Abstract
Background
Total Joint Arthroplasties (TJAs) are becoming more popular, resulting in a growing economic burden due to potential postoperative complications, with periprosthetic joint infections (PJIs) playing a significant role. The effect of immunosuppression on PJI risk, particularly in cancer patients following chemotherapy, is unknown. The hypothesis of this study investigated whether chemotherapy increases PJI rates in patients who received post-arthroplasty chemotherapy within one year of surgery.
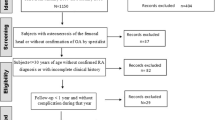
Methods
Data from the M161Ortho dataset of PearlDiver patient records database were utilized using ICD-9, ICD-10, and CPT codes. The cohort includes Total Knee Arthroplasty (TKA), Total Hip Arthroplasty (THA), and Total Shoulder Arthroplasty (TSA) patients who underwent post-arthroplasty chemotherapy within one year after surgery between 2010 and 2022. Patients in the matched control group did not receive post-arthroplasty chemotherapy. Pre-arthroplasty chemotherapy recipients, PJI, and post-op first year revisions were excluded. Analyses including the linear logistic regression were performed via R statistical software.
Results
Totally, 17,026 patients (8,558 TKAs, 6,707 THAs, and 1,761 TSAs) were included. At two (OR = 1.59, p = 0.034), three (OR = 1.57, p = 0.009), and four (OR = 1.40, p = 0.032) years for TKA, and two (OR = 2.27, p = 0.008), three (OR = 2.32, p < 0.001), and four (OR = 2.25, p0.001) years for THA, PJI rates were significantly higher in the chemotherapy group. TSA patients had a significant rise in PJI after four years (OR = 2.20, p = 0.031).
Conclusions
This study reveals a possible relationship between postoperative chemotherapy and an increased incidence of PJI in patients with arthroplasty. Chemotherapy suppresses the immune system, rendering patients more vulnerable to infections. Additional research is required to confirm these findings.


Similar content being viewed by others
References
Alamanda VK, Springer BD (2018) Perioperative and modifiable risk factors for periprosthetic joint infections (PJI) and recommended guidelines. Curr Rev Musculoskelet Med 11:325–331
Anderson K, Hamm RL (2012) Factors that impair Wound Healing. J Am Coll Clin Wound Spec 4(4):84–91
Bloom GB, Mears SC, Edwards PK, Barnes CL, Stambough JB (2020) Total Knee Periprosthetic Joint Infection in the setting of hematologic malignancy: considerations for management. Arthroplast Today 6(3):309–315
Bozic KJ, Lau E, Kurtz S, Ong K, Berry DJ (2012) Patient-related risk factors for postoperative mortality and periprosthetic joint infection in medicare patients undergoing TKA. Clin Orthop Relat Res 470(1):130–137
Chang C-H, Lee S-H, Lin Y-C, Wang Y-C, Chang C-J, Hsieh P-H (2020) Increased periprosthetic hip and knee infection projected from 2014 to 2035 in Taiwan. J Infect Public Health 13(11):1768–1773
DeFrancesco CJ, Fu MC, Kahlenberg CA, Miller AO, Bostrom MP (2019) Extended antibiotic Prophylaxis May be linked to lower peri-prosthetic joint infection rates in high-risk patients: an evidence-based review. Hss j 15(3):297–301
Eka A, Chen AF (2015) Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Annals Translational Med, 3(16)
Gao Y-x, Ling X, Ye J-m et al (2010) Analysis of risk factors of surgical site infections in breast cancer. Chin Med J 123(5):559–562
Hardes J, von Eiff C, Streitbuerger A et al (2010) Reduction of periprosthetic infection with silver-coated megaprostheses in patients with bone sarcoma. J Surg Oncol 101(5):389–395
Hu W, Sung T, Jessen BA et al (2016) Mechanistic Investigation of Bone Marrow Suppression Associated with Palbociclib and its differentiation from cytotoxic chemotherapies. Clin Cancer Res 22(8):2000–2008
Kamath AF, Ong KL, Lau E et al (2015) Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplast 30(9):1492–1497
Kim HS, Park JW, Moon S-Y, Lee Y-K, Ha Y-C, Koo K-H (2020) Current and future burden of periprosthetic joint infection from national claim database. J Korean Med Sci, 35(49)
Kong L, Cao J, Zhang Y, Ding W, Shen Y (2017) Risk factors for periprosthetic joint infection following primary total hip or knee arthroplasty: a meta-analysis. Int Wound J 14(3):529–536
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplast 27(8):61–65 e61
Martin-Davila P, Blanes M, Fortun J (2007) Immunosuppression and infection in transplant recipients. Enferm Infecc Microbiol Clin 25(2):143–154
Muttana S, Solowiej Singh C, Kim H, Smith CJ, Michael MB (2021) The development of multiple Periprosthetic Joint infections in Conjunction with Ibrutinib Therapy. Cureus 13(12):e20639
Oncology NCCNNCPGi (2021) Prevention and Treatment of Cancer-Related Infections 1(ed)^(eds)
Parvizi J, Sullivan TA, Pagnano MW, Trousdale RT, Bolander ME (2003) Total joint arthroplasty in human immunodeficiency virus-positive patients: an alarming rate of early failure. J Arthroplast 18(3):259–264
Puhto T, Puhto A-P, Vielma M, Syrjälä H (2019) Infection triples the cost of a primary joint arthroplasty. Infect Dis 51(5):348–355
Racano A, Pazionis T, Farrokhyar F, Deheshi B, Ghert M (2013) High infection rate outcomes in long-bone tumor surgery with endoprosthetic reconstruction in adults: a systematic review. Clin Orthop Relat Res 471(6):2017–2027
Safdar A, Armstrong D (2011) Infections in patients with hematologic neoplasms and hematopoietic stem cell transplantation: neutropenia, humoral, and splenic defects. Clin Infect Dis 53(8):798–806
Salimy MS, Blackburn AZ, Alpaugh K, Lozano-Calderón SA, Bedair HS, Melnic CM (2023) Postoperative outcomes in total hip and total knee arthroplasty for patients who have multiple myeloma. The Journal of Arthroplasty
Sandiford NA, Franceschini M, Kendoff D (2021) The burden of prosthetic joint infection (PJI). Annals of Joint, 6
Sereda AP, Kochish AA, Cherny AA et al (2021) Epidemiology of hip and knee arthroplasty and Periprosthetic Joint Infection in Russian Federation. Traumatol Orthop Russia 27(3):84–93
Singh JA, Yu S, Chen L, Cleveland JD (2019) Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rhuematol 46(9):1134–1140
Taplitz RA, Kennedy EB, Bow EJ et al (2018) Antimicrobial prophylaxis for adult patients with Cancer-related immunosuppression: ASCO and IDSA Clinical Practice Guideline Update. J Clin Oncol 36(30):3043–3054
Xu Y, Huang TB, Schuetz MA, Choong PFM (2023) Mortality, patient-reported outcome measures, and the health economic burden of prosthetic joint infection. EFORT Open Rev. https://doi.org/10.1530/eor-23-0078
Yürekli A, Erbaş O (2021) Cancer and Immunosuppression. J Experimental Basic Med Sci 2(2):116–121
Zhu Y, Zhang F, Chen W, Liu S, Zhang Q, Zhang Y (2015) Risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. J Hosp Infect 89(2):82–89
Zuidhof R-JWJ, Löwik CAM, Ploegmakers JJW, Dijkstra SPD, Wouthuyzen-Bakker M, Jutte PC (2019) Periprosthetic joint infection in orthopaedic surgical oncology. Annals of Joint; Vol 4 (May 2019): Annals of Joint
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hoveidaei, A.H., Ghaseminejad-Raeini, A., Hosseini-Asl, S.H. et al. Initiating chemotherapy in joint arthroplasty patients increases the risk of periprosthetic joint infections. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05307-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05307-4