Abstract
Introduction
The purpose of this study is to investigate whether the specific socioeconomic factor such as marital status has any effect on clinical outcomes and patient-reported outcome measures (PROMs) after primary total hip (THA) and knee (TKA) arthroplasty.
Materials and methods
We retrospectively reviewed patients who underwent primary THA or TKA from January 2019 to August 2019 who answered all PROM questionnaires. Both THA and TKA patients were separated into two groups based on their marital status at the time of surgery (married vs. non-married). Demographics, clinical data, and PROMs (FJS-12, HOOS, JR, KOOS, JR, and VR-12 PCS&MCS) were collected at various time-periods. Demographic differences were assessed using chi-square and independent sample t tests. Clinical data and mean PROMs were compared using multilinear regressions while accounting for demographic differences.
Results
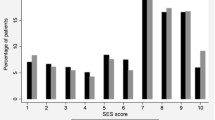
This study included 389 patients who underwent primary THA and 193 that underwent primary TKA. In the THA cohort, 256 (66%) patients were married and 133 (34%) were non-married. In the TKA cohort, there were 117 (61%) married patients and 76 (39%) non-married patients. Length of stay was significantly shorter for married patients in both the THA (1.30 vs. 1.64; p = 0.002) and TKA (1.89 vs. 2.36; p = 0.024) cohorts. Surgical-time, all-cause emergency department visits, discharge disposition, and 90-day all-cause adverse events (readmissions/revisions) did not statistically differ between both cohorts. Both HOOS, JR and KOOS, JR score improvements from baseline to 1-year did not statistically differ for the THA and TKA cohorts, respectively. Although VR-12 PCS (p = 0.012) and MCS (p = 0.004) score improvement from baseline to 1-year statistically differed for the THA cohort, they did not for the TKA cohort.
Conclusion
Total joint arthroplasty may yield similar clinical benefits in all patients irrespective of their marital status. Although some PROMs statistically differed among married and non-married patients, the differences are likely not clinically significant. Surgeons should continue to assess levels of psychosocial support in their patients prior to undergoing TJA to optimize outcomes.
Level of evidence
III, Retrospective Cohort Study.
Similar content being viewed by others
References
Wolford ML, Palso K, Bercovitz A (2015) Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000-2010. NCHS Data Brief (186):1–8
Steinhaus ME, Christ AB, Cross MB (2017) Total knee arthroplasty for knee osteoarthritis: support for a foregone conclusion? HSS J 13:207–210
Almeida GJ, Khoja SS, Piva SR (2018) Physical activity after total joint arthroplasty: a narrative review. Open access. J Sport Med 9:55–68. https://doi.org/10.2147/oajsm.s124439
Brembo EA, Kapstad H, Van Dulmen S, Eide H (2017) Role of self-efficacy and social support in short-term recovery after total hip replacement: a prospective cohort study. Health Qual Life Outcomes. https://doi.org/10.1186/s12955-017-0649-1
Wu KT, Lee PS, Chou WY et al (2018) Relationship between the social support and self-efficacy for function ability in patients undergoing primary hip replacement. J Orthop Surg Res. https://doi.org/10.1186/s13018-018-0857-3
Kugelman DN, Haglin JM, Carlock KD et al (2019) The association between patient education level and economic status on outcomes following surgical management of (fracture) non-union. Injury 50:344–350. https://doi.org/10.1016/j.injury.2018.12.013
Inacio MCS, Paxton EW, Graves SE et al (2017) Projected increase in total knee arthroplasty in the United States—an alternative projection model. Osteoarthr Cartil 25:1797–1803. https://doi.org/10.1016/j.joca.2017.07.022
Bonasia DE, Palazzolo A, Cottino U et al (2019) Modifiable and nonmodifiable predictive factors associated with the outcomes of total knee arthroplasty. Joints 7:13–18. https://doi.org/10.1055/s-0039-1678563
Rosenberger PH, Jokl P, Ickovics J (2006) Psychosocial factors and surgical outcomes: an evidence-based literature review. J Am Acad Orthop Surg 14:397–405. https://doi.org/10.5435/00124635-200607000-00002
Theiss MM, Ellison MW, Tea CG et al (2011) The connection between strong social support and joint replacement outcomes. Orthopedics. https://doi.org/10.3928/01477447-20110317-02
Lindner M, Nosseir O, Keller-Pliessnig A et al (2018) Psychosocial predictors for outcome after total joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord 19:159. https://doi.org/10.1186/s12891-018-2058-y
Lall AC, Schwarzman GR, Battaglia MR et al (2019) Effect of marital status on patient-reported outcomes following total hip arthroplasty: a matched analysis with minimum 2-year follow-up. HIP Int. https://doi.org/10.1177/1120700019864015
Holtz N, Hamilton DF, Giesinger JM et al (2020) Minimal important differences for the WOMAC osteoarthritis index and the Forgotten Joint Score-12 in total knee arthroplasty patients. BMC Musculoskelet Disord 21:401. https://doi.org/10.1186/s12891-020-03415-x
Lyman S, Lee YY, McLawhorn AS et al (2018) What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after total joint replacement? Clin Orthop Relat Res 476:2432–2441. https://doi.org/10.1097/CORR.0000000000000456
Kazis LE, Miller DR, Skinner KM et al (2004) Patient-reported measures of health: the veterans health study. J Ambul Care Manag 27:70–83. https://doi.org/10.1097/00004479-200401000-00012
Sorel JC, Veltman ES, Honig A, Poolman RW (2019) The influence of preoperative psychological distress on pain and function after total knee arthroplasty a systematic review and meta-analysis. Bone Jt J 101B:7–14. https://doi.org/10.1302/0301-620X.101B1.BJJ-2018-0672.R1
Lavernia CJ, Villa JM, Iacobelli DA (2015) what is the role of mental health in primary total knee arthroplasty? Clin Orthop Relat Res 473:159–163. https://doi.org/10.1007/s11999-014-3769-5
Khatib Y, Madan A, Naylor JM, Harris IA (2015) Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clin Orthop Relat Res 473:2630–2638. https://doi.org/10.1007/s11999-015-4234-9
Ali A, Lindstrand A, Sundberg M, Flivik G (2017) Preoperative Anxiety and depression correlate with dissatisfaction after total knee arthroplasty: a prospective longitudinal cohort study of 186 patients, with 4-year follow-up. J Arthroplasty 32:767–770. https://doi.org/10.1016/j.arth.2016.08.033
Lopez-Olivo MA, Landon GC, Siff SJ et al (2011) Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis 70:1775–1781. https://doi.org/10.1136/ard.2010.146423
Horn EE, Xu Y, Beam CR et al (2013) Accounting for the physical and mental health benefits of entry into marriage: a genetically informed study of selection and causation. J Fam Psychol 27:30–41. https://doi.org/10.1037/a0029803
Carr D, Springer KW (2010) Advances in families and health research in the 21st century. J Marriage Fam 72:743–761. https://doi.org/10.1111/j.1741-3737.2010.00728.x
Robards J, Evandrou M, Falkingham J, Vlachantoni A (2012) Marital status, health and mortality. Maturitas 73:295–299. https://doi.org/10.1016/j.maturitas.2012.08.007
Ihekweazu UN, Sohn GH, Laughlin MS et al (2018) Socio-demographic factors impact time to discharge following total knee arthroplasty. World J Orthop 9:285–291. https://doi.org/10.5312/wjo.v9.i12.285
Farley KX, Anastasio AT, Premkumar A et al (2019) The Influence of modifiable, postoperative patient variables on the length of stay after total hip arthroplasty. J Arthroplasty 34:901–906. https://doi.org/10.1016/j.arth.2018.12.041
Marsh J, Somerville L, Howard JL, Lanting BA (2019) Significant cost savings and similar patient outcomes associated with early discharge following total knee arthroplasty. Can J Surg 62:20–24. https://doi.org/10.1503/cjs.002118
Garbarino LJ, Gold PA, Sodhi N et al (2019) The effect of operative time on in-hospital length of stay in revision total knee arthroplasty. Ann Transl Med 7:66–66. https://doi.org/10.21037/atm.2019.01.54
Varacallo M, Luo TD, Johanson NA (2020) Total Knee Arthroplasty Techniques. In: StatPearls, 31 Jul 2020. StatPearls Publishing, Treasure Island
Choi Y-J, Ra HJ (2016) Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res 28:1–15. https://doi.org/10.5792/ksrr.2016.28.1.1
Funding
There was no funding provided for this study. The records and existing data were de-identified and a part of our institutional quality improvement program; therefore, the present study was exempt from human-subjects review by our Institutional Review Board (IRB). Informed consent was obtained from all individual participants included in the study as part of our standard operative consent. The authors have not received grant support or research funding for this project and do not have any proprietary interests in the materials described in the article. Individual potential conflict of interests are as follows. V.S: none. B.F: none. D.N.K: none. V.K.A: none. M.M reports receiving royalties from Innomed, is a paid consultant for Intellijoint, and has stock options in CAIRA surgical outside the submitted work. RS: paid consultant for Smith & Nephew and Intellijoint, has stock options in Gauss Surgical and PSI outside the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest pertinent to this study.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, V., Fiedler, B., Kugelman, D.N. et al. Effect of Marital Status on Outcomes Following Total Joint Arthroplasty. Arch Orthop Trauma Surg 142, 3651–3658 (2022). https://doi.org/10.1007/s00402-021-03914-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03914-z