Abstract
Purpose
Total hip arthroplasty (THA) is a successful procedure. However, in time, heterotopic ossification (HO) can form due to, amongst others, soft tissue damage. This can lead to pain and impairment. This study compares the formations of HO between patients who underwent either THA with the posterolateral approach (PA) or with the direct lateral approach (DLA). Our hypothesis is that patients who underwent THA with a PA form less HO compared to THA patients who underwent DLA.
Methods
In this prospective cohort study, 296 consecutive patients were included who underwent THA. A total of 127 patients underwent THA with the PA and 169 with the DLA. This was dependent on the surgeon’s preference and experience. More than 95% of patients had primary osteoarthritis as the primary diagnosis. Clinical outcomes were scored using the Numeric Rating Scale (NRS) and Harris Hip Score (HHS), radiological HO were scored using the Brooker classification. Follow-up was performed at 1 and 6 years postoperatively.
Results
Two hundred and fifty-eight patients (87%) completed the 6-year follow-up. HO formation occurred more in patients who underwent DLA, compared to PA (43(30%) vs. 21(18%), p = 0.024) after 6 years. However, the presence of severe HO (Brooker 3–4) was equal between the DLA and PA (7 vs. 5, p = 0.551). After 6 years the HHS and NRS for patient satisfaction were statistically significant higher after the PA (95.2 and 8.9, respectively) compared to the DLA (91.6 and 8.5, respectively) (p < 0.001 and p = 0.003, respectively). The NRS for load pain was statistically significant lower in the PA group (0.5) compared to the DLA group (1.2) (p = 0.004). The NRS for rest pain was equal: 0.3 in the PA group and 0.5 in the DLA group.
Conclusion
THA with the PA causes less HO formation than the DLA.
Trial registration
Registrated as HipVit trial, NL 32832.100.10, R-10.17D/HIPVIT 1. Central Commission Human-Related research (CCMO) Registry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is a successful treatment for patients with hip osteoarthritis, resulting in less pain, a greater range of motion (ROM) and a considerably higher quality of life [1, 2]. However, in a minority of patients, peri-articular heterotopic ossifications (HO) develop postoperatively. These bony formations in the soft tissues of the operated hip can lead to pain and impairment of ROM [3, 4]. Especially severe HO can lead to significant disability [5].
Soft tissue damage caused by the surgery provides an environment that causes osteoblasts to arrive from mesenchymal cells, resulting in HO [3, 4]. Therefore, it is thought that increased soft tissue damage during surgery result in more HO [6]. Known risk factors for the formation of HO include male sex, smoking, a chronic infection, high number of operations, hypertrophic osteoarthritis, previous development of HO, posttraumatic arthritis, ankylosing spondylitis, diffuse hyperostosis, Paget’s disease, paraplegia or traumatic brain injury [7,8,9,10,11].
However, there is no consensus about the influence of different surgical approaches in THA on the formation of HO. A more extensive approach may cause more tissue damage which increases formation of HO [6, 12,13,14]. These studies compare anterior, anterolateral and direct lateral approaches. No information is available about HO formation after a direct lateral approach (DLA) compared to a posterolateral approach (PA) yet.
The aim of this study is to compare the presence and severity of HO after 1 and 6 years after THA between the DLA and the PA for THA.
Materials and methods
Study design
This prospective cohort study was performed at the Diakonessenhuis Hospital, a medium size general hospital in Utrecht/Zeist, the Netherlands. Ethical local institutional review board approval was obtained. Informed consent was acquired from all participating patients. Between 2009 and 2015, a total of 296 consecutive patients were included. All included patients are derived from two existing prospective THA cohorts of our hospital [15, 16]. All patients scheduled for primary THA between 20 and 85 years old with either primary osteoarthritis or secondary osteoarthritis due to congenital hip dysplasia, rheumatoid arthritis, avascular necrosis of the femoral head or trauma and who were willing to participate in this study were eligible. Patients with an ASA score > III were excluded, because both cohorts were established to describe long-term follow-up after THA. Baseline characteristics are shown in Table 1. More than 95% of patients had primary osteoarthritis as the primary diagnosis. The other patients were included after a fracture, because of secondary osteoarthritis, hip dysplasia or avascular necrosis of the femoral head. None of the included patients had one of the following risk factors for developing HO: diffuse osteopathic skeletal hyperostosis, Paget’s disease or paraplegia. We did not collect data on hypertrophic osteoarthritis or previous development of HO or hypertrophic.
Patients were scheduled for clinical and radiological follow-up after 1 and 6 years. At each follow-up HHS, NRS score for rest and load pain and patient satisfaction were documented, and antero-posterior radiographs of the pelvis in supine position were made. Follow-up was performed by two investigators (JHJE and TES). The primary outcome of this study is the prevalence of HO after 6 years. Secondary outcomes are the presence of HO after 1 year and clinical outcomes at both moments.
Procedure
Critical aspects of the surgical procedure were standardized. The procedures were performed by seven orthopedic surgeons, each with vast experience in uncemented THA. The surgical approach used was dependent on the surgeon’s preference and experience. Alumina ceramic femoral prosthetic heads (BIONIT2, Mathys Ltd, Bettlach, Switzerland) of 28, 32 or 36 mm were used. An uncemented hydroxyapatite coated stem (Twinsys, Mathys Ltd, Bettlach, Switzerland) was implanted in all cases. All patients received an uncemented vitamin E blended HXLPE cup (RM uncemented monoblock pressfit Vitamys® cup, Mathys Ltd, Bettlach, Switzerland) or a UHMWPE cup (RM uncemented monoblock pressfit®, Mathys Ltd, Bettlach, Switzerland) [15, 17]. No pulse lavage was used.
Key aspects of pre- and postoperative care were protocolled to ensure similar perioperative regimens. All patients received cefazolin prophylaxis during 24-h perioperatively and thromboprophylaxis with low molecular weight heparin for 6 weeks postoperative. All patients followed the same rehabilitation regimen, starting on the first day after surgery, with diclofenac, a non-steroidal anti-inflammatory drug (NSAID), except when use was medically contraindicated. For the NSAID use, patients received a 14-day prescription for home use of 50 mg 3 times a day. We did not follow-up the therapy compliance of the patients. No radiotherapy was used to prevent HO.
Radiological assessment
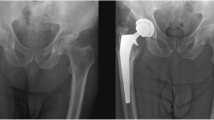
The Brooker classification was used for grading of HO, which has proven to be the most accurate scoring system for HO [18]. Figure 1 shows an example of a patient with Brooker grade 4 HO. Radiological assessment was performed twice by two authors independently (JRAM and ST). The authors were blinded for the approach. Brooker grade 1–2 was considered as radiological mild HO and Brooker grade 3–4 was considered as radiological severe HO.
Statistical analysis
Statistical analysis was performed using SPSS Statistics, version 23.0 (IBM Corp., Armonk, NY, USA). Normal distribution of the data was analyzed using the Kolmogorov–Smirnov test. Patients’ characteristics were compared using an independent t test and a Chi-square test. The prevalence of HO was compared using a Chi-square test. Clinical outcomes were compared using an independent t test.
Ethical standards
The procedures performed in this study, involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
A total of 258 patients (87%) completed the 6-year follow-up (Fig. 2). Data were normally distributed. A total of 38 patients (13%) were lost to follow-up because of revision, other diseases, unable to attend or death. There were no revisions performed because of HO.
Heterotopic ossifications
After 1 year, HO was found in 18 (14%) patients of the PA group and in 30 (19%) patients of the DLA group (p = 0.207) (Table 2). After 6 years, HO was found in 21 (18%) patients of the PA group and 43 (30%) patients of the DLA group (p = 0.024).
When considering Brooker (3–4) as radiological severe, in both groups three patients (2%) had HO after 1 year (p = 0.537) (Table 2). After 6 years, this was 5 (4%) patients in the PA group and 7 (5%) in the DLA group (p = 0.551).
Clinical outcomes
NRS score and Harris Hip Scores (HHS) at 1- and 6-year follow-up are presented in Fig. 3. Scores for both groups at 6-year follow-up are specified in Table 3. After 6 years, the HHS was statistically significant higher after the PA (95.2) compared to the DLA (91.6) (p < 0.001). Furthermore, NRS score for patient satisfaction was significantly higher in the PA group (8.9) compared to the DLA group (8.5) (p = 0.003). The NRS score for rest pain was equal: 0.3 in the PA group and 0.5 in the DLA group. The NRS score for load pain was statistically significant lower in the PA group (0.5) compared to the DLA group (1.2) (p = 0.004) (Table 3).
After 6 years, in patients with severe HO (Brooker 3–4), the mean HHS was 96.4(± 6) for the PA and 88.5(± 6) for the DLA. The mean NRS for patient satisfaction was 8.8(± 1) for the PA and 8.5(± 1) for the DLA. The NRS for rest pain was 0.0 in both groups. The NRS for load pain was 0.0(± 0) in the PA and 1.5(± 2) for the DLA. For one patient, who underwent the DLA, clinical data were missing (Table 4).
Discussion
This prospective cohort study was conducted to compare HO formations between patients who underwent THA either with a PA or DLA. After 6 years of follow-up, statistically significant more radiological HO formation was found after the DLA compared to the PA (30% vs. 18%). However, no difference in radiological severe HO (Brooker 3–4) was found between groups at 6-year follow-up.
The finding that patients undergoing DLA for THA form more HO can be explained by the fact that DLA presumably causes more tissue damage (because this approach requires dissection of gluteal musculature from the trochanter major with specific placement of retractors necessary to perform DLA) [19]. More tissue damage causes more inflammation, and subsequently more HO formation [20, 21].
Some studies have been conducted about the influence of approach of THA on HO formation [6, 12, 14]. However, only one discussed HO formation after PA. This study did not find differences in HO formation (Brooker 1–4) between the anterolateral approach and the PA [13]. However, similar to our study, the lowest incidence of both HO formation (Brooker 1–4) and severe HO formation (Brooker 3–4) was found after PA. Furthermore, nowadays, the direct anterior approach (DAA) is performed in increasing numbers. Alijanipour et al. compared DAA with DLA and found a statistically significant more HO formation in DLA [6]. However, no statistically significant difference was found in the severe HO formation between DAA and DLA. Zran et al. found a lower incidence of HO in patients undergoing a PA (27.6%) compared to patients undergoing DLA without orthopedic table (47.7%) (p < 0.01) [22]. They, as well, did not find significant differences regarding the severity of HO.
At the 6-year follow-up, we found significantly better HHS and NRS scores for patient satisfaction and load pain for patients who underwent PA compared to DLA. In our opinion, these results cannot be attributed to less HO formation in the PA group compared to DLA because more factors related to the surgical approach may influence outcome of THA [23]. Overall, clinical scores for patients with severe HO were evidently lower compared to the total patient group. However, differences between the approaches could not be tested due to the small patient number.
It is clear that severe HO formation decreases clinical outcomes. However, further research with a higher number of patients with severe HO formation is necessary to define the effect of surgical approach on severe HO formation since a low Brooker grade (1–3) does not seem to impact outcomes [24]. However, given the fact that no revisions for HO were performed in our cohort, the clinical relevance of HO formation can be questioned. Nevertheless, this knowledge can be of interest for clinical decision making and future studies in the field of THA approaches since it seems that more tissue damage is associated with more HO formation. Especially in patients with pre-existent risk factors for the formation of HO, one could consider minimizing the risk of developing HO when choosing the surgical approach.
This is the first large, long-term, prospective cohort study that compares the prevalence of HO between these two approaches. However, this study has some limitations. First, only two approaches were compared. Second, no randomization was performed. However, all measurements were performed twice by two authors who were blinded for surgical approach. Nevertheless, it was not possible to correct for unknown confounding factors that may affect HO formation. Third, the data on duration of NSAID use were not optimal. Long-term NSAID use may influence the (amount of) HO formation [25, 26]. However, there is no reason to assume the use of NSAIDs was different between groups. Furthermore, Haffer et al. showed that diclofenac is efficacious in the prevention of HO when started the first day postoperative for a minimum of 9 days [27]. In the Netherlands, all hospitals follow standard protocols for postoperative NSAID use with at least a 14-day prescription.
The current study shows the difference in HO formation after THA with PA or DLA. The good clinical scores and high follow-up rate show that the THA technique used in the current study is functioning well. Due to the presence of several confounding factors associated with the different approaches, this study cannot draw any conclusions with regard to the influence of HO formation on clinical outcomes. Due to the small number of patients with severe HO formation, this study cannot draw any conclusions with regard to the influence of approach on severe HO formation. A large, long-term randomized controlled trial comparing approaches can assess with which approach most (severe) HO formation occurs. The resulting frequencies of HO formation and clinical outcome scores can eventually determine the influence of the different approaches in THA.
In conclusion, this study shows that DLA for THA is associated with more radiological HO formation compared to the PA. However, there is no difference in the prevalence of radiological severe HO. No revisions were performed because of HO within the 6-year follow-up after THA. Long-term clinical trials are needed to assess the influence of approach on HO formation and clinical outcome scores.
References
Berger RA, Jacobs JJ, Meneghini RM et al (2004) Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res 429:239–247. https://doi.org/10.1097/01.blo.0000150127.80647.80
Barrett WP, Turner SE, Leopold JP (2013) Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty 28:1634–1638. https://doi.org/10.1016/J.ARTH.2013.01.034
Kaplan FS, Glaser DL, Hebela N, Shore EM (2004) Heterotopic ossification. J Am Acad Orthop Surg 12:116–125. https://doi.org/10.5435/00124635-200403000-00007
Ranganathan K, Loder S, Agarwal S et al (2015) Heterotopic Ossification. J Bone Jt Surg 97:1101–1111. https://doi.org/10.2106/JBJS.N.01056
Kocic M, Lazovic M, Mitkovic M, Djokic B (2010) Clinical significance of the heterotopic ossification after total hip arthroplasty. Orthopedics 33:16. https://doi.org/10.3928/01477447-20091124-13
Alijanipour P, Patel RP, Naik TU, Parvizi J (2017) Heterotopic ossification in primary total hip arthroplasty using the direct anterior vs direct lateral approach. J Arthroplasty 32:1323–1327. https://doi.org/10.1016/j.arth.2016.11.030
Iorio R, Healy WL (2002) Heterotopic ossification after hip and knee arthroplasty: risk factors, prevention, and treatment. J Am Acad Orthop Surg 10:409–416. https://doi.org/10.5435/00124635-200211000-00005
Nayak KN, Mulliken B, Rorabeck CH et al (1997) Prevalence of heterotopic ossification in cemented versus noncemented total hip joint replacement in patients with osteoarthrosis: a randomized clinical trial. Can J Surg 40:368–374
Ahrengart L, Lindgren U (1993) Heterotopic bone after hip arthroplasty. Defining the patient at risk. Clin Orthop Relat Res 153–159
Anthonissen J, Steffen CT, Alessandri B et al (2020) Traumatic brain injury enhances the formation of heterotopic ossification around the hip: an animal model study. Arch Orthop Trauma Surg 140:1029–1035. https://doi.org/10.1007/s00402-019-03326-0
Rosteius T, Rausch V, Pätzholz S et al (2019) Incidence and risk factors for heterotopic ossification following periprosthetic joint infection of the hip. Arch Orthop Trauma Surg 139:1307–1314. https://doi.org/10.1007/s00402-019-03215-6
Pai VS (1994) Heterotopic ossification in total hip arthroplasty. The influence of the approach. J Arthroplasty 9:199–202. https://doi.org/10.1016/0883-5403(94)90069-8
Morrey BF, Adams RA, Cabanela ME (1984) Comparison of heterotopic bone after anterolateral, transtrochanteric, and posterior approaches for total hip arthroplasty. Clin Orthop Relat Res 160–7
Hürlimann M, Schiapparelli F-F, Rotigliano N et al (2017) Influence of surgical approach on heterotopic ossification after total hip arthroplasty—is minimal invasive better? A case control study. BMC Musculoskelet Disord 18:27. https://doi.org/10.1186/s12891-017-1391-x
Snijders TE, Halma JJ, Massier JRA et al (2019) The survivorship of the uncemented iso-elastic monoblock acetabular component at a mean of 6-year follow-up. HSS J 16:15–22. https://doi.org/10.1007/s11420-018-09658-8
Massier JRA, Van Erp JHJ, Snijders TE, Gast ADE (2020) A vitamin E blended highly cross-linked polyethylene acetabular cup results in less wear: 6-year results of a randomized controlled trial in 199 patients. Acta Orthop. https://doi.org/10.1080/17453674.2020.1807220
van Erp JHJ, Massier JRA, Halma JJ et al (2020) 2-year results of an RCT of 2 uncemented isoelastic monoblock acetabular components: lower wear rate with vitamin E blended highly cross-linked polyethylene compared to ultra-high molecular weight polyethylene. Acta Orthop 3674:1–6. https://doi.org/10.1080/17453674.2020.1730073
Brooker AF, Bowerman JW, Robinson RA, Riley LH (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Van Oldenrijk J, Hoogland PVJM, Tuijthof GJM et al (2010) Soft tissue damage after minimally invasive THA: a comparison of 5 approaches. Acta Orthop 81:696–702. https://doi.org/10.3109/17453674.2010.537804
Nilsson OS, Persson P-E (1999) Heterotopic bone formation after joint replacement. Curr Opin Rheumatol 11:127–131. https://doi.org/10.1097/00002281-199903000-00008
Meyers C, Lisiecki J, Miller S et al (2019) Heterotopic ossification: a comprehensive review. JBMR Plus 3:e10172. https://doi.org/10.1002/jbm4.10172
Zran N, Joseph E, Callamand G et al (2020) Heterotopic ossification after total hip arthroplasty: radiological comparison between a direct anterior approach without an orthopaedic table and a posterior approach. Hip Int J Clin Exp Res hip Pathol Ther. https://doi.org/10.1177/1120700020970793
Amlie E, Havelin LI, Furnes O et al (2014) Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty A cross-sectional questionnaire study of 1,476 patients 1–3 years after surgery. Acta Orthop 85:463–469. https://doi.org/10.3109/17453674.2014.934183
Rüdiger HA, Dittrich M, Robinson J et al (2020) The impact of heterotopic ossification on self-reported outcomes after total hip arthroplasty using the direct anterior approach. J Bone Joint Surg Am 102:91–98. https://doi.org/10.2106/JBJS.20.00071
Gebuhr P, Wilbek H, Soelberg M (1995) Naproxen for 8 Days Can Prevent Heterotopic Ossification After Hip Arthroplasty. Clin Orthop Relat Res
Winkler S, Springorum HR, Vaitl T et al (2016) Comparative clinical study of the prophylaxis of heterotopic ossifications after total hip arthroplasty using etoricoxib or diclofenac. Int Orthop 40:673–680. https://doi.org/10.1007/s00264-015-3077-z
Haffer H, Müller M, Ascherl R et al (2020) Diclofenac for prophylaxis of heterotopic ossification after hip arthroplasty: a systematic review. Hip Int J Clin Exp Res hip Pathol Ther. https://doi.org/10.1177/1120700020978194
Funding
Funded by Clinical Orthopedic Research Center, mN.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by JHJE, JRAM and ST. The first draft of the manuscript was written by JHJE and JRAM, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
This study was approved by the local institutional review board.
Consent to participate
All the authors agreed to participate.
Consent for publication
All the authors are in agreement with the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Erp, J.H.J., Massier, J.R.A., Truijen, S. et al. Heterotopic ossification in primary total hip arthroplasty using the posterolateral compared to the direct lateral approach. Arch Orthop Trauma Surg 141, 1253–1259 (2021). https://doi.org/10.1007/s00402-021-03783-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03783-6