Abstract
Purpose
Supraventricular tachyarrhythmias are a major cause of inappropriate defibrillator shocks. Sleep-disordered breathing (SDB) is a known risk factor for atrial fibrillation (AF). We hypothesized that Cheyne–Stokes respiration (CSA) and obstructive sleep apnea (OSA) have an impact on inappropriate defibrillator discharges in patients witch chronic heart failure (CHF) and cardiac resynchronization therapy with defibrillator (CRT-D).
Methods
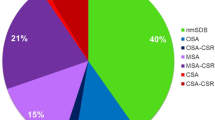
In this study, 172 patients with CHF (LVEF ≤ 45 %, NYHA-class ≥ 2) and CRT-D underwent overnight polygraphy; 54 had no SDB (apnea–hypopnea index < 5/h), 59 had OSA, and 59 had CSA. During follow-up (36 months), inappropriate defibrillator shocks were documented.
Results
In all, 17 patients had inappropriate defibrillator shocks (9.9 %; eight oversensing due to lead fractures, five caused by atrial fibrillation, four because of sinus tachycardia). Mean event-free survival time was 33.5 ± 1.2 months in the CSA group, 35.2 ± 0.7 months in the OSA group, and 32.1 ± 1.5 months in the no SDB group, respectively (CSA vs. no SDB p = 0.63; OSA vs. no SDB p = 0.31; CSA vs. OSA p = 0.45). Stepwise Cox proportional hazard regression analysis revealed an independent association for age (per year: hazard ratio 0.90, 95 % confidence interval 0.85–0.96, p < 0.001), but not for any kind of SDB.
Conclusions
SDB was not associated with inappropriate defibrillator shocks. We assume this is due to the low incidenceand low proportion of inappropriate therapies in response to AF.
Zusammenfassung
Hintergrund
Supraventrikuläre Arrhythmien sind eine häufige Ursache für inadäquate Schocks durch implantierbare Kardioverter-Defibrillatoren (ICD). Schlafbezogene Atmungsstörungen (SBAS) gelten als Risikofaktor für das Auftreten von Vorhofflimmern (AF). Ziel dieser Studie war es daher zu untersuchen, ob die Cheyne-Stokes-Atmung (CSA) oder die obstruktive Schlafapnoe (OSA) das Auftreten inadäquater ICD-Schocks bei Patienten mit chronischer Herzinsuffizienz (CHF) und kardialer Resynchronisationstherapie mit Defibrillator (CRT-D) beeinflussen.
Methodik
172 Patienten mit CHF (linksventrikuläre Ejektionsfraktion, LVEF: ≤ 45 %, New-York-Heart-Association(NYHA)-Klasse ≥ 2) und CRT-D durchliefen eine nächtliche Polygraphie. Nachfolgend wurden während des 36-monatigen Follow-up inadäquate ICD-Schocks dokumentiert.
Ergebnisse
Bei 59 Patienten konnte eine OSA, bei 59 Patienten eine CSA und bei 54 Patienten keine SBAS (Apnoe-Hypopnoe-Index < 5/h) dokumentiert werden. 17 Patienten waren von inadäquaten Schocks betroffen (9,9 %); 8 bei Oversensing aufgrund eines Sondendefekts, 5 wegen Vorhofflimmern, 4 aufgrund von Sinustachykardien). Das mittlere ereignisfreie Überleben betrug 33,5 ± 1,2 Monate in der CSA-Gruppe, 35,2 ± 0,7 Monate in der OSA-Gruppe und 32,1 ± 1,5 Monate bei Patienten ohne SBAS (CSA vs. keine SBAS: p = 0,63; OSA vs. keine SBAS: p = 0,31; CSA vs. OSA: p = 0,45). In der Stepwise-Cox-proportional-Hazard-Regressionsanalyse zeigte sich einzig das Patientenalter (pro Jahr: Hazard Ratio 0,90; 95%-Konfidenzintervall: 0,85 bis 0,96; p < 0,001), nicht jedoch die SBAS als ein unabhängiger Risikofaktor.
Schlussfolgerung
Eine Assoziation zwischen SBAS und inadäquaten ICD-Schocks konnte nicht nachgewiesen werden. Dies scheint begründet in einer geringen Inzidenz sowie einem geringen Anteil inadäquater Schocks aufgrund von AF.
.

Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud JB, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Tregaer S, Reston J, Schoelles K, Phillps B (2009) Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med 5:573–581
Prinz C, Bitter T, Piper C, Horstkotte D, Faber L, Oldenburg O (2010) Sleep apnea is common in patients with coronary artery disease. Wien Med Wochenschr 160:349–355
Bitter T, Prinz C, Faber L, Hering D, Langer C, Horstkotte D et al (2009) Sleep-disordered breathing in heart failure with normal left ventricular ejection fraction. Eur J Heart Fail 11:602–608
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Töpfer V (2007) Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9:251–257
Bitter T, Langer C, Vogt J, Lange M, Horstkotte D, Oldenburg O (2009) Sleep-disordered breathing in patients with atrial fibrillation and normal systolic left ventricular function. Dtsch Ärztebl Int 106:164–170
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Strömberg A et al (2008) Task force for diagnosis and treatment of acute and chronic heart failure 2008 of European Society of Cardiology. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 10:933–989
Merit-HF Study Group (1999) Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 353:2001–2007
Goldenberg I, Gillespie J, Moss AJ, Hall WJ, Klein H, McNitt S, Brown MW, et al (2010) Executive committee of the multicenter automatic defibrillator implantation trial II. Long-term benefit of primary prevention with an implantable cardioverter-defibrillator: an extended 8-year follow-up study of the Multicenter automatic defibrillator implantation trial II. Circulation 122:1265–1271
Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA 3rd et al (2009) MADIT-CRT Trial Investigators. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med 36:1329–1338
Dichtl W, Wolber T, Paoli U, Brüllmann S, Stühlinger M, Berger T, Spuller K et al (2011) Appropriate therapy but not inappropriate shocks predict survival in implantable cardioverter defibrillator patients. Clin Cardiol 34:433–436
Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK et al (2008) Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med 359:1009–1017
Daubert JP, Zareba W, Cannom DS, McNitt S, Rosero SZ, Wang P, Schuger C et al (2008) MADIT Investigators. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II. J Am Coll Cardiol 51:1357–1365
Bitter T, Westerheide N, Prinz C, Hossain MS, Vogt J, Langer C, Horstkotte D, Oldenburg O (2011) Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J 32:61–74
Gami AS, Hodge DO, Herges RM, Olsson EJ, Nykodym J, Kara T, Somers VK (2007) Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol 49:565–571
Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, Shamsuzzaman AS, Somers VK (2003) Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation 107:2589–2594
Bitter T, Nölker G, Vogt J, Prinz C, Horstkotte D, Oldenburg O (2012) Predictors of recurrence in patients undergoing cryoballoon ablation for treatment of atrial fibrillation: the independent role of sleep-disordered breathing. J Cardiovasc Electrophysiol 23:18–25
Iliceto S, Dambrosio M, Sorino M, D’Ambrosio G, Amico A, Fiore T, Rizzon P (1988) Effects of acute intrathoracic pressure changes on left ventricular geometry and filling. Am Heart J 116:155–465
Dickstein K, Vardas PE, Auricchio A, Daubert JC, Linde C, Mc Murray J, Ponikowski P et al (2010) Committee for practice guidelines of the European Society of Cardiology. 2010 focused update of ESC Guidelines on device therapy in heart failure: an update of the 2008 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC guidelines for cardiac resynchronisation therapy. Developed with the special contribution of the Heart Failure Assocation and the European Heart Rhythm Association. Eur J Heart Fail 12:1143–1153
Iber C, Ancoli-Israel S, Chesson AL Jr, Quan SF (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. AASM Manual for Scoring Sleep, Westchester, IL
Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS et al (2003) ACC; AHA; ASE. Guideline update for the clinical application of echocardiography: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to update the 1997 guidelines for the clinical application of echocardiography). J Am Soc Echocardiogr 16:1091–1110
Read DJ (1967) A clinical method for assessing the ventilatory response to carbon dioxide. Australasian Ann Medi 16:20–32
Theuns DA, Klootwijk AP, Goedhart DM, Jordaens LJ (2004) Prevention of inappropriate therapy in implantable cardioverter-defibrillators: results of a prospective, randomized study of tachyarrhythmia detection algorithms. J Am Coll Cardiol 44:2362–2367
Sinha AM, Stellbrink C, Schuchert A, Mox B, Jordaens L, Lamaison D, Gill J et al (2004) Clinical expirience with a new detection algorithm for differentiation of supraventricular from ventricular tachycardia in a dual-chamber defibrillator. J Cardiovasc Electrophysiol 15:646–652
Toquero J, Alzueta J, Mont L, Lozano IF, Barrera A, Berruezo A, Castro V et al (2009) Morphology discrimination criterion wavelet improves rhythm discrimination in single chamber implantable cardioverter-defibrillators: Spanish register of morphology discrimination criterion wavelet (REMEDIO). Europace 11:727–733
Jacq F, Foulldrin G, Savouré A, Anselme F, Baquelin-Pinaud A, Cribier A, Thibaut F (2009) A comparison of anxiety, depression and quality of life between device shock and nonshock groups in implantable cardioverter defibrillator recipients. Gen Hosp Psychiat 31:266–273
Weber M, Block M, Brunn J, Bänsch D, Böcker D, Hammel D, Gietzen F, Breithardt G (1996) Inadequate therapies with implantable cardioverter-defibrillators–incidence, etiology, predictive factors and preventive strategies. Z Kardiol 85:809–819
Nagai T, Satomi K, Noda T, Okamura H, Yamada Y, Shimizu W, Suyama K et al (2010) Relationship between oral amiodarone and inappropriate therapy from an implantable cardioverter defibrillator. Circulation J 74:1302–1307
Friedman PA, McClelland RL, Bamlet WR, Acosta H, Kessler D, Munger TM, Kavesh NG et al (2006) Dual chamber versus single-chamber detection enhancements for implantable defibrillator rhythm diagnosis: the detect supraventricular tachycardia study. Circulation 113:2871–2879
Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, Sahadevan J, Redline S, Sleep Heart Health Study (2006) Association of nocturnal arrhythmias with sleep-disordered breathing: the sleep heart health study. Am J Respir Crit Care Med 173:910–916
Desai H, Aronows WS, Ahn C, Gandhi K, Hussain S, Lai HM, Sharma M et al (2010) Risk factors for appropriate cardioverter-defibrillator shocks, inappropriate cardioverter-defibrillator shocks, and time to mortality in 549 patients with heart failure. Am J Cardiol 105:336–338
Stevenson IH, Teichtahl H, Cunnington D, Ciavarella S, Gordon I, Kalman JM (2008) Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J 29:1662–1669
Porthan KM, Melin JH, Kupila JT, Venho KK, Partinen MM (2004) Prevalence of sleep apnea syndrome in lone atrial fibrillation: a case-control study. Chest 125:879–885
Braga B, Poyares D, Cintra F, Guilleminault C, Cirenza C, Horbach S, Macedo D et al (2009) Sleep-disordered breathing and chronic atrial fibrillation. Sleep Med 10:212–216
Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, Malouf JF et al (2004) Association of atrial fibrillation and obstructive sleep apnea. Circulation 110:364–367
Kreuz J, Skowasch D, Horlbeck F, Atzinger C, Schrickel JW, Lorenzen H, Nickenig G, Schwab JO (2013) Usefulness of sleep-disordered breathing to predict occurrence of appropriate and inappropriate implantable-cardioverter defibrillator therapy in patients with implantable cardioverter-defibrillator for primary prevention of sudden cardiac death. Am J Cardiol 111:1319–1323
Oliveira W, Campos O, Cintra F, Matos L, Vieira M, Ponchirolli A, De Paola AA et al (2008) Left atrial volume and function in patients with obstructive sleep apnea assessed by real-time three dimensional echocardiography. J Am Soc Echocardiogr 21:1355–1361
Franz MF, Bode R (2003) Mechano-electrical feedback underlying arrhythmias: the atrial fibrillation case. Progr Biophys Mol Biol 82:163–174
Korte T, Ködlitz H, Niehaus M, Paul T, Tebbenjohanns J (2004) High incidence of appropriate and inappropriate ICD therapies in children and adolescents with implantable cardioverter defibrillator. Pacing Clin Electrophysiol 27:924–932
Morrison TB, Rea RF, Hodge DO, Crusan D, Koestler C, Asirvatham SJ, Bradley D et al (2010) Risk factors for implantable defibrillator lead fracture in a recalled and a nonrecalled lead. J Cardiovasc Electrophysiol 21:671–677
Love BA, Barrett KS, Alexander ME, Bevillacqua LM, Epstein MR, Triedman JK, Walsh EP, Berul CI (2001) Supraventricular arrhythmias in children and young adults with implantable cardioverter defibrillators J Cardiovasc Electrophysiol 12:1097–1101
Moss AJ, Schuger C, Beck CA, Brown MW, Cannom DS, Daubert JP, Estes NA 3rd et al (2012) MADIT-RIT trial investigators.Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med 367:2275–2283
Dingli K, Coleman EL, Vennelle M, Finch SP, Wraith PK, Mackay TW, Douglas NJ (2003) Evaluation of a portable device for diagnosing the sleep apnoea/hypopnoea syndrome. Eur Respir J 21:253–259
Oldenburg O, Lamp B, Freivogel K, Bitter T, Langer C, Horstkotte D (2008) Low night-to-night variability of sleep disordered breathing in patients with stable congestive heart failure. Clin Res Cardiol 97:899–904
Compliance with ethical guidelines
Conflict of interest
T. Bitter and O. Oldenburg state that they have received travel expenses from ResMed Germany. K.-J. Gutleben has received travel expenses from Biotronik, Sorin, and St. Jude Medical. J. Vogt has received travel expenses from Biotronik, Medtronic Inc., and St. Jude Medical. G. Nölker has received travel expenses from Medtronic and Biotronik. Z. Dimitriadis, C. Prinz, and D. Horstkotte state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
T. Bitter and K.-J. Gutleben contributed equally to the study and the manuscript.
Rights and permissions
About this article
Cite this article
Bitter, T., Gutleben, KJ., Nölker, G. et al. Sleep-disordered breathing and inappropriate defibrillator shocks in chronic heart failure. Herzschr Elektrophys 25, 198–205 (2014). https://doi.org/10.1007/s00399-014-0324-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-014-0324-8
Keywords
- Heart failure
- Inappropriate defibrillator shocks
- Sleep-disordered breathing
- Cardiac resynchronization therapy
- Incidence