Abstract
Introduction
Postoperative infection is one of the most common postoperative complications in hip fracture surgery. It is related with increased morbidity and mortality. This study aimed at developing a nomogram to predict the individual probability of postoperative infection to facilitate perioperative decision-making.
Materials and Methods
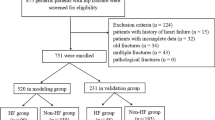
In this retrospective study, we included all patients over 65 years old admitted for hip fracture in West China Hospital of Sichuan University from 1 January 2015 to 31 December 2019. Univariate and multivariate logistic regression analyses were used to identify significant predictors. We used all-subsets regression to screen an optimal model, and visualized the model through drawing nomogram. To evaluate the model performance, we applied receiver operating characteristic curve and calibration curve.
Results
We enrolled 677 older patients. 136 (20.1%) patients developed postoperative infection during hospitalization. Variables retained in the final model were albumin [odds ratio (OR) 0.90, 95% confidence interval (CI) 0.84–0.96], cholesterol (OR 1.49, 95% CI 1.04–2.15), blood phosphorus (OR 0.16, 95% CI 0.05–0.48), high-density lipoprotein (OR 0.42, 95% CI 0.19–0.89), surgery type (OR 2.27, 95% CI 1.35–3.90), smoking (OR 1.95, 95% CI 1.02–3.66), American Society of Anesthesiologists classification [class III (OR 1.02, 95% CI 0.55–1.93); class IV (OR 1.93, 95% CI 0.76–4.82)], and chronic pulmonary disease (OR 2.16, 95% CI 1.25–3.68). The C-index of the nomogram was 0.752 (95% CI 0.697–0.806). Calibration curve showed good agreement between predicted value and observed outcome. In the validation group, our nomogram showed an area under the receiver operating characteristic curve of 0.723 (95% CI 0.639–0.807).
Conclusion
Our nomogram showed good discrimination ability in predicting individual probability of postoperative infection among older patients with hip fracture surgery. The nomogram could help clinicians identify patients at high risk of postoperative infection before surgery.






Similar content being viewed by others
References
Ma T, Lu K, Song L et al (2019) Modifiable factors as current smoking, hypoalbumin, and elevated fasting blood glucose level increased the SSI risk following elderly hip fracture surgery. J Invest Surg. https://doi.org/10.1080/08941939.2018.1556364
Norouzi A, Behrouzibakhsh F, Kamali A et al (2018) Short-term complications of anesthetic technique used in hip fracture surgery in elderly people. Eur J Transl Myol 28(3):280–287. https://doi.org/10.4081/ejtm.2018.7355
Liu X, Dong Z, Li J et al (2019) Factors affecting the incidence of surgical site infection after geriatric hip fracture surgery: a retrospective multicenter study. J Orthop Surg Res 14(1):382. https://doi.org/10.1186/s13018-019-1449-6
Kristensen PK, Rock ND, Christensen HC et al (2020) The danish multidisciplinary hip fracture registry 13-year results from a population-based cohort of hip fracture patients. Clin Epidemiol 12:9–21. https://doi.org/10.2147/CLEP.S231578
Katsoulis M, Benetou V, Karapetyan T et al (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med 281(3):300–310. https://doi.org/10.1111/joim.12586
Kjorholt KE, Kristensen NR, Prieto-Alhambra D et al (2019) Increased risk of mortality after postoperative infection in hip fracture patients. Bone 127:563–570. https://doi.org/10.1016/j.bone.2019.07.023
Xiao H, Zhou H, Liu K et al (2019) Development and validation of a prognostic nomogram for predicting post-operative pulmonary infection in gastric cancer patients following radical gastrectomy. Sci Rep 9(1):14587. https://doi.org/10.1038/s41598-019-51227-4
Gallo O, Locatello LG, Larotonda G et al (2018) Nomograms for prediction of postoperative complications in open partial laryngeal surgery. J Surg Oncol 118(6):1050–1057. https://doi.org/10.1002/jso.25232
de Jong L, Klem TMAL, Kuijper TM et al (2017) Factors affecting the rate of surgical site infection in patients after hemiarthroplasty of the hip following a fracture of the neck of the femur. Bone Jt J 99-B:1088–1094. https://doi.org/10.1302/0301-620X.99B8
Colman M, Wright A, Gruen G et al (2013) Prolonged operative time increases infection rate in tibial plateau fractures. Injury 44(2):249–252. https://doi.org/10.1016/j.injury.2012.10.032
Liu D, Zhu Y, Chen W et al (2020) Multiple preoperative biomarkers are associated with incidence of surgical site infection following surgeries of ankle fractures. Int Wound J 17(3):842–850. https://doi.org/10.1111/iwj.13351
Cross MB, Yi PH, Thomas CF et al (2014) Evaluation of malnutrition in orthopaedic surgery. J Am Acad Orthop Surg 22(3):193–199. https://doi.org/10.5435/JAAOS-22-03-193
Ren MG, Liang WD, Wu ZY et al (2019) Risk factors of surgical site infection in geriatric orthopedic surgery: a retrospective multicenter cohort study. Geriatr Gerontol Int 19(3):213–217. https://doi.org/10.1111/ggi.13590
Folbert EC, Hegeman JH, Gierveld R et al (2017) Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg 137(4):507–515. https://doi.org/10.1007/s00402-017-2646-6
Vochteloo AJ, Borger van der Burg BL, Roling MA et al (2012) Contralateral hip fractures and other osteoporosis-related fractures in hip fracture patients: incidence and risk factors. An observational cohort study of 1229 patients. Arch Orthop Trauma Surg 132(8):1191–1197. https://doi.org/10.1007/s00402-012-1520-9
Kastanis G, Topalidou A, Alpantaki K et al (2016) Is the ASA score in geriatric hip fractures a predictive factor for complications and readmission? Scientifica 2016:1–6. https://doi.org/10.1155/2016/7096245
Garcia AE, Bonnaig JV, Yoneda ZT et al (2012) Patient variables which may predict length of stay and hospital costs in elderly patients with hip fracture. J Orthop Trauma 26(11):620–623. https://doi.org/10.1097/BOT.0b013e3182695416
Li Y, Tan BB, Fan LQ et al (2016) Clinicopathologic characteristics of elderly with gastric cancer, and the risk factors of postoperative complications. J Invest Surg. https://doi.org/10.1080/08941939.2016.1265617
Qaseem A, Snow V, Fitterman N et al (2006) Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: a guideline from the American college of physicians. Ann Intern Med 144:575–580. https://doi.org/10.7326/0003-4819-144-8-200604180-00008
Nie B, Wu D, Yang Z et al (2017) Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: a meta-analysis. Medicine 96(27):e7446. https://doi.org/10.1097/MD.0000000000007446
Ye CY, Liu A, Xu MY et al (2016) Arthroplasty versus internal fixation for displaced intracapsular femoral neck fracture in the elderly: systematic review and meta-analysis of short- and long-term effectiveness. Chin Med J (Engl) 129(21):2630–2638. https://doi.org/10.4103/0366-6999.192788
Xiao P, Song W, Han Z (2018) Characteristics of pulmonary infection after mitral valve repair in patients with metabolic syndrome and its relationship with blood pressure, blood glucose and blood lipid. Exp Ther Med 16(6):5003–5008. https://doi.org/10.3892/etm.2018.6839
Murphy AJ, Chin-Dusting JPF, Sviridov D et al (2009) The anti inflammatory effects of high density lipoproteins. Curr Med Chem 16:667–675. https://doi.org/10.2174/092986709787458425
Lee SH, Lee JY, Hong TH et al (2018) Severe persistent hypocholesterolemia after emergency gastrointestinal surgery predicts in-hospital mortality in critically ill patients with diffuse peritonitis. PLoS ONE 13(7):e0200187. https://doi.org/10.1371/journal.pone.0200187
Tekkesin AI, Hayiroglu MI, Zehir R et al (2017) The use of monocyte to HDL ratio to predict postoperative atrial fibrillation after aortocoronary bypass graft surgery. North Clin Istanb 4(2):145–150. https://doi.org/10.14744/nci.2017.53315
Lin CA, Behrens PH, Paiement G et al (2020) Metabolic factors and post-traumatic arthritis may influence the increased rate of surgical site infection in patients with human immunodeficiency virus following total hip arthroplasty. J Orthop Surg Res 15(1):316. https://doi.org/10.1186/s13018-020-01827-y
Miguel DR, Marcelino MC, Gabriel MG et al (1997) Total cholesterol, HDL-cholesterol, and risk of nosocomial infection: a prospective study in surgical patients. Infect Control Hosp Epidemiol 18(1):9–18. https://doi.org/10.1086/647494
Canturk NZ, Canturk Z, Okay E et al (2002) Risk of nosocomial infections and effects of total cholesterol, HDL cholesterol in surgical patients. Clin Nutr 21(5):431–436. https://doi.org/10.1054/clnu.2002.0575
Giovannini I, Chiarla C, Nuzzo G (2002) Pathophysiologic and clinical correlates of hypophosphatemia and the relationship with sepsis and outcome in postoperative patients after hepatectomy. Shock 18(2):111–115. https://doi.org/10.1097/00024382-200208000-00003
Kabacoff RI (2015) R in action-Data analysis and graphics with R. Selecting the “best” regression model. Manning Publications, Shelter Island, pp 209–212
Kabacoff RI (2015) R in action-data analysis and graphics with R. Multiple imputation. Manning Publications, Shelter Island, pp 365–369
Jaafar G, Hammarqvist F, Enochsson L et al (2017) Patient-related risk factors for postoperative infection after cholecystectomy. World J Surg 41(9):2240–2244. https://doi.org/10.1007/s00268-017-4029-0
Funding
This work was supported by National Key R&D Program of China (grant number 2018YFC2001800) to XCH and TZ; National Clinical Research Center for Geriatrics, West China Hospital of Sichuan University (grant number Z2018A02) to TZ; and 1·3·5 project for disciplines of excellence, West China Hospital, Sichuan University to TZ.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data acquisition, data analysis and model construction were performed by XP and XH. The initial draft of the manuscript was written by XP. Critical revision of manuscript was performed by XH and TZ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
The protocol of this study was approved by Committee of Ethics from West China Hospital of Sichuan University (2019-473) with waiver of informed consent, and registered at www.chictr.org.cn (ChiCTR1900025160).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
402_2021_4171_MOESM1_ESM.pdf
Supplementary file1 Supplementary table S1 Variables included in study. Supplementary table S1 Univariate logistic regression analysis of predictors for postoperative infection Supplementary table S3 VIF value of each variable. Supplementary table S4 VIF value of each variable after adjustment for strongly correlated variables (PDF 443 kb)
Rights and permissions
About this article
Cite this article
Peng, X., Hao, X. & Zhu, T. A nomogram to predict postoperative infection for older hip fracture patients. Arch Orthop Trauma Surg 143, 847–855 (2023). https://doi.org/10.1007/s00402-021-04171-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04171-w