in all cases. Physical therapy adhering to standardized protocols was initiated 48 h after the operation. For a period of 12 weeks, stabilizing braces with posterior tibial support (Jack PCL Brace; Albrecht, Bernau am Chiemsee, Germany) were worn while limiting the range of motion for 6 weeks. For the initial 2 weeks following surgery, the knee was flexed to a maximum angle of 20°. Physical therapists performed passive knee flexion up to 45° in a prone position after drain removal. During weeks 3 and 4, patients received passive mobilisation up to 60° of flexion and up to 90° during weeks 5 and 6. The patients had a weight-bearing limit of 20 kg for six weeks. After six weeks, the patients were allowed to have a full range of motion and gradually started full weight-bearing.
Postoperative clinical testing
Follow-up examination was conducted at least 12 month following surgery and included functional outcome scoring systems by Lysholm and International Knee Documentation Committee (IKDC). Subjective pain during exercise was quantified by visual analogous scale (VAS). Posterior tibial translation (PTT) measurement was conducted by Rolimeter-Test (Aircast, Neubeuern, Germany) to measure the posterior translation of the tibia in the technique according to Höher et al. [17]. Clinical examination of ROM and ER in 30° and 90° of flexion was performed with the use of a HALO Goniometer® (HALO, model HG1, HALO Medical Devices, Australia) [18]. Varus stability was tested clinically at 0 and 30 degrees to evaluate collateral ligament stability.
We defined postoperative clinical failure as non-traumatic re-rupture of the posterior cruciate ligament that was confirmed through magnetic resonance imaging (MRI) or arthroscopy, or through a side-to-side difference (SSD) greater than 6 mm in posterior drawer test or a dial test SSD of ER greater than 10°.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 8 (San Diego, CA, USA). Data are presented as means and standard deviations (SD). Differences between the groups were calculated with the Student’s t test and Mann Whitney U-Test for non-parametric parameters. Difference within groups were calculated with paired Student’s t test. Categorical parameters were compared using Fisher’s exact text. A p-value < 0.05 was considered significant. An a priori sample size calculation indicated n = 24 patients (12 in each group) to detect a difference of 10 points in the clinical Lysholm score using G-Power (version 3.1.9.7., Heinrich Heine University, Düsseldorf) with a 𝛼 error of 5% and a power of 0.8.
Results
Patient demographics
Demographic data and surgical details of the included cases are displayed in Table 1. After an average follow-up of 14.9 ± 7.2 months, 26 patients were ultimately included in the study, 4 patients were lost to follow-up for geographical reasons. Duration of surgery was significantly longer in Group A patients than in group B (139.8 ± 31.8 vs. 183.2 ± 45.8 min; p = 0.0109).
Patient reported functional outcome
Functional outcome scores at follow-up are shown in Table 2. There was no difference between the two groups according to VAS, Lysholm and IKDC scores. All participants were content with the overall outcome and would undergo the surgery again in hindsight. Among those who received arthroscopic treatment, six Patients (42.9%) were satisfied and eight Patients (57.1%) expressed high satisfaction. In the open group, two Patients (16.7%) expressed conditional contentment, whereas six Patients (41.7%) were satisfied, and six Patients (41.7%) were highly satisfied.
Clinical testing and instrumental stability testing
Regarding PTT, all patients except one had a preoperative SSD greater than 11 mm. In total, eleven patients had a preoperative SSD greater than 15 mm, with five patients in group A and six patients in group B. At the postoperative follow-up, there was no significant difference in SSD between the groups in terms of objective assessments of posterior drawer test, flexion or dial test results in ER at 30 or 90° flexion. Patients in both groups were postoperatively sufficiently clinically stable under varus loading (Varus stress-test: Negative 88.5%, mildly positive 11.5%) and showed a negative Dial test in 30° and 90° Flexion. The SSD of PTT, varus stability, SSD of ER and PROMS (Lysholm and IKDC-Score) were significantly improved in both groups when comparing preoperative and postoperative values (Groups A and B p < 0.0001). (see Table 3)
Complications
No patient experienced complications such as vascular or nerve injury, compartment syndrome, deep vein thrombosis or infection were reported. One patient in Group A reported joint stiffness (ROM 0-5-110°), which was resolved by arthroscopic arthrolysis after 46 weeks (ROM at last follow-up 0-0-125°). There were no cases of clinical failure in both groups.
Discussion
The main finding in this prospective examination of chronic Fanelli B/PoLIS LI-B injuries was that the arthroscopic as well as the open technique showed sufficient restoration of posterior, rotational and lateral joint stability in clinical examinations and led to good (Lysholm-Score) and satisfying (IKDC-Score) clinical results.
Open procedures based on Arciero’s technique have shown significantly improved objective and subjective stability in higher grade instabilities, with equivalent clinical outcomes [19]. The arthroscopic equivalents for open Arciero reconstructions, as described by Frings et al. and Liu et al., respectively, provide viable options for those seeking arthroscopic procedures [11, 12, 14]. Arthroscopic PLC reconstruction requires profound knowledge of anatomic relations. However, it offers the benefit of visualizing all key structures, including the posteromedial aspect of the fibular head, for precise fibular drill tunnel placement [8, 20]. Some concerns have been raised regarding arthroscopic PLC reconstructions, such as the risk of tunnel misplacement and neurovascular injuries [21, 22]. However, Weiss et al. and our study’s clinical results did not show any neurovascular or tunnel-related complications [14]. Previous studies have demonstrated that the development of a transseptal portal and posterolateral arthroscopy can be safely performed with intraoperative knee flexion of 90° [8, 23,24,25]. The utilization of dependable soft-tissue and osseous reference points located at the fibular head allows for accurate arthroscopic anatomic fibular tunnel placement in the context of PLC surgery, consequently presenting a reduced probability of tunnel misalignment when contrasted with conventional open surgical methodologies [26]. Additionally, arthroscopic procedures circumvent the necessity for common peroneal nerve preparation and visualization, reducing the risk of nerve injury and saving time [27]. Notably, no instances of peroneal nerve damage were observed in either group in this study, indicating that both procedures are equally safe. We observed a shorter operative time in the arthroscopic group. A possible explanation for this difference could be the better arthroscopic visualisation of key structures and anatomical landmarks, leading to faster tunnel placement, apart from improved wound closure time.
To the best of our knowledge this is the first study to make a direct comparison between arthroscopic and open techniques regarding Fanelli B/PoLIS LI-B injuries. Overall our results align with previous studies that compared PROMS and restoration of stability, and lead to positive postoperative outcomes [14, 28,29,30,31,32,33]. Li et al. [30] conducted a study on PLC injuries, including 27 type A, 10 type B, and 12 type C patients, with 21 acute cases and 28 chronic cases. They used different reconstruction and repair techniques of the PLC and PCL single bundle reconstruction and followed up after a mean of 31.5 ± 9.3 months. The study showed that the PTT of SSD improved from 18.4 ± 9.2 mm to 5.2 ± 5.0 mm, and ER of SSD decreased from 18.0° ± 14.4° to 1.2° ± 7.5°. The same study group compared arthroscopic and open reconstruction of the PLT in combination with PCL reconstruction and showed no difference in PROMS and stability between the two groups of patients (SSD of PTT 4 and 5 mm and ER of 1 and 3°) [31]. Recently, Helal et al. [32] reported on a case series with a mean follow-up of 25 months. They found that 11 patients who underwent a reconstruction of the PLC and PCL had comparable results in external rotation (SSD of ER decreased from 16.7° to 3.5° postoperatively) and clinical outcomes (Lysholm/ IKDC 81/78 points). According to their report, not all of their patients had their varus stability sufficiently restored, whereas in our patients, only three had mildly positive varus instability (11.5%). This aligns with the findings of Sanders et al. [34], who reported that 88.5% of patients had grade 0 varus laxity, while 9.8% had grade I laxity, and 1.7% had grade II laxity. Van Gennip et al. [29] also demonstrated residual varus laxity but good clinical outcomes (Lysholm/IKDC 86/79 points) in 5 Fanelli C and 6 Fanelli B patients who underwent PLC reconstruction with a Larson technique in addition to PCL reconstruction, with a 2-year follow-up. Variations in surgical techniques may account for the difference in Varus stability. It is possible that Arciero’s anatomical technique is more effective in restoring stability than other non-anatomical techniques [35]. However, it is important to note that our study did not include an objective varus stability assessment, and the inclusion of Fanelli C patients in previous studies limits direct comparison. Overall, our results demonstrate that the anatomical technique of Arciero effectively restores the PLC, resulting in comparable PROMS and SSD of ER and PTT when compared to non-anatomical surgical techniques.
Arthrofibrosis is a commonly observed complication in multiligament knee injuries [36]. In this study, the incidence of arthrofibrosis was at 4% (1/26), which is comparable to other PLC-reconstructing studies [31, 32].
Overall, our study adds to the growing body of evidence that supports the feasibility and efficacy of arthroscopic PLC reconstruction for Fanelli B/PoLIS LI-B injuries. Arthroscopic care offers potential benefits, which were demonstrated by our study in terms of slightly increased patient satisfaction and shorter time of operation. However, the arthroscopic technique has a flat and long learning curve. While both arthroscopic and open techniques demonstrated favourable clinical outcomes and stability restoration, the choice of approach should be based on the surgeon’s experience, patient characteristics, and specific injury characteristics. Further research is warranted to explore the learning curve and long-term outcomes associated with arthroscopic PLC reconstruction, as well as to compare different arthroscopic techniques and their outcomes.
Limitations
Scientific conclusions based on this study are limited by the relatively small number of cases due to the rare incidence of these complex injuries. In addition, matched-pair analysis was not possible due to the rarity of PLC injuries. All arthroscopic procedures were carried out by a single surgeon, whereas open surgeries were conducted by multiple surgeons. Although the inclusion and exclusion criteria were precise, the time between injury and surgery varied, but was always > 6 weeks and therefore considered as a chronic injury. Clinical follow-up of anterior-posterior stability testing was performed with the Rolimeter instead of stress radiographs, and varus/valgus instability was detected by clinical examination rather than stress radiographs. Long-term follow-up is needed to validate the concept of arthroscopic PLC reconstruction, as recent studies have shown promising results.
Conclusion
Both surgical techniques for isolated chronic PLC Fanelli Type B injuries significantly improved the knee stability, were equivalent with respect to PROMs and led to good clinical results. However, arthroscopic PLC reconstruction was associated with a shorter surgery time compared to open PLC reconstruction. Therefore, arthroscopic PLC reconstruction may be a viable option in the hands of an experienced surgeon.
References
LaPrade RF et al (2010) Analysis of the static function of the popliteus tendon and evaluation of an anatomic reconstruction: the fifth ligament of the knee. Am J Sports Med 38(3):543–549
Domnick C et al (2017) Kinematics of different components of the Posterolateral Corner of the knee in the lateral collateral ligament-intact state: a human cadaveric study. Arthroscopy 33(10):1821–1830e1
Thaunat M et al (2014) The arcuate ligament revisited: role of the posterolateral structures in providing static stability in the knee joint. Knee Surg Sports Traumatol Arthrosc 22(9):2121–2127
Grood ES, Stowers SF, Noyes FR (1988) Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am 70(1):88–97
Fanelli GC, Larson RV (2002) Practical management of posterolateral instability of the knee. Arthroscopy 18(2 Suppl 1):1–8
Weiler A et al (2021) The posterolateral instability score (PoLIS) of the knee joint: a guideline for standardized documentation, classification, and surgical decision-making. Knee Surg Sports Traumatol Arthrosc 29(3):889–899
Weiss S, Krause M, Frosch KH (2020) Posterolateral corner of the knee: a systematic literature review of current concepts of arthroscopic reconstruction. Arch Orthop Trauma Surg 140(12):2003–2012
Frings J et al (2022) Arthroscopic anatomy of the posterolateral corner of the knee: anatomic relations and arthroscopic approaches. Arch Orthop Trauma Surg 142(3):443–453
Frosch KH et al (2015) Arthroscopic reconstruction of the popliteus complex: accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc 23(10):3114–3120
Feng H et al (2009) Posterolateral sling reconstruction of the popliteus tendon: an all-arthroscopic technique. Arthroscopy 25(7):800–805
Liu P et al (2020) Anatomic, All-Arthroscopic Reconstruction of Posterolateral Corner of the knee: a cadaveric biomechanical study. Arthroscopy 36(4):1121–1131
Frings J et al (2019) Anatomic Reconstruction of the Posterolateral Corner: an all-arthroscopic technique. Arthrosc Tech 8(2):e153–e161
Kolb JP et al (2019) An All-Arthroscopic Technique for Complex Posterolateral Corner Reconstruction. Arthrosc Tech 8(9):e999–e1006
Weiss S, Krause M, Frosch KH (2023) Clinical results after arthroscopic reconstruction of the posterolateral corner of the knee: a prospective randomized trial comparing two different surgical techniques. Arch Orthop Trauma Surg 143(2):967–975
Arciero RA (2005) Anatomic posterolateral corner knee reconstruction. Arthroscopy 21(9):1147
Hughston J et al (1976) Classification of knee ligament instabilities. Part II. The lateral compartment. JBJS 58(2):173–179
Höher J et al (2015) Rolimeter measurements are suitable as substitutes to stress radiographs in the evaluation of posterior knee laxity. Knee Surg Sports Traumatol Arthrosc 23(4):1107–1112
Correll S et al (2018) RELIABILITY AND VALIDITY OF THE HALO DIGITAL GONIOMETER FOR SHOULDER RANGE OF MOTION IN HEALTHY SUBJECTS. Int J Sports Phys Ther 13(4):707–714
Boksh K et al (2023) Fibular- Versus Tibiofibular-Based Reconstruction of the Posterolateral Corner of the knee: a systematic review and Meta-analysis. Am J Sports Med, : p. 3635465221138548
Krause M et al (2019) Posterolateral rotatory knee Instability-MRI evaluation of anatomic landmarks for tibial Drill tunnel Placement in Open and Arthroscopic Popliteus Tendon Reconstruction. J Knee Surg 32(7):667–672
Chahla J et al (2019) Posterolateral corner of the knee: an expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc 27(8):2520–2529
Chahla J, Williams BT, LaPrade RF (2020) Editorial Commentary: shedding light on the Posterolateral Corner of the knee: can we do it with the scope? Is there a Real Benefit? Arthroscopy 36(4):1132–1134
Ahn JH et al (2011) The relationship of neural structures to arthroscopic posterior portals according to knee positioning. Knee Surg Sports Traumatol Arthrosc 19(4):646–652
Makridis KG et al (2013) Neurovascular anatomic relationships to arthroscopic posterior and transseptal portals in different knee positions. Am J Sports Med 41(7):1559–1564
Kim SJ et al (2011) The safe establishment of a transseptal portal in the posterior knee. Knee Surg Sports Traumatol Arthrosc 19(8):1320–1325
Krause M, Weiss S (2023) Comparison of arthroscopic versus Open Placement of the Fibular tunnel in Posterolateral Corner Reconstruction. 36(9):977–987
Hohmann E et al (2021) The anatomical relationship of the common peroneal nerve to the proximal fibula and its clinical significance when performing fibular-based posterolateral reconstructions. Arch Orthop Trauma Surg 141(3):437–445
Sharma A, Saha P, Bandyopadhyay U (2022) Reconstruction of the Posterolateral Corner of the knee using LaPrade and Modified Larson technique: a prospective study. Indian J Orthop 56(1):125–132
van Gennip S et al (2020) Posterolateral corner reconstruction in combined injuries of the knee: improved stability with Larson’s fibular sling reconstruction and comparison with LaPrade anatomical reconstruction. Knee 27(1):124–131
Li Y et al (2019) Midterm clinical outcome of combined posterior Cruciate Ligament Reconstruction and Posterolateral Corner surgery using second-look arthroscopic lateral gutter drive-through Test as an adjunctive evaluation. Orthop Surg 11(3):422–430
Li Y et al (2019) The clinical outcome of arthroscopic Versus Open Popliteal Tendon Reconstruction Combined with posterior Cruciate Ligament Reconstruction in patients with type A posterolateral rotational instability. Arthroscopy 35(8):2402–2409
Helal A et al (2023) Clinical and radiological outcomes of a modified anatomic posterolateral corner reconstruction technique using a single semitendinosus autograft. Arch Orthop Trauma Surg 143(9):5767–5776
Franciozi CE et al (2019) A hamstring-based anatomic posterolateral knee Reconstruction with autografts improves both Radiographic instability and functional outcomes. Arthroscopy 35(6):1676–1685e3
Sanders TL et al (2018) Satisfactory knee function after single-stage posterolateral corner reconstruction in the multi-ligament injured/dislocated knee using the anatomic single-graft technique. Knee Surg Sports Traumatol Arthrosc 26(4):1258–1265
Jackson GR et al (2023) Non-anatomical reconstruction of chronic posterolateral corner knee injuries show failure rates from 0–36% versus 4.3–24.2% for anatomic reconstruction techniques: an updated systematic review reflecting the 2019 expert consensus statement. J Isakos
Fahlbusch H et al (2023) Arthrofibrosis is a common but poorly defined complication in multiligament knee injuries: a systematic review. 143(8):5117–5132
Acknowledgements
Not applicable.
Funding
Not applicable.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conceptualization HF, SW, KHF, MK Methodology SW, HF, RA, MK Validation HF, SW, FP, TD, KHF, RA, MK; Formal analysis HF, SW, JL, MK.; Investigation HF, JL, SW ; Writing—original draft preparation HF, SW; Writing—review and editing all authors; Visualization HF, SW; Supervision KHF; Project administration RA, MK, KHF.; All authors have read and agreed to the final version of this manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the institutional Ethics Committee of the University of Hamburg (2021-100677-BO-ff).
Informed consent
Informed consent was obtained of each study participant prior to inclusion.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fahlbusch, H., Weiß, S., Landenberger, J. et al. Arthroscopic and open reconstruction of the posterolateral corner of the knee have equally good clinical results: first results of a prospective 12-month follow-up study. Arch Orthop Trauma Surg 144, 2745–2752 (2024). https://doi.org/10.1007/s00402-024-05355-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-024-05355-w