Abstract
Background
Hip fractures in the elderly population are common and the number of patients is rising. For young and geriatric patients with undisplaced fractures osteosynthesis is the primary type of treatment. The dynamic hip screw (DHS) is around for many years and proved its value especially in displaced fractures. Since 2018 the femoral neck system (FNS) is available as an alternative showing promising biomechanical results. The aim of this study is to evaluate clinical results of the FNS and compare it to the DHS.
Materials and methods
Patients older than 18 years with Garden I–IV fractures that were treated with osteosynthesis in a level 1 trauma center were included in the study. Between January 2015 and March 2021, all patients treated with FNS (1-hole plate, DePuy-Synthes, Zuchwil, Switzerland) or DHS (2-hole plate, DePuy-Synthes, Zuchwil, Switzerland) for proximal femur fractures were included in the study. Closed reduction was achieved using a traction table. All operations were carried out by experienced orthopedic trauma surgeons. Primary outcome measures were rate of implant failure (cut out) and surgical complications (hematoma, infection). Secondary outcome measures were Hb-difference, length of hospital stay and mortality.
Results
Overall, 221 patients were included in the study. 113 were treated with FNS, 108 with DHS. Mean age was 69 ± 14 years. There were 17.2% Garden I, 47.5% Garden II, 26.7% Garden III and 8.6% Garden IV fractures. No difference between the groups for age, body mass index (BMI), Charlson comorbidity index (CCI), time to surgery, Pauwels and Garden classification, rate of optimal blade position or tip apex distance was found. FNS showed lower pre- to postoperative Hb-difference (1.4 ± 1.1 g/l vs. 2.1 ± 1.4 g/l; p < 0.05), shorter operating time (36.3 ± 11.6 min vs. 54.7 ± 17.4 min; p < 0.05) and hospital stay (8.8 ± 4.3 d vs. 11.2 ± 6.8 d; p < 0.05). Surgical complications (FNS 13.3% vs. DHS 18.4%, p > 0.05), rate of cut out (FNS 12.4% vs. DHS 10.2%, p > 0.05) and mortality (FNS 3.5%; DHS 0.9%; p > 0.05) showed no difference between the groups. Logistic regression showed that poor blade position was the only significant predictor for cut out and increased the risk by factor 7. Implant related infection (n = 3) and hematoma/seroma (n = 6) that needed revision was only seen in DHS group.
Conclusion
FNS proved to be as reliable as DHS in all patients with hip fractures. Not the type of implant but blade positioning is still key to prevent implant failure. Still due to minimal invasive approach implant related infections and postoperative hematomas might have been prevented using the FNS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background/introduction
The number of hip fracture patients is predicted to increase and will range between 7.3 and 21.3 million by the year 2050 [1]. In Germany, for example cases increased by 23% from 2009 to 2019 with a ratio of 18/82 for under and over 70 year old patients [2]. While young patient suffer from high energy trauma like traffic accidents, hip fractures in older patients are mainly caused by ground level falls [3]. Surgical treatment options are osteosynthesis, arthroplasty and rarely conservative treatment [4]. Despite modern implants complication rate and mortality is still high [5,6,7]. Most commonly used implants are three cancellous compression screws (CCS) and the dynamic hip screw (DHS) which showed better results in dislocated and lateral fractures and lesser rate of implant removal [8]. Since 2018 the femoral neck system (FNS; DePuy-Synthes, Zuchwil, Switzerland) was introduced showing promising biomechanical results [9, 10]. Comparative studies evaluating the clinical outcome are still limited. The aim of this study was to evaluate the outcome of patients of all ages treated with the femoral neck system and compare it to patients treated with the dynamic hip screw.
Methods
Institutional and prior ethical committee approval for the use of data in this study was obtained.
All patients over 18 years with a hip fracture type Garden I–IV that were treated in a level 1 trauma center between January 2015 and March 2021 were retrospectively reviewed. Exclusion criteria were patients with pathologic fractures and patients treated with arthroplasty. Osteosynthesis was used mainly in patients under 65 years following current guidelines [4]. In patients over 65 osteosynthesis was used in Garden I and II fractures and also in a low number of cases in Garden III or IV fractures if the patient was in poor general condition. Until July 2018 only DHS-Blades were used. Starting August 2018 DHS was replaced with the femoral neck system. A traction table was used to achieve closed reduction. None of the cases needed open reduction. FNS and DHS was implanted following AO principles through six different experienced trauma surgeons all of them using both implants. The majority of the patient were mobilized on the first postoperative day with full weight bearing. Weight bearing was only restricted in a few young patients with Garden III and IV fractures that had the capability of partial weight bearing. Postoperative X-rays anterior–posterior and lateral were performed postoperative, after 14 days, 6 weeks and 3 months.
All fractures were classified using the AO/OTA Fracture and Dislocation classification, Garden and Pauwels classification. Blade positioning and tip apex distance was measured by an independent observer in the intraoperative X-rays which were performed in perfect ap and lateral view. For signs of implant failure (cut out) all postoperative X-rays were reviewed. In the 3 month controls the shortening of the femoral neck was measured. Patient charts were reviewed to detect further surgical complications like implant related infections or hematoma/seroma which needed revision surgery.
Primary outcome measures were implant failure and surgical complications. Secondary outcome measures were hemoglobin difference pre- to postoperative and length of hospital stay. Data analysis was performed with IBM SPSS Statistics (V21.0) and Microsoft Excel (V16.3). Demographic characteristics are described as mean and standard deviation. For the primary outcome measures, logistic regression was performed considering all variables related implant failure and surgical complications.
Results
Patient population
For 221 patients, medical records were reviewed. Out of these 221 patients, 109 were male and 112 were female. The youngest patient was 20, while the oldest was 98 years old. The mean age was 69.5 ± 15.4 years and did not differ between the groups (DHS 68.5 ± 15.1; FNS 66.6 ± 21.5; p > 0.05). 19 patients were preoperatively classified as ASA I, 46 as ASA II, 127 as ASA III and 29 as ASA IV. The DHS was used in 108 cases, FNS in 113 cases. Mean follow-up was 13 months. Time to surgery was approximately 14 h for both groups. There was no significant difference between the groups for age, sex, BMI, ASA classification, Charlson comorbidity index or time to surgery.
Fracture classification
All fractures were classified according to the AO classification. There was a significant difference within the groups with twice the number of patients with 31-B3 fractures in the DHS group. There were slightly more patients that were treated for dislocated Garden III and IV fractures in FNS group. Using Pauwels classification there were 39 Grade III fractures in DHS group and 40 in FNS group. There was no difference between the groups for Pauwels and Garden classification. Detailed classification is shown in Table 1.
Perioperative factors
There was a significant difference between the groups for operating time and Hb-difference. Operating time was approximately 18 min shorter and Hb-difference 0.7 g/dl lower in FNS group. The rate of optimal blade position (center–center und inferior–center) and tip apex distance showed no difference between the groups. Center–center or inferior–center position could be achieved in more than 87% of the cases. Mean tip apex distance was less than 25 mm in both groups.
Cut out and surgical complications
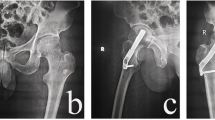
Femoral neck compression showed no difference between the groups and exceeded 5 mm in 27.6% of all cases. The rate of surgical complications showed no significant difference between the groups. In the DHS group there were 11 cut outs, 3 implant related infections and 6 patients with hematoma. All infections were successfully treated with multiple local debridement and antibiotics keeping the implant. In FNS group there were 14 cut outs and 1 hematoma. Implant failure occurred 12 times at the side of the blade and 2 time at the 1-hole plate (Fig. 1). Both implants allowed a comparable mean femoral neck shortening of 5 mm over 3 months. Logistic regression showed that the only significant factor for cut out in both groups was blade positioning. If the blade was not positioned center–center or inferior–center, the risk of cut out increased by factor 7. In the FNS group cut out occurred significantly more often in Pauwels III fracture (p < 0.05). High age was no significant predictor of implant failure. Overall 52 patients older than 60 years were treated with FNS or DHS for Garden III and IV fractures. Out of this geriatric cohort only eight (15.3%) patients showed mechanical failure. In the majority of cases with implant failure implant removal and arthroplasty was performed. In two young patients implant removal and reosteosynthesis was performed. In one geriatric patient due to the poor general condition only the implant was removed. Intraoperative factors of all 25 cut out cases are shown in Table 2.
Discussion
In this clinical study, the FNS proved to be an alternative in the treatment of hip fractures compared to DHS. Previous biomechanical studies showed comparable results for FNS compared with DHS and an increased stability compared to three screws [9] or Hansson Pins [10]. Chang-Ho et al. showed that center–center blade positioning and low tip apex distance will increase the stability of the FNS [11]. A finite element study from Fan et al. showed increased stability of the FNS compared to 3 screws but also a higher stability for the 2-hole plate in if the fracture angle exceeded 70° [12]. There are only a few clinical studies evaluating the clinical use of the FNS. Stassen et al. showed for 34 patients’ surgical complications in 23.5% [13]. Yan et al. evaluated 24 patients with FNS compared to 58 patients with CCS showing a surgical complications rate of 8.3% in the FNS group [14]. In the 47 patients treated with FNS in the study of Tang et al., 12% had surgical complications [15]. The surgical complication rate in this larger cohort was 13.3% and, therefore, within the range of the mentioned studies and lower compared to DHS group, despite that the mean age was considerably higher in our study. All mentioned studies reported cases with avascular necrosis, which did not occur in any patients of this study. This might be explained with the low time to surgery of 13.5 h. Compared to DHS the FNS group had a lower surgical complication rate. While cut out was slightly more often (FNS 12.4% vs. DHS 10.2%), there were considerably less cases with hematoma and no case of implant related infection in FNS group. With careful surgical planning, the FNS can be implanted through a 3–4 cm incision and is, therefore, more minimal invasive than DHS [16]. The incision size in the study of Tang et al. was 4 cm in FNS group and comparable to the incision of the CCS group. There was no significant difference between the groups with regard to cut outs, underlining the biomechanical comparisons that showed equal stability for both implants. The main influence to prevent mechanical failure is still the surgeon. Less than 50% of the patients with cut out of the FNS or DHS-blade had an optimal blade position. The relative risk for cut out significantly increased sevenfold for none optimal blade positioning. Despite that, multiple studies already showed an increased rate of cut out with blade position deviating from center–center and inferior–center [17,18,19,20] there were still around 88% of the patient had optimal blade positions in this study. This highlights the importance of the correct surgical technique regardless of the implant. The tip apex distance was no significant predictor of implant failure in this study. In both groups mean tip apex distance was less than 25 mm, what might have prevented further cut outs compared to the results of studies including more cases with tip apex distance higher than 25 mm [19, 20]. Tip apex distance was slightly less in FNS group. The authors used the described technique from Cha et al. to ensure low tip apex distance in all cases [21]. Cut outs in the FNS group occurred significantly more often in Pauwels III fractures. This might be explained with the usage of only 1-hole plates for the FNS. Yan et al. showed a lower biomechanical stability of the FNS when the fracture angle exceed 70° and only a 1-hole plate is used [14]. Therefore, the author suggests using 2-hole plates in Pauwels III fractures to prevent implant failure at the side of the plate (Fig. 1B). In both groups, patients between 20 and 98 years of age with Garden III/IV as well as Pauwels III fractures were included. Neither fracture classifications nor age showed a statistically significant influence on surgical complications and implant failure. While current guidelines recommend osteosynthesis only in undisplaced fractures in patients over 60 years [4] the authors also used it in Garden III and IV fractures. Overall 52 patients older than 60 years were treated with FNS or DHS for Garden III and IV fractures if the overall condition of the patients does not allow arthroplasty. Out of the geriatric cohort only eight patients showed mechanical failure. This highlights that both implants can be used even in older patients as an alternative to endoprosthesis for patients in poor overall condition. There is evidence that patients with severe comorbidities might profit from osteosynthesis compared to arthroplasty [22]. If mechanical failure was detected in X-ray controls and the patient presented with pain and impaired functionality of the hip revision surgery was performed in the majority of the cases with arthroplasty. Only two young patients were treated with reosteosynthesis.
Hip fractures treated with osteosynthesis have a risk of femoral neck shortening which can result in a difference of leg length. The FAITH trial showed comparable femoral neck shortening of DHS compared to CCS [8]. Femoral neck shortening was significantly less in the FNS group compared to the CCS group in the study of Tang et al. Compared to both studies the rate of femoral neck compression over 5 mm of the FNS in our study was comparable. Still, the DHS showed no difference in mean shortening or rate of shortening over 5 mm compared to the FNS in this study. Furthermore, Haider et al. showed that femoral neck shortening did not impair functional outcome in the majority of cases [23]. The FNS could be implanted with shorter operating time and less Hb-difference and the patients could be released home or into rehabilitation significantly earlier. Compared to the study of Yan et al. and Tang et al. the FNS was implanted 22 min and 16 min faster in our study, which might be explained by a higher case load of approximately 40 cases a year at our institution.
In summary, the "new" FNS is slightly better regarding operating time, Hb-difference and duration of hospital stay and can be used for all ages and fracture patterns. However, the most important factor is not the implant, but the correct surgical technique to prevent surgical complications.
Conclusion
The FNS is a new strong treatment option for femoral neck fractures for patients of all ages. Compared to DHS it can be implanted faster and with less blood loss. Surgical complication rates are comparable, especially rate of cut out. However, most important is not a modern implant but a surgical technique respecting optimal blade positioning and tip apex distance less than 25 mm.
References
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413. https://doi.org/10.1007/pl00004148
Rupp M, Walter N, Pfeifer C et al (2021) The incidence of fractures among the adult population of Germany. Dtsch Arztebl Int 118:665–669. https://doi.org/10.3238/arztebl.m2021.0238
Parker M, Johansen A (2006) Hip fracture. BMJ 333:27–30. https://doi.org/10.1136/bmj.333.7557.27
Bhandari M, Swiontkowski M (2017) Management of acute hip fracture. N Engl J Med 377:2053–2062. https://doi.org/10.1056/NEJMcp1611090
Bhandari M, Devereaux PJ, Swiontkowski MF et al (2003) Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Jt Surg Am 85:1673–1681. https://doi.org/10.2106/00004623-200309000-00004
Deng J, Wang G, Li J et al (2021) A systematic review and meta-analysis comparing arthroplasty and internal fixation in the treatment of elderly displaced femoral neck fractures. OTA Int 4:e087. https://doi.org/10.1097/OI9.0000000000000087
Hu F, Jiang C, Shen J et al (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 43:676–685. https://doi.org/10.1016/j.injury.2011.05.017
Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH) Investigators (2017) Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. Lancet 389:1519–1527. https://doi.org/10.1016/S0140-6736(17)30066-1
Stoffel K, Zderic I, Gras F et al (2017) Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma 31:131–137. https://doi.org/10.1097/BOT.0000000000000739
Schopper C, Zderic I, Menze J et al (2020) Higher stability and more predictive fixation with the femoral neck system versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Transl 24:88–95. https://doi.org/10.1016/j.jot.2020.06.002
Jung C-H, Cha Y, Yoon HS et al (2022) Mechanical effects of surgical variations in the femoral neck system on Pauwels type III femoral neck fracture: a finite element analysis. Bone Jt Res 11:102–111. https://doi.org/10.1302/2046-3758.112.BJR-2021-0282.R1
Fan Z, Huang Y, Su H, Jiang T (2021) How to choose the suitable FNS specification in young patients with femoral neck fracture: a finite element analysis. Injury 52:2116–2125. https://doi.org/10.1016/j.injury.2021.05.043
Stassen RC, Jeuken RM, Boonen B et al (2021) First clinical results of 1-year follow-up of the femoral neck system for internal fixation of femoral neck fractures. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04216-0
Yan C, Wang X, Xiang C et al (2021) Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 35:1286–1292. https://doi.org/10.7507/1002-1892.202103099
Tang Y, Zhang Z, Wang L et al (2021) Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res 16:504–508. https://doi.org/10.1186/s13018-021-02659-0
Hou W-R, Xu M-O (2015) Comparison among three cannulated screws and dynamic hip screw combined with antirotation screw for comminut-ed fractures of femoral neck. Zhongguo Gu Shang 28:796–801
Pervez H, Parker MJ, Vowler S (2004) Prediction of fixation failure after sliding hip screw fixation. Injury 35:994–998. https://doi.org/10.1016/j.injury.2003.10.028
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Jt Surg Am 77:1058–1064. https://doi.org/10.2106/00004623-199507000-00012
Page PRJ, Field MH, Vetharajan N et al (2020) Incidence and predictive factors of problems after fixation of trochanteric hip fractures with sliding hip screw or intramedullary devices. Hip Int 32:1120700020959339. https://doi.org/10.1177/1120700020959339
Caruso G, Corradi N, Caldaria A et al (2022) New tip-apex distance and calcar-referenced tip-apex distance cut-offs may be the best predictors for cut-out risk after intramedullary fixation of proximal femur fractures. Sci Rep 12:357–410. https://doi.org/10.1038/s41598-021-04252-1
Cha Y, Song J-U, Yoo J-I et al (2021) Improved control over implant anchorage under the use of the femoral neck system for fixation of femoral neck fractures: a technical note. BMC Musculoskelet Disord 22:621–628. https://doi.org/10.1186/s12891-021-04497-x
Cintean R, Pankratz C, Hofmann M et al (2021) Early results in non-displaced femoral neck fractures using the femoral neck system. Geriatr Orthop Surg Rehabil 12:21514593211050150. https://doi.org/10.1177/21514593211050153
Haider T, Schnabel J, Hochpöchler J, Wozasek GE (2018) Femoral shortening does not impair functional outcome after internal fixation of femoral neck fractures in non-geriatric patients. Arch Orthop Trauma Surg 138:1511–1517. https://doi.org/10.1007/s00402-018-3011-0
Funding
Open Access funding enabled and organized by Projekt DEAL. No author is affiliated to any of the supporting companies or received or will receive any form of payment related to this study. The authors did not receive support from any organization for the submitted work. No funding was received to assist with the preparation of this manuscript. No funding was received for conducting this study. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
We affirm that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere. All authors have contributed equally.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest. No company had influence in the collection of data or contributed to or had influence on the conception, design, analysis and writing of the study. No further funding was received. The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible ethics committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University Ulm.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schuetze, K., Burkhardt, J., Pankratz, C. et al. Is new always better: comparison of the femoral neck system and the dynamic hip screw in the treatment of femoral neck fractures. Arch Orthop Trauma Surg 143, 3155–3161 (2023). https://doi.org/10.1007/s00402-022-04551-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04551-w