Abstract
Objective
There are scarce data on the mortality after hip fracture surgery for patients treated in the most recent years. The objective of this study was to analyze whether the overall initiatives introduced over the last decade for elderly patients with hip fractures had a positive impact on the 1-year mortality.
Methods
Patients treated during 2010–2012 were compared with patients treated during 2018–2020 for all-cause 1-year mortality. Variables influencing mortality were collected based on the literature, including demographic, comorbidity, cognitive status, and preinjury physical function. Crude mortalities were compared between periods, as well as with the expected mortality in the general population adjusted for age, gender, and year of surgery using the standardized mortality ratio (SMR). A multivariate model was used to identify mortality risk factors.
Results
591 patients older than 65 years were treated during 2010–2012 and 642 patients during 2018–2020. The mean age increased significantly between periods (78.9 vs. 82.6 years, respectively, p = 0.001) in both genders, together with an increase in comorbidity (p = 0.014). The in-hospital mortality risk had no significant difference between periods (2.5 vs. 2.0%, p = 0.339), but the 30-day mortality risk (8.3 vs. 5.5%, p = 0.031) and 1-year mortality risk (16.1 vs. 11.9%, p = 0.023) declined significantly. However, 1-year mortality in 2020 had an excess of 1.33 in SMR. Age older than 80 years, male gender, and Charlson comorbidity index > 2 were significant predictors of 1-year mortality.
Conclusion
The important evolution achieved in the last decade for the management of patients with hip fracture surgery has led to a significant decline in 1-year mortality, but the 1-year mortality remains significantly higher compared to the general population of similar age and gender.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures remain associated with high mortality in the elderly population, and they represent an important public health concern with significant financial cost implications [1]. During the last decades, advances in anesthesia and surgical procedures emerged with the aim of reducing surgical mortality risks. However, as older patients and with more comorbidities are currently undergoing surgery, the postoperative complications and especially mortality risk remain a serious concern [2].
Despite these advances, the 1-year mortality after hip fracture surgery is reported as high as 29% [3], which represented an excess 3–4 times higher than expected in the general population [4]. Few studies on secular trends and changes in excess mortality after hip fractures over time are available and the results are conflicting [3, 5, 6]. While some studies reported no significant mortality risk changes from1960 to 2000 in United Kingdom [3] and from 2000 to 2014 in Denmark [5], other more recent study found a significant decline from 2000 and 2016 in Italy [6]. Most of these large studies were based on national registries that included all patients with hip fracture older than 18 or 50 years [5, 7]. On the other hand, most studies available reported trends for mortality after hip fracture including historical cohorts of the 1990s or data from patients treated before 2005, and they do not consider that care has evolved in the last 10 years [3].
With the implementation in the last decade of specific hip fracture pathways [8], such as early surgery, preoperative optimization of patients at higher risk and multi-disciplinary team between surgeons and geriatricians for perioperative and postoperative cares of these elderly patients [9], one would argue that there would probably be an improvement in morbidity and mortality risks. However, data on recent trends in mortality after hip fracture surgery are scarce. Only some studies have focused on patients treated in the last years. Trevisan et al. [6] reported no significant change in 1-year mortality from 2000 to 2016. Likely, Gjertsen et al. [10] reported no significant change from 2005 to 2014, and Kjaervik et al. [11] found small survival differences from 2014 to 2018. Conversely, Nordstrom et al. [12] reported that short-term mortality increased during 1998–2017. Thus, there is scarce evidence on the postoperative mortality or whether the difference in mortality between hip fracture patients and the general population has changed over the last decade.
The objective of this study was to investigate if there was any change in mortality over the last decade. The hypothesis was that improvement in mortality should have occurred.
Materials and methods
A prospective registry-based observational cohort study was performed after approval by the institutional ethics committee. Informed consent was not required as it was performed on available anonymized data. The level-I trauma department database at our regional public hospital prospectively collected patient data from admission to 1-year postoperatively.
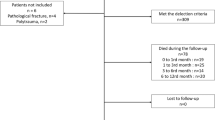
To analyze the mortality trend during the last decade, two periods of three consecutive years each were compared: 2010–2012 and 2018–2020. Patients admitted for hip fracture in these periods were identified from the departmental database. The inclusion criteria were diagnosis of proximal femoral fracture, age 65 years or older, and surgical treatment. For patients with subsequent hip fracture during the study period, only the first fracture was included for study. The exclusion criteria were patients treated with a conservative approach (usually decision to palliative care), pathological fracture (metastasis), and multiple trauma. Patients who were tested positive for an infection by the SARS-CoV-2 virus were also excluded.
During the last 5 years (2016–2020), a co-management of elderly patients between orthopedic surgeons and geriatricians was used from admission to 30-day after discharge. Our strategy for hip fracture was to perform surgery as early as possible, within 48 h from the trauma. All surgeries were performed under spinal anesthesia. Trochanteric fractures were treated with sliding hip screw or intramedullary trochanteric nail when a more stable construct was required, subtrochanteric fractures with locked long intramedullary nail, and cervical fractures with hemiarthroplasty or total hip arthroplasty (usually for active patients under 70 years of age). Postoperative rehabilitation was carried out with the assistance of a physiotherapist, and usually began within 24 h after surgery with mobilization out of bed to a chair. Progressive full weight-bearing with walker was authorized at 48 postoperative day if they tolerated.
Follow-up and evaluations
All patients were evaluated at admission and up to 1 year postoperatively. The primary outcome was the postoperative all-cause mortality over time (in-hospital, at 30 days, and at 1 year). Our center is linked to all primary healthcare centers, remaining hospitals of our country, and the national mortality register. Data from these different sources could be combined using the unique personal identification number of each citizen, and it is possible to construct the complete medical history for each patient and to identify admission in other outside hospitals.
Variables influencing mortality were collected based on the literature [2, 9] including gender, body mass index (BMI), fracture type (cervical or trochanteric), and time to surgery after admission. Age was also categorized into two groups: 65–79 years and 80 or over. Comorbidity at admission was assessed by the American Society of Anaesthesiology (ASA) (I–II, low risk; III–IV, high risk) [13], and the Charlson comorbidity index (≤ 2 low risk, > 2 high risk) [14]. Cognitive status at admission was measured by the Hodkinson's abbreviated mental test 0–10 score, where six or less suggested dementia [15]. Preinjury physical function was assessed using the Katz Index [16] for activities of daily living (ADL), where full independence was defined as the ability to do all six ADL without assistance, partial dependence as the ability to do four or five activities without assistance, and total dependence as the ability to do three activities or fewer without assistance.
Statistical analysis
Statistical analyses were conducted with SPSS v. 21 software (IBM, Armonk, USA). A p value of 0.05 or less was considered as significant. Kolmogorov–Smirnov tested normal distribution. All variables had a non-Gaussian distribution, and only nonparametric tests were used. Categorical data were analyzed by Fischer’s exact test or Mantel–Haenszel test, and continuous variables by Mann–Whitney test. Independent factors influencing mortality were analyzed by Cox proportional hazards regression models. In the models, significant covariates in univariate analyses were entered, as well as those suggested by the literature as potential predictors. Risks were presented as hazard ratio (HR) with 95% confidence interval (CI).
Crude 1-year mortality was expressed as proportion (%), and also compared with the expected mortality based on the general population adjusted for age, gender, and year of surgery. This last outcome was expressed as the standardized mortality ratio (SMR, ratio of observed to expected deaths) with 95% CI. An SMR > 1 indicated an observed mortality higher than expected. Mortality tables from the National Institute of Statistics were used to determine the expected mortality [17].
Results
Patient characteristics
There were 1233 patients who met the criteria. The 2010–2012 cohort was composed of 591 patients, and 2018–2020 of 642 patients. Baseline characteristics of both cohorts are shown in Table 1. There was a significant higher proportion of females throughout the period studied (p = 0.023), with an increment of males in 2018–2020. In this last period, the mean age increased significantly in both genders (p = 0.001) with a significant increase in the proportion of patients older than 80 years (p = 0.033). Likewise, there was a significant increase in comorbidities according to the Charlson index (p = 0.042), and ASA showed a significant higher proportion of class III–IV patients (p = 0.023) in 2018–2020 compared with 2010–2012. On the other hand, the proportion of patients operated within 48 h after admission was significantly higher in 2018–2020 (p = 0.029). Overall, the commonest comorbidities were arterial hypertension (65%), heart failure (27%), diabetes (29%), chronic pulmonary disease (14%), cerebrovascular disease (9%), cancer (8%), hypothyroidism (4%), chronic renal disease (4%), and Parkinson (3%).
Mortality analysis
The commonest causes of death throughout the study period were pneumonia (31%) and cardiac failure (22%), without substantial differences between both periods. Comparing 2010–2012 and 2018–2020 cohorts with univariate analyses (Table 2), the in-hospital mortality risks were 2.5% and 2.0%, respectively (p = 0.339), but 30-day (8.3% and 5.5%, p = 0.031) and 1-year (16.1% and 11.9%, p = 0.023) mortalities declined significantly. The cumulative 30-day mortality risk declined significantly in females from 8.8% in 2010–2012 to 5.5% in 2018–2020 (p = 0.040), in patients older than 80 years from 19.2 to 12.3%, respectively (p = 0.042), and for ASA III–IV patients from 24.3 to 13.7% (p = 0.003), but not in males (p = 0.341). The cumulative 1-year mortality risk declined significantly from 16.2% in 2010–12 to 10.4% in 2018–20 in females (p = 0.009), and ASA III–IV patients from 31.2 to 20.3%, respectively (p = 0.006), but there were no significant differences between the two periods in males (p = 0.545) or patients older than 80 years (p = 0.053). There were no significant differences between fracture types at any postoperative time analyzed (all p > 0.05).
In multivariate analysis (Table 3), the only significant predictor of in-hospital mortality was ASA III–IV in both studied periods (p = 0.021 in 2010–12, and 0.048 in 2018–20), but it is to be noted that the Charlson index > 2 was not a predictor in either period (p = 0.321 and 0.425, respectively). For 30-day mortality, multivariate analysis showed in both 2010–12 and 2018–20 periods that male gender (p = 0.028 and 0.016, respectively), age older than 80 years (p = 0.008 and 0.037, respectively), and ASA category III–IV (p = 0.025 and 0.017, respectively) were significant predictors, although the Charlson index was not significant (p = 0.076 and 0.059, respectively). In multivariate analysis for 1-year mortality, male gender (p = 0.022 in 2010–12, and 0.038 in 2018–20), age older than 80 years p = 0.009 and 0.031, respectively), and Charlson index > 2 (p = 0.041 and 0.040, respectively) were significant predictors, but not ASA category III–IV (p = 0.082 and 0.377, respectively). Despite the significant declines in 30-day and 1-year mortalities from 2010–12 to 2018–20, there was no improvement compared with the mortality in the general population of similar gender and age (Table 4). Based on the standardized reference population, the observed 1-year mortality risks during 2010–12 (SMR 1.51, 95% CI 1.17–1.89) and 2018–20 (SMR 1.33, 95% CI 1.25–1.61) were higher than expected in the same periods.
Discussion
The initiatives introduced during the last decade to improve the care of elderly patients with hip fractures, especially co-management with geriatricians and shorter time to surgery, have had a positive impact on mortality within 1-year postoperatively. However, the postoperative survival in these patients is still lower than in the general population of similar age and gender.
A significant decrease over time of the in-hospital mortality has been reported in the literature, from 12% in the 1990s [18] to 3.5%–4.7% in the 2000s [19]. The in-hospital mortality in the present study agrees with the risk about 2% reported currently [20], and female gender was not a significant predictor, while female was significant in the cohort by Forni et al. [20]. A recent meta-analysis [21] indicated reduced mortality for patients operated within 24 h compared with those operated within 36 h. Contrary, other recent study [22]) reported that early surgery within 48 and 72 h was significantly associated with a lower in-hospital mortality in patients older than 85 years. In a prior study [23], we found that patients with severe active comorbidities could benefit from surgery delayed more than 2 days. On the other hand, the co-management between surgeons and geriatricians has showed a significant reduction of the in-hospital mortality [24].
The in-hospital mortality risk remained unchanged over the last decade, and this was influenced by older mean age and more patients with comorbidities and high surgical risk as measured by the ASA in the last 3 years studied. However, significant improvements in mortality at 30-day and 1-year postoperatively were observed in the present study. Age and male gender influenced mortality, although the proportion of patients older than 80 years were gradually highest. Moreover, together with an increase over time in age there was also an increase in patient comorbidity. It is to be noted that the comorbidity as measured by the ASA was a mortality predictor at in-hospital and 30 days, but not at 1 year. On the contrary, comorbidity measured by the Charlson index was a predictor of 1-year mortality. This could be because the ASA assesses comorbidity for an immediate surgical risk, while the Charlson index assesses health status with respect to concomitant chronic diseases that can worsen over time. The improvement in 30-day mortality over the last decade was likely the result of better clinical perioperative management and faster regain of weight-bearing, and the improvement in 1-year mortality was the result of an improvement in the care for these patients in the public health system.
The evolution over time of 30-day mortality is controversial in the literature. A Danish trend study found no significative change in 30-day mortality between 1980 and 1990 [7], with a risk of 9%, while other Danish study based on national registry reported similar risk of 9% between 2000 and 2014 [5]. Contrary, a recent study on the Swedish national registry [12] found the 30-day mortality increased between 1998 and 2017 from 4.3% to 6.2% in women and from 8.4 to 11.1% in men, which was attributed to the fact that the length of stay had decreased. The most recent studies found a decline from 12 to 7% between 2000 and 2016 [6], and risks between 2018 and 2020 ranged from 5 to 7% [20]. An English report found a 30-day mortality risk of 1.2% during 2009–10 [25]. Like us, some of these more recent studies reported a higher 30-day mortality risk in males compared with females between 2010 and 2017 [11, 24, 26], while others found that male was not significant predictor in 2014 [20]. In the present study, the 30-day mortality decreased significantly from 2010 to 2020, despite an increase over time in the mean age of patients and their comorbidities.
In most studies of patients treated in past and recent decades, 1-year mortality remained unchanged despite multi-disciplinary cares [27]. In the present study, 1-year mortality significantly declined over the last decade, and the risk at 1 year was substantially lower than those reported in past decades [6, 28]. The 1-year mortality is high over time in the literature, with risks about 29% in the 1960s [3], 23% in the 1980s [29], and 26% in the 1990s [7, 28]. In the most recent studies, no significant changes in the last 20 years have been reported with risks maintained about 22% [2, 6, 11]. Like us, the most common predictors reported were male, age > 80 years, and Charlson index > 2 [30]. Nevertheless, mortality risks are influenced by various factors. Kjaerevik et al. [11] included 18 factors in a study of mortality after hip fracture. Sheehan et al. [31] identified 39 patient-factors that could be associated with mortality after hip fracture. Compared with the general population of similar age and gender, hip fracture patients had 1-year mortality risk 16 times higher in females, and 12 times higher in males during the 1990s [32], with a SMR of 2.4 increased risk in females and 3.5 in males in 2010 [33], and of 3.5 for both genders in 2018 [11]. However, this decrease did not translate into increased survival as compared with that in the general population of similar gender and age. SMR showed a higher mortality risk over the last decade, of 1.91 in 2010 and 1.84 in 2020, which was not a substantial difference. The higher relative excess mortality at 1-year after hip fracture, as compared with the general population, probably reflects the frailty and multi-morbidity in the elderly patients who sustain a hip fracture.
To our knowledge, this is the study to analyze mortality change over time after hip fracture in elderly patients using more recent patient cohorts. Although this was a retrospective study, perioperative data had been collected prospectively without the problem of variable completeness of reporting of population-based or administrative register studies. However, the study has several limitations. The sample of patients was relatively small as it was based on a single hospital. However, the sample was representative of patients treated in routine clinical practice, there were a complete follow-up of patients without loss of their data, and reliable identification of deaths. On the other hand, the results of this single institution study may not be extrapolated to other populations, since mortality may be associated with multiple factors including lifestyle, socio-economic status and facilities to live at a nursing home. A recent study [34] found that 30-day mortality varied from 5 to 9% among 32 public hospitals in the same country. The authors suggested that this could be due to a varied adherence to current clinical guidelines.
In conclusion, the important evolution achieved in the last decade for the management of patients with hip fracture surgery has led to a significant decline in 1-year mortality, but the 1-year mortality remains significantly higher compared to the general population of similar age and gender.
Data availability
Data are available by requesting the corresponding author.
References
Hommel A, Ulander K, Bjorkelund KB, Norrman PO, Wingstrand H, Thorngren KG (2008) Influence of optimised treatment of people with hip fracture on time to operation, length of hospital stay, reoperations and mortality within 1 year. Injury 39:1164–1174
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture: a systematic review. World J Orthop 10:166–175
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39:1157–1163
Finnes TE, Meyer HE, Falch JA, Medhus AW, Wentzel-Larsen T, Lofthus CM (2013) Secular reduction of excess mortality in hip fracture patients >85 years. BMC Geriatr 13:25
Gundel O, Thygesen LC, Gögenur I, Ekeloef S (2020) Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop 91:58–62
Trevisan C, Gallinari G, Carbone A, Klumpp R (2021) Fifteen years change in acute management of hip fracture patients: 1-year mortality calls for improvements. Injury 52:2367–2372
Giversen IM (2007) Time trends of mortality after first hip fractures. Osteoporos Int 18:721–732
Scottish Hip Fracture Audit (2021) Scottish standards of care for hip fracture patients 2020. https://www.shfa.scot.nhs.uk/Quality-Improvement/index.html. Accessed 26 June 2021
Moyet J, Deschasse G, Marquant B, Mertl P, Bloch F (2019) Which is the optimal orthogeriatric care model to prevent mortality of elderly subjects post hip fractures? A systematic review and meta-analysis based on current clinical practice. Int Orthop 43:1449–1454
Gjertsen JE, Dybvik E, Furnes O, Fevang JM, Havelin LI, Matre K et al (2017) Improved outcome after hip fracture surgery in Norway. Acta Orthop 88:505–511
Kjaervik C, Gjertsen JE, Stensland E, Saltyte-Benth J, Soereide O (2022) Modifiable and non-modifiable risk factors in hip fracture mortality in Norway, 2014 to 2018: a linked multiregistry study. Bone Jt J 104-B:884–893
Nordstrom P, Bergman J, Ballin M, Nordström A (2022) Trends in hip fracture incidence, length of hospital stay, and 30-day mortality in sweden from 1998–2017: a nationwide cohort study. Calcif Tissue Int 111:21–28
American Society of Anesthesiologists (2017) Relative value guide 2017. http://www.asahq.org. Accessed 26 June 2017
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Hodkinson HM (1972) Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 4:233–238
Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychological function. JAMA 185:914–919
Instituto Nacional de Estadística (2021). España, Tablas de mortalidad Comunidad Valenciana. http://www.ine.es/jaxi/tabla.do. Accessed 26 June 2022
Wu TY, Jen MH, Bottle A, Liaw CK, Aylin P, Majeed A (2011) Admission rates and in-hospital mortality for hip fractures in England 1998 to 2009: time trends study. J Public Health 33:284–291
Maravic M, Taupin P, Landais P, Roux C (2011) Decrease of inpatient mortality for hip fracture in France. Joint Bone Spine 78:506–509
Forni C, Gazineo D, D’Alessandro F, Fiorani A, Morri M, Sabattini T et al (2019) Predictive factors for thirty day mortality in geriatric patients with hip fractures: a prospective study. Int Orthop 43:275–281
Welford P, Jones CS, Davies G, Kunutsor SK, Costa ML, Sayers A et al (2021) The association between surgical fixation of hip fractures within 24 hours and mortality: a systematic review and meta-analysis. Bone Jt J 103:1176–1186
De Luca A, Murena L, Zanetti M, De Colle P, Ratti C, Canton G (2022) Should the early surgery threshold be moved to 72 h in over-85 patients with hip fracture? A single-center retrospective evaluation on 941 patients. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04509-y
Lizaur-Utrilla A, Gonzalez-Navarro B, Vizcaya-Moreno MF, Miralles Muñoz FA, Gonzalez-Parreño S, Lopez-Prats FA (2019) Reasons for delaying surgery following hip fractures and its impact on one year mortality. Int Orthop 43:441–448
Kusen JQ, Schafroth B, Poblete B, van der Vet PCR, Link BC, Wijdicks FJG et al (2019) The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: an observational study. Arch Orthop Trauma Surg 139:1705–1712
Sheikh HQ, Alnahhal A, Aqil A, Hossain FS (2021) Length of hospital stay following hip fracture and risk of 30 and 90 day mortality in a United Kingdom cohort. Acta Orthop Belg 87:607–617
Ahman R, Siverhall PF, Snygg J, Fredrikson M, Enlund G, Bjornström K et al (2018) Determinants of mortality after hip fracture surgery in Sweden: a registry- based retrospective cohort study. Sci Rep 24(8):15695
Civinini R, Paoli T, Cianferotti L, Cartei A, Boccaccini A, Peris A, Brandi ML et al (2019) Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit.” Int Orthop 43:187–192
Jantzen C, Madsen CM, Lauritzen JB, Jørgensen H (2018) Temporal trends in hip fracture incidence, mortality, and morbidity in Denmark from 1999 to 2012. Acta Orthop 89:170–176
Mundi S, Pindiprolu B, Simunovic N, Bhandari M (2014) Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop 85:54–59
Giummarra MJ, Ekegren CL, Gong J, Simpson P, Cameron PA, Edwards E et al (2020) Twelve month mortality rates and independent living in people aged 65 years or older after isolated hip fracture: a prospective registry-based study. Injury 51:420–428
Sheehan KJ, Sobolev B, Chudyk A, Stephens T, Guy P (2016) Patient and system factors of mortality after hip fracture: a scoping review. BMC Musculoskelet Disord 17:166
Roberts SE, Goldacre MJ (2003) Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98: database study. BMJ 327:771–775
Klop C, Welsing PM, Cooper C, Harvey NC, Elders PJ, Bijlsma JW et al (2014) Mortality in British hip fracture patients, 2000–2010: a population-based retrospective cohort study. Bone 66:171–177
Kristensen PK, Merlo J, Ghith N, Leckie G, Johnsen SP (2019) Hospital differences in mortality rates after hip fracture surgery in Denmark. Clin Epidemiol 16(11):605–614
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Elda University Hospital, Miguel Hernandez University (Date 27/11/2021 / No PI2021-167).
Consent to participate
Informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miralles-Muñoz, F.A., Perez-Aznar, A., Gonzalez-Parreño, S. et al. Change in 1-year mortality after hip fracture surgery over the last decade in a European population. Arch Orthop Trauma Surg 143, 4173–4179 (2023). https://doi.org/10.1007/s00402-022-04719-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04719-4