Abstract
Introduction
Patients recovering from musculoskeletal trauma have a heightened risk of opioid dependence and misuse, as these medications are typically required for pain management. The purpose of this meta-analysis was to examine the association between fracture type and chronic opioid use following fracture fixation in patients who sustain lower extremity trauma.
Materials and Methods
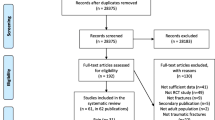
A meta-analysis was performed using PubMed and Web of Science to identify articles reporting chronic opioid use in patients recovering from surgery for lower extremity fractures. 732 articles were identified using keyword and MeSH search functions, and 9 met selection criteria. Studies were included in the final analysis if they reported the number of patients who remained on opioids 6 months after surgery for a specific lower extremity fracture (chronic usage). Logistic regressions and descriptive analyses were performed to determine the rate of chronic opioid use within each fracture type and if age, year, country of origin of study, or pre-admission opioid use influenced chronic opioid use following surgery.
Results
Bicondylar and unicondylar tibial-plateau fractures had the largest percentage of patients that become chronic opioid users (29.7–35.2%), followed by hip (27.8%), ankle (19.7%), femoral-shaft (18.5%), pilon (17.2%), tibial-shaft (13.8%), and simple ankle fractures (2.8–4.7%).Most opioid-naive samples had significantly lower rates of chronic opioid use after surgery (2–9%, 95% CI) when compared to samples that allowed pre-admission opioid use (13–50%, 95% CI). There were no significant associations between post-operative chronic opioid use and age, year, or country of origin of study.
Conclusions
Patients with lower extremity fractures have substantial risk of becoming chronic opioid users. Even the lowest rates of chronic opioid use identified in this meta-analysis are higher than those in the general population. It is important that orthopedic surgeons tailor pain-management protocols to decrease opioid usage after lower extremity trauma.







Similar content being viewed by others
References
Manchikanti L, Singh A (2008) Therapeutic opioids: a ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician 11(2):63–88
Benyamin R, Trescot AM, Datta S et al (2008) Opioid complications and side effects. Pain Physician 11(2):105–120. https://doi.org/10.1007/978-3-540-35423-9_14
Orfield NJ, Gaddis A, Russell KB, Hartman DW, Apel PJ, Mierisch C (2019) New long-term opioid prescription-filling behavior arising in the 15 months after orthopaedic surgery. J Bone Jt Surg. https://doi.org/10.2106/jbjs.19.00241
Rosenbloom BN, McCartney CJL, Canzian S, Kreder HJ, Katz J (2017) Predictors of prescription opioid use 4 months after traumatic musculoskeletal injury and corrective surgery: a prospective study. J Pain 18(8):956–963. https://doi.org/10.1016/j.jpain.2017.03.006
Flanagan CD, Wysong EF, Ramey JS, Vallier HA (2018) Understanding the opioid epidemic: factors predictive of inpatient and postdischarge prescription opioid use after orthopaedic trauma. J Orthop Trauma 32:E408–E414. https://doi.org/10.1097/BOT.0000000000001256
Goesling J, Moser SE, Zaidi B et al (2016) Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain 157(6):1259–1265. https://doi.org/10.1097/j.pain.0000000000000516
Sjberg C, Bladh L, Klintberg L, Mellstrm D, Ohlsson C, Wallerstedt SM (2010) Treatment with fall-risk-increasing and fracture-preventing drugs before and after a hip fracture: an observational study. Drugs Aging 27(8):653–661. https://doi.org/10.2165/11538200-000000000-00000
Simoni AH, Nikolajsen L, Olesen AE, Christiansen CF, Pedersen AB (2019) Opioid use after hip fracture surgery: a Danish nationwide cohort study from 2005 to 2015. Eur J Pain (UK) 23(7):1309–1317. https://doi.org/10.1002/ejp.1392
Finger A, Teunis T, Hageman MG, Ziady ER, Ring D, Heng M (2017) Association between opioid intake and disability after surgical management of ankle fractures. J Am Acad Orthop Surg 25(7):519–526. https://doi.org/10.5435/JAAOS-D-16-00505
Al-Dabbagh Z, Jansson KA, Stiller CO, Montgomery S, Weiss RJ (2016) Long-term pattern of opioid prescriptions after femoral shaft fractures. Acta Anaesthesiol Scand 60(5):634–641. https://doi.org/10.1111/aas.12666
Al-Dabbagh Z, Jansson KÅ, Stiller CO, Montgomery S, Weiss RJ (2014) No signs of dose escalations of potent opioids prescribed after tibial shaft fractures: a study of Swedish National Registries. BMC Anesthesiol 14:2–7. https://doi.org/10.1186/1471-2253-14-4
Rodriguez-Buitrago A, Attum B, Enata N et al (2018) Opioid prescribing practices after isolated pilon fractures. J Foot Ankle Surg 57(6):1167–1171. https://doi.org/10.1053/j.jfas.2018.06.010
Lindestrand AG, Christiansen MLS, Jantzen C, van der Mark S, Andersen SE (2015) Opioids in hip fracture patients: an analysis of mortality and post hospital opioid use. Injury 46(7):1341–1345. https://doi.org/10.1016/j.injury.2015.04.016
Rodriguez-Buitrago A, Attum B, Enata N et al (2019) Opiate prescribing practices after common isolated lower extremity injuries. J Orthop Trauma 33(3):e93–e99. https://doi.org/10.1097/BOT.0000000000001375
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Online) 339(7716):332–336. https://doi.org/10.1136/bmj.b2535
Sun EC, Darnall BD, Baker LC, MacKey S (2016) Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med 176(9):1286–1293. https://doi.org/10.1001/jamainternmed.2016.3298
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN (2014) Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ (Online) 348(February):1–10. https://doi.org/10.1136/bmj.g1251
Holman JE, Stoddard GJ, Higgins TF (2013) Rates of prescription opiate use before and after injury in patients with orthopaedic trauma and the risk factors for prolonged opiate use. J Bone Jt Surg Ser A 95(12):1075–1080. https://doi.org/10.2106/JBJS.L.00619
Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee GC (2017) Preoperative opiate use independently predicts narcotic consumption and complications after total joint arthroplasty. J Arthroplasty 32(9):2658–2662. https://doi.org/10.1016/j.arth.2017.04.002
Pryymachenko Y, Wilson RA, Abbott JH, Dowsey MM, Choong PFM (2020) Risk factors for chronic opioid use following hip and knee arthroplasty: evidence from New Zealand population data. J Arthroplasty 35(11):3099-3107.e14. https://doi.org/10.1016/j.arth.2020.06.040
Kim SC, Choudhry N, Franklin JM et al (2017) Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthrit Cartil 25(9):1399–1406. https://doi.org/10.1016/j.joca.2017.04.002
Inacio MCS, Hansen C, Pratt NL, Graves SE, Roughead EE (2016) Risk factors for persistent and new chronic opioid use in patients undergoing total hip arthroplasty: a retrospective cohort study. BMJ Open 6(4):1–10. https://doi.org/10.1136/bmjopen-2015-010664
Doverty M, White JM, Somogyi AA, Bochner F, Ali R, Ling W (2001) Hyperalgesic responses in methadone maintenance patients. Pain 90(1–2):91–96. https://doi.org/10.1016/S0304-3959(00)00391-2
Levy RS, Hebert CK, Munn BG, Barrack RL (1996) Drug and alcohol use in orthopedic trauma patients: a prospective study. J Orthop Trauma 10(1):21–27
Blake R, Brinker M, Ursic C, Clark J, Cox D (1997) Alcohol and drug use in adult patients with musculoskeletal injuries. Am J Orthop (Belle Mead NJ) 26(10):704–709
Massey GM, Dodds HN, Roberts CS, Servoss TJ, Blondell RD (2005) Toxicology screening in orthopedic trauma patients predicting duration of prescription opioid use. J Addict Dis 24(4):31–41
Lawrence J (2003) Tibial plafond fractures: how do these ankles function over time? J Bone Jt Surg Am 85:287–295
Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. http://journals.lww.com/jorthotrauma
Rodgers J, Cunningham K, Fitzgerald K, Finnerty E (2012) Opioid consumption following outpatient upper extremity surgery. J Hand Surg 37(4):645–650. https://doi.org/10.1016/j.jhsa.2012.01.035
Bicket MC, White E, Pronovost PJ, Wu CL, Yaster M, Alexander GC (2019) Opioid oversupply after joint and spine surgery: a prospective cohort study. Anesth Analg 128(2):358–364. https://doi.org/10.1213/ANE.0000000000003364
Kim N, Matzon JL, Abboudi J et al (2016) A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Jt Surg Am Vol 98(20):e89. https://doi.org/10.2106/JBJS.15.00614
Kumar K, Gulotta LV, Dines JS et al (2017) Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med 45(3):636–641. https://doi.org/10.1177/0363546517693665
Michigan opioid prescribing engagement network. Opioid prescribing recommendations.
Al Dabbagh Z, Jansson KÅ, Stiller CO, Montgomery S, Weiss RJ (2014) No signs of dose escalations of potent opioids prescribed after Tibial shaft fractures: a study of Swedish National Registries. BMC Anesthesiol 14:2–7. https://doi.org/10.1186/1471-2253-14-4
Lindenhovious ALC, Helmerhorts GTT, Schnellen AC, Vrahas M, Ring D, Kloen P (2009) Differences in prescription of narcotic pain medication after operative treatment of hip and ankle fractures in the United States and the Netherlands. J Trauma Injury, Infect Crit Care 67(1):160–164. https://doi.org/10.1097/TA.0b013e31818c12ee
Hooten WM, Sauver JLS, McGree ME, Jacobson D, Warner DO (2016) Incidence and risk factors for progression from acute to longer-term opioid prescribing: a population-based study. Mayo Clin Proc 116(8):1477–1490. https://doi.org/10.1161/circresaha.116.303790.The
Wiznia DH, Zaki T, Leslie MP, Halaszynski TM (2018) Complexities of perioperative pain management in orthopedic trauma. Curr Pain Headache Rep 22(9):1–9. https://doi.org/10.1007/s11916-018-0713-5
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Otwell, Blake, Cherney and Siegel declare that they have no financial interests. Author Stambough declares relationships with the American Association of Hip and Knee Surgeons as a Board Member, American Joint Replacement Registry (AJRR) as a Board Member, Journal of Arthroplasty as an Editorial Board Member, Signature Orthopaedics as receiving IP royalties and Smith & Nephew as a Paid consultant. Author Mears declares relationships with Delta Ortho LLC as having Stock Options, Fragility Fracture Network as a Board or committee member, Journal of the American Geriatrics Society as an Editorial or governing board member, and SAGE as an Editorial or governing board member.
Ethical approval
This manuscript is not submitted to more than one journal for simultaneous consideration. The submitted work is original and has not been published elsewhere in any form or language.
Informed consent
Our IRB deemed this study exempt from ethical approval as non-human subjects research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Otwell, A.G., Stambough, J.B., Cherney, S.M. et al. Does the type of lower extremity fracture affect long-term opioid usage? A meta-analysis. Arch Orthop Trauma Surg 144, 1221–1231 (2024). https://doi.org/10.1007/s00402-023-05174-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05174-5