Abstract
Introduction
This study aimed to evaluate the meniscal size of asymptomatic discoid lateral meniscus (DLM) and compare it with that of normal lateral meniscus (LM) and to compare changes in meniscal dimensions with age among patients with asymptomatic DLM and those with normal LM using magnetic resonance imaging (MRI).
Materials and methods
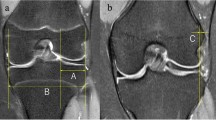
We retrospectively reviewed the medical records, including MRI data, of patients with asymptomatic DLM (DLM group) or normal LM (control group). Width and extrusion of both DLM and normal LM and tibial length were measured and compared using mid-coronal and mid-sagittal MR images. Meniscal size and sagittal and coronal meniscal ratio according to age, as well as differences between DLM and normal menisci, were also evaluated.
Results
Thirty-four knees were included in the DLM group, whereas the control group comprised of 50 patients. The DLM group showed significantly less meniscal extrusion, greater coronal width, posterior capsule distance, sagittal meniscal length, and sagittal meniscal ratio than the control group (DLM: 0.1 ± 0.3 mm, 23.3 ± 2.2 mm, 5.4 ± 2.4 mm, 25.1 ± 2.8 mm, 61 ± 6%, and control: 0.4 ± 0.4 mm, 9.5 ± 2.3 mm, 2.5 ± 1.2 mm, 30.2 ± 2.6 mm, 71 ± 4%, respectively). The coronal meniscal ratio decreased with age in both the control (p = 0.001) and DLM (p = 0.037) groups. The sagittal meniscal ratio (p = 0.001) and minimum height (p = 0.04) decreased and the anterior capsule distance (p = 0.035), posterior capsule distance (p = 0.026), and entire sagittal length (p = 0.005) increased with age in the DLM group, while the distance between the meniscal inner margins (p = 0.019) increased with age in the control group.
Conclusions
The meniscal ratio in the sagittal plane of the DLM group was significantly lower than that of the control group. The sagittal meniscal ratio of asymptomatic DLM decreased with age, indicating that the size of asymptomatic DLM does not change with age.
Level of evidence
III: Retrospective comparative study.




Similar content being viewed by others
Data availability
The data associated with this study is available from the corresponding author on reasonable request.
Change history
26 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00402-023-05157-6
References
Kim JH, Ahn JH, Kim JH, Wang JH (2020) Discoid lateral meniscus: importance, diagnosis, and treatment. J Exp Orthop 7(1):81
Tapasvi S, Shekhar A, Eriksson K (2021) Discoid lateral meniscus: current concepts. J ISAKOS 6(1):14–21
Tyler PA, Jain V, Ashraf T, Saifuddin A (2022) Update on imaging of the discoid meniscus. Skeletal Radiol 51(5):935–956
Restrepo R, Weisberg MD, Pevsner R, Swirsky S, Lee EY (2019) Discoid meniscus in the pediatric population: emphasis on MR imaging signs of instability. Magn Reson Imaging Clin N Am 27:323–339. https://doi.org/10.1016/j.mric.2019.01.009
Saavedra M, Sepúlveda M, Jesús Tuca M, Birrer E (2020) Discoid meniscus: current concepts. EFORT Open Rev 5(7):371–379
Hesse DG, Finlayson CJ, Gladstein AZ, Samet JD (2021) Pediatric discoid meniscus: can magnetic resonance imaging features coupled with clinical symptoms predict the need for surgery? Pediatr Radiol 51(9):1696–1704
Jung YJ, Choi SH, Ahn JH, Lee SA (2013) MRI findings with arthroscopic correlation for tear of discoid lateral meniscus: comparison between children and adults. Acta Radiol 54:442–447. https://doi.org/10.1177/0284185113475442
Yilgor C, Atay OA, Ergen B, Doral MN (2014) Comparison of magnetic resonance imaging findings with arthroscopic findings in discoid meniscus. Knee Surg Sports Traumatol Arthrosc 22:268–273
Bedoya MA, Barrera CA, Chauvin NA, Delgado J, Jaramillo D, Ho-Fung VM (2019) Normal meniscal dimensions at different patient ages-MRI evaluation. Skeletal Radiol 48(4):595–603
Kim SH, Lee JW, Kim KI, Lee SH (2021) Can an injured discoid lateral meniscus be returned to the correct anatomic position and size of the native lateral meniscus after surgery? Knee 28:25–35
Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL (2007) Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med 35:475–478 (28)
Cui JH, Min BH (2007) Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy 23:635–641
Ahn JH, Lee SH, Yoo JC, Lee HJ, Lee JS (2010) Bilateral discoid lateral meniscus in knees: evaluation of the contralateral knee in patients with symptomatic discoid lateral meniscus. Arthroscopy 26(10):1348–1356
Liu WX, Zhao JZ, Huangfu XQ, He YH, Yang XG (2015) Prevalence of bilateral Discoid Lateral Menisci (DLM) in patients operated for symptomatic DLM with a follow-up study on their asymptomatic contralateral knees: a Magnetic Resonance Imaging (MRI) assessment. BMC Musculoskelet Disord 16:172
Choi SH, Shin KE, Chang MJ, Woo SY, Lee SH (2013) Diagnostic criterion to distinguish between incomplete and complete discoid lateral meniscus on MRI. J Magn Reson Imaging. 38(2):417–421. https://doi.org/10.1002/jmri.23985
Samoto N, Kozuma M, Tokuhisa T, Kobayashi K (2002) Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging 20:59–64. https://doi.org/10.1016/s0730-725x(02)00473-3
Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS (2009) A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med 37:1564–1569. https://doi.org/10.1177/0363546509332502
Nishino K, Hashimoto Y, Tsumoto S, Yamasaki S, Nakamura H (2021) Morphological changes in the residual meniscus after reshaping surgery for a discoid lateral meniscus. Am J Sports Med 49(12):3270–3278. https://doi.org/10.1177/03635465211033586
Kim SH, Ahn J, Kim TW, Kim KI, Lee SH (2019) Midbody of the medial meniscus as a reference of preservation in partial meniscectomy for complete discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc 27(8):2558–2567
Choi YH, Seo YJ, Ha JM, Jung KH, Kim J, Song SY (2017) Collagenous ultrastructure of the discoid meniscus: a transmission electron microscopy study. Am J Sports Med 45(3):598–603. https://doi.org/10.1177/0363546516674181
Papadopoulos A, Kirkos JM, Kapetanos GA (2009) Histomorphologic study of discoid meniscus. Arthroscopy 25(3):262–268
Klingele KE, Kocher MS, Hresko MT et al (2004) Discoid lateral meniscus: prevalence of peripheral rim instability. J Pediatr Orthop 24:79–82. https://doi.org/10.1097/00004694-200401000-00015
Good CR, Green DW, Griffith MH, Valen AW, Widmann RF, Rodeo SA (2007) Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy 23:157–163. https://doi.org/10.1016/j.arthro.2006.09.002
Hashimoto Y, Nishino K, Reid JB 3rd et al (2020) Factors related to postoperative osteochondritis dissecans of the lateral femoral condyle after meniscal surgery in juvenile patients with a discoid lateral meniscus. J Pediatr Orthop 40:e853–e859. https://doi.org/10.1097/bpo.0000000000001636
Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H (2017) Risk factors associated with knee joint degeneration after arthroscopic reshaping for juvenile discoid lateral meniscus. Am J Sports Med 45:570–577. https://doi.org/10.1177/0363546516668623
Yoo WJ, Lee K, Moon HJ, Shin CH, Cho TJ, Choi IH, Cheon JE (2012) Meniscal morphologic changes on magnetic resonance imaging are associated with symptomatic discoid lateral meniscal tear in children. Arthroscopy 28(3):330–336. https://doi.org/10.1016/j.arthro.2011.08.300
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
YH: conception and design, drafting of the article. KN: drafting of the article, and acquisition of the data. TK: interpretation of data. KI: drafting of the article, analysis of the data. HN: conception and design, final approval of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest in this study.
Ethical approval
Institutional Review Board/Ethics Committee approval number: 2727.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hashimoto, Y., Nishino, K., Kinoshita, T. et al. Age-based comparison of meniscal dimensions between an asymptomatic complete discoid lateral meniscus and normal meniscus: MRI evaluation. Arch Orthop Trauma Surg 144, 791–798 (2024). https://doi.org/10.1007/s00402-023-05084-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05084-6