Abstract
Introduction
Proximal humerus fractures are usually treated with locking plates, which could present recurrence, screw penetration, joint varization. The push–pull principle was introduced to prevent these risks and showed promising results; a dedicated design was then developed and this feasibility study aims to compare the biomechanical performances of such dedicated push–pull plate with the traditional locking plate using finite elements.
Materials and methods
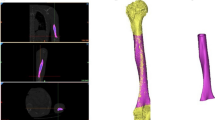
The humerus geometry was obtained from Sawbone CT-scans; the geometries of a traditional locking plate and of the dedicated push–pull one were used. A fracture was added below the humeral head and the plates were virtually implanted. The wire pulling mechanism was simulated connecting the plate to the humeral head apex, considering two levels of tension. Three testing set-ups (axial, torsion and compression bending) were simulated. Stress distributions on bone, plate and screws were measured.
Results
Stress distribution on the distal humerus was similar for both plates. Stress distribution on the proximal humerus was more homogeneous for the push–pull model, showing less unloaded sections (up to 78%). The different levels of tension applied to the wire returned slight differences in terms of stress values, but the comparison with the traditional approach gave similar outcomes.
Conclusions
More homogeneous stress distribution is found with the push–pull plate in all three testing set-ups, showing lower unloaded areas (and thus lower stress-shielding) compared to the traditional plate; the screws implemented returned to be all loaded in at least one of the set-ups, thus showing that they all contribute to plate stability.








Similar content being viewed by others
Data availability
Raw data were generated at BEAMS Department. Derived data supporting the findings of this study are available from the corresponding author [BI] on request.
References
Atalar AC, Eren I, Uludağ S, Demirhan M (2014) Results of surgical management of valgus-impacted proximal humerus fractures with structural allografts. Acta Orthop Traumatol Turc 48(5):546–552. https://doi.org/10.3944/AOTT.2014.14.0115
Barlow JD, Logli AL, Steinmann SP, Sems SA, Cross WW, Yuan BJ, Torchia ME, Sanchez-Sotelo J (2020) Locking plate fixation of proximal humerus fractures in patients older than 60 years continues to be associated with a high complication rate. J Shoulder Elbow Surg 29(8):1689–1694. https://doi.org/10.1016/j.jse.2019.11.026
Capriccioso CE, Zuckerman JD, Egol KA (2016) Initial varus displacement of proximal humerus fractures results in similar function but higher complication rates. Injury 47(4):909–913. https://doi.org/10.1016/j.injury.2016.01.021
Castro-Franco AD, Mendoza-Muñoz I, González-Ángeles Á, Cruz-Sotelo SE, Castañeda AM, Siqueiros-Hernández M (2020) Trends in the characterization of the proximal humerus in biomechanical studies: a review. Appl Sci 10(18):6514. https://doi.org/10.3390/app10186514
Clavert P, Adam P, Bevort A, Bonnomet F, Kempf J-F (2010) Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 19(4):489–494. https://doi.org/10.1016/j.jse.2009.09.005
Floyd SB, Campbell J, Chapman CG, Thigpen CA, Kissenberth MJ, Brooks JM (2019) Geographic variation in the treatment of proximal humerus fracture: an update on surgery rates and treatment consensus. J Orthop Surg Res 14(1):22. https://doi.org/10.1186/s13018-018-1052-2
Götz R, Stefano B, Damiano S, Ronald S, Alexander S, Boyko G, Florian G, Andrea T (2013) Mechanical assessment of local bone quality to predict failure of locked plating in a proximal humerus fracture model. Orthopedics 36(9):e1134–e1140. https://doi.org/10.3928/01477447-20130821-14
Handoll HHG, Elliott J, Thillemann TM, Aluko P, Brorson S (2022) Interventions for treating proximal humeral fractures in adults. In: Cochrane database of systematic reviews. John Wiley and Sons Ltd
Hardeman F, Bollars P, Donnelly M, Bellemans J, Nijs S (2012) Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury 43(2):153–158. https://doi.org/10.1016/j.injury.2011.04.003
Innocenti B (2023) Are flexible metaphyseal femoral cones stable and effective? A biomechanical study on hinged total knee arthroplasty. J Arthroplast 39:1328. https://doi.org/10.1016/j.arth.2023.11.009
Innocenti B, Bori E, Armaroli F, Schlager B, Jonas R, Wilke H-J, Galbusera F (2022) Chapter 34 - the use of computational models in orthopedic biomechanical research. In: Innocenti B, Galbusera F (eds) Human orthopaedic biomechanics. Academic Press, pp 681–712
Jung S-W, Shim S-B, Kim H-M, Lee J-H, Lim H-S (2015) Factors that influence reduction loss in proximal humerus fracture surgery. J Orthop Trauma 29(6):276
Kim SH, Szabo RM, Marder RA (2012) Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res 64(3):407–414. https://doi.org/10.1002/acr.21563
MacLeod AR, Pankaj P, Simpson AHRW (2012) Does screw–bone interface modelling matter in finite element analyses? J Biomech 45(9):1712–1716. https://doi.org/10.1016/j.jbiomech.2012.04.008
Marongiu G, Verona M, Cardoni G, Capone A (2020) Synthetic bone substitutes and mechanical devices for the augmentation of osteoporotic proximal humeral fractures: a systematic review of clinical studies. J Func Biomater 11(2):29. https://doi.org/10.3390/jfb11020029
Mirulla AI, Muccioli GMM, Fratini S, Zaffagnini S, Ingrassia T, Bragonzoni L, Innocenti B (2022) Analysis of different geometrical features to achieve close-to-bone stiffness material properties in medical device: a feasibility numerical study. Comput Methods Prog Biomed 221:106875. https://doi.org/10.1016/j.cmpb.2022.106875
Orman S, Mohamadi A, Serino J, Murphy J, Hanna P, Weaver MJ, Dyer G, Nazarian A, von Keudell A (2019) Comparison of surgical and non-surgical treatments for 3- and 4-part proximal humerus fractures: a network meta-analysis. Should Elb 12(2):99–108. https://doi.org/10.1177/1758573219831506
Patel M, Castaneda P, Kisana H, Roache WK, Dehghan N, McKee MD, Amini MH (2022) Using the greater tuberosity as a reference for placement of proximal humerus plates leads to a high rate of calcar screw malposition. J Orthop Trauma 36(10):525
Putzeys G (2023) The humeral head push-pull plate technique: an alternative way to stabilize the humeral head in varus angulated proximal humeral fractures in the elderly. J Orthop Trauma 37(12):e478
Rupp M, Walter N, Pfeifer C, Lang S, Kerschbaum M, Krutsch W, Baumann F, Alt V (2021) The incidence of fractures among the adult population of Germany. Dtsch Arztebl Int 118(40):665–669
Solberg BD, Moon CN, Franco DP, Paiement GD (2009) Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma 23(2):113
Spross C, Zeledon R, Zdravkovic V, Jost B (2017) How bone quality may influence intraoperative and early postoperative problems after angular stable open reduction–internal fixation of proximal humeral fractures. J Shoulder Elbow Surg 26(9):1566–1572. https://doi.org/10.1016/j.jse.2017.02.026
Sun S, Eichinger JK, Yao H, Friedman RJ (2023) Three-dimensional finite element modeling of glenoid bone loss and baseplate fixation in reverse total shoulder arthroplasty. Seminars Arthroplast JSES 33(4):768–774. https://doi.org/10.1053/j.sart.2023.08.005
Unger S, Erhart S, Kralinger F, Blauth M, Schmoelz W (2012) The effect of in situ augmentation on implant anchorage in proximal humeral head fractures. Injury 43(10):1759–1763. https://doi.org/10.1016/j.injury.2012.07.003
Varga P, Inzana JA, Gueorguiev B, Südkamp NP, Windolf M (2018) Validated computational framework for efficient systematic evaluation of osteoporotic fracture fixation in the proximal humerus. Med Eng Phys 57:29–39. https://doi.org/10.1016/j.medengphy.2018.04.011
Wagner E, Houdek MT, Elhassan BT, Sanchez-Sotelo J, Sperling JW, Cofield RH (2016) Glenoid bone-grafting in revision to a reverse total shoulder arthroplasty: surgical technique. JBJS Essential Surg Tech 6(4):e35
Funding
Funding was provided by VLAIO (Vlmase Agentschap Innoveren & Ondernemen), i.e., Flanders Agency for Innovation & Entrepreneurship(Grant No: HBC.2021.0763).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Putzeys, G., Bori, E., Overes, T. et al. Biomechanical analysis of push–pull principle versus traditional approach in locking plates for proximal humeral fracture treatment. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05342-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05342-1