Abstract
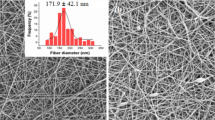
In this research, hydrogels based on chitosan, pectin, and salt (NaCl) were synthesized through the formation of polyelectrolyte complexes (PECs). The synthesis parameters, including pH, salinity, and polymer concentration, were varied to explore their influence. Weight and texture analysis revealed differences in hydrogel morphology. Swelling behavior studies showed hydrogels synthesized at pH 4 exhibiting higher swelling capacities. Additionally, the presence of salt affected the formation process. Thermal characterization showed a first decomposition step occurring around 180–224 °C. Morphological testing using SEM highlighted differences in pore size and distribution, notably when salt was included in the formulation (pore wall diameter without NaCl, 2.2 ± 1.1 um, with NaCl, 4.7 ± 1.2 um). Physico-chemical tests, including Zeta potential, FTIR, and XRD, provided insights into interactions within the hydrogels: hydrogen bonds and electrostatic interactions. Moreover, antibacterial tests demonstrated efficacy against Escherichia coli and Staphylococcus aureus, with varying inhibition degrees correlated with NaCl content (halo for E. coli without NaCl, 8 and 10 mm; with NaCl, 10 and 15 mm). Further assessments, including water vapor transmission rate (WVTR) and lidocaine release assays, highlighted hydrogel potential for wound dressing applications, with suitable moisture retention properties and controlled drug release capabilities. The release percentage achieved by the hydrogel with 0.15 M NaCl was higher than without salt (111.1% ± 9.5% and 31.16% ± 15.13%, respectively). Preliminary in vivo wound healing studies showed promising results. Overall, our findings emphasize the tunable properties of these hydrogels and their potential for wound dressings.







Similar content being viewed by others
Availability of data and materials
All experimental data, materials, and methods used in this research are available to other researchers upon request. Additionally, all data and results presented in this article are supported by the provided materials, methods, and custom analysis software. Further details on data and materials can be obtained by contacting the authors.
References
Xu J, Tsai Y-L, Hsu S (2020) Design strategies of conductive hydrogel for biomedical applications. Molecules 25:5296. https://doi.org/10.3390/molecules25225296
Srivastava S, Levi AE, Goldfeld DJ, Tirrell MV (2020) Structure, morphology, and rheology of polyelectrolyte complex hydrogels formed by self-assembly of oppositely charged triblock polyelectrolytes. Macromolecules 53:5763–5774. https://doi.org/10.1021/acs.macromol.0c00847
Costa RR, Soares da Costa D, Reis RL, Pashkuleva I (2019) Bioinspired baroplastic glycosaminoglycan sealants for soft tissues. Acta Biomater 87:108–117. https://doi.org/10.1016/j.actbio.2019.01.040
Reisch A, Tirado P, Roger E et al (2013) Compact saloplastic poly(acrylic acid)/poly(allylamine) complexes: kinetic control over composition, microstructure, and mechanical properties. Adv Funct Mater 23:673–682. https://doi.org/10.1002/adfm.201201413
Elnashar M (2011) Biotechnology of biopolymers. BoD–Books on Demand
Martinez YN, Piñuel L, Castro GR, Breccia JD (2012) Polyvinyl alcohol-pectin cryogel films for controlled release of enrofloxacin. Appl Biochem Biotechnol 167:1421–1429. https://doi.org/10.1007/s12010-012-9554-6
Dai T, Tanaka M, Huang Y-Y, Hamblin MR (2011) Chitosan preparations for wounds and burns: antimicrobial and wound-healing effects. Expert Rev Anti Infect Ther 9:857–879. https://doi.org/10.1586/eri.11.59
Wu X, Sun H, Qin Z et al (2020) Fully physically crosslinked pectin-based hydrogel with high stretchability and toughness for biomedical application. Int J Biol Macromol 149:707–716. https://doi.org/10.1016/j.ijbiomac.2020.01.297
Mangoni ML, McDermott AM, Zasloff M (2016) Antimicrobial peptides and wound healing: biological and therapeutic considerations. Exp Dermatol 25:167–173. https://doi.org/10.1111/exd.12929
Eroglu E, Eroglu F, Agalar F et al (2001) The effect of lidocaine/prilocaine cream on an experimental wound healing model. Eur J Emerg Med Off J Eur Soc Emerg Med 8:199–201. https://doi.org/10.1097/00063110-200109000-00007
Weinschenk S, Mergenthaler C, Armstrong C et al (2017) Local anesthetics, procaine, lidocaine, and mepivacaine show vasodilatation but no type 1 allergy: a double-blind, placebo-controlled study. BioMed Res Int 2017:9804693. https://doi.org/10.1155/2017/9804693
Waite A, Gilliver SC, Masterson GR et al (2010) Clinically relevant doses of lidocaine and bupivacaine do not impair cutaneous wound healing in mice. Br J Anaesth 104:768–773. https://doi.org/10.1093/bja/aeq093
Pourmohammadi-Bejarpasi Z, Sabzevari R, Mohammadi Roushandeh A et al (2022) Combination therapy of metadichol nanogel and lipocalin-2 engineered mesenchymal stem cells improve wound healing in rat model of excision injury. Adv Pharm Bull 12:550–560. https://doi.org/10.34172/apb.2022.059
Morris G, Kök S, Harding S, Adams G (2010) Polysaccharide drug delivery systems based on pectin and chitosan. Biotechnol Genet Eng Rev 27:257–284. https://doi.org/10.1080/02648725.2010.10648153
Neufeld L, Bianco-Peled H (2017) Pectin–chitosan physical hydrogels as potential drug delivery vehicles. Int J Biol Macromol 101:852–861. https://doi.org/10.1016/j.ijbiomac.2017.03.167
da Costa MPM, de Mello Ferreira IL, de Macedo Cruz MT (2016) New polyelectrolyte complex from pectin/chitosan and montmorillonite clay. Carbohydr Polym 146:123–130. https://doi.org/10.1016/j.carbpol.2016.03.025
Amirian J, Zeng Y, Shekh MI et al (2021) In-situ crosslinked hydrogel based on amidated pectin/oxidized chitosan as potential wound dressing for skin repairing. Carbohydr Polym 251:117005. https://doi.org/10.1016/j.carbpol.2020.117005
Chetouani A, Follain N, Marais S et al (2017) Physicochemical properties and biological activities of novel blend films using oxidized pectin/chitosan. Int J Biol Macromol 97:348–356. https://doi.org/10.1016/j.ijbiomac.2017.01.018
Shanti SK, Aprilita NH, Siswanta D (2022) Sodium dodecyl sulfate adsorption on sulfuric acid-crosslinked chitosan/pectin polyelectrolyte complex film. Key Eng Mater 920:43–50. https://doi.org/10.4028/p-k915ls
Li D, Wang S, Meng Y et al (2020) An injectable, self-healing hydrogel system from oxidized pectin/chitosan/γ-Fe2O3. Int J Biol Macromol 164:4566–4574. https://doi.org/10.1016/j.ijbiomac.2020.09.072
Martins JG, Camargo SEA, Bishop TT et al (2018) Pectin-chitosan membrane scaffold imparts controlled stem cell adhesion and proliferation. Carbohydr Polym 197:47–56. https://doi.org/10.1016/j.carbpol.2018.05.062
Dziadek M, Dziadek K, Salagierski S et al (2022) Newly crosslinked chitosan- and chitosan-pectin-based hydrogels with high antioxidant and potential anticancer activity. Carbohydr Polym 290:119486. https://doi.org/10.1016/j.carbpol.2022.119486
Mohan P, Rangari VD, Kesavan K (2022) Cationic chitosan/pectin polyelectrolyte nanocapsules of moxifloxacin as novel topical management system for bacterial keratitis. Curr Eye Res 47:1498–1507. https://doi.org/10.1080/02713683.2022.2124274
Vildanova RR, Petrova SF, Kolesov SV, Khutoryanskiy VV (2023) Biodegradable hydrogels based on chitosan and pectin for cisplatin delivery. Gels 9:342. https://doi.org/10.3390/gels9040342
Schröder P, Cord-Landwehr S, Schönhoff M, Cramer C (2023) Composition and charge compensation in chitosan/gum arabic complex coacervates in dependence on pH and salt concentration. Biomacromol 24:1194–1208. https://doi.org/10.1021/acs.biomac.2c01255
Wang W, Feng Y, Chen W et al (2021) Citrus pectin modified by microfluidization and ultrasonication: improved emulsifying and encapsulation properties. Ultrason Sonochem 70:105322. https://doi.org/10.1016/j.ultsonch.2020.105322
Ali SM, Yosipovitch G (2013) Skin pH: from basic science to basic skin care. Acta Derm Venereol 93:261–267. https://doi.org/10.2340/00015555-1531
Pereda M, Ponce AG, Marcovich NE et al (2011) Chitosan-gelatin composites and bi-layer films with potential antimicrobial activity. Food Hydrocoll 25:1372–1381. https://doi.org/10.1016/j.foodhyd.2011.01.001
Gonzalez JS, Ludueña LN, Ponce A, Alvarez VA (2014) Poly(vinyl alcohol)/cellulose nanowhiskers nanocomposite hydrogels for potential wound dressings. Mater Sci Eng C Mater Biol Appl 34:54–61. https://doi.org/10.1016/j.msec.2013.10.006
Long J, Etxeberria AE, Nand AV et al (2019) A 3D printed chitosan-pectin hydrogel wound dressing for lidocaine hydrochloride delivery. Mater Sci Eng C 104:109873. https://doi.org/10.1016/j.msec.2019.109873
Abou-Okeil A, Rehan M, El-Sawy SM et al (2018) Lidocaine/β-cyclodextrin inclusion complex as drug delivery system. Eur Polym J 108:304–310. https://doi.org/10.1016/j.eurpolymj.2018.09.016
Bagher Z, Ehterami A, Safdel M et al (2019) Wound healing with alginate/chitosan hydrogel containing hesperidin in rat model. J Drug Deliv Sci Technol 55:101379. https://doi.org/10.1016/j.jddst.2019.101379
Allan JR, Wilson CG (1971) Influence of acclimatization on sweat sodium concentration. J Appl Physiol 30:708–712. https://doi.org/10.1152/jappl.1971.30.5.708
Kowalski G, Kijowska K, Witczak M et al (2019) Synthesis and effect of structure on swelling properties of hydrogels based on high methylated pectin and acrylic polymers. Polymers 11:114. https://doi.org/10.3390/polym11010114
Elliott JE, Macdonald M, Nie J, Bowman CN (2004) Structure and swelling of poly(acrylic acid) hydrogels: effect of pH, ionic strength, and dilution on the crosslinked polymer structure. Polymer 45:1503–1510. https://doi.org/10.1016/j.polymer.2003.12.040
De Yao K, Liu J, Cheng GX et al (1996) Swelling behavior of pectin/chitosan complex films. J Appl Polym Sci 60:279–283. https://doi.org/10.1002/(SICI)1097-4628(19960411)60:2%3c279::AID-APP16%3e3.0.CO;2-0
Hanna DH, Lotfy VF, Basta AH, Saad GR (2020) Comparative evaluation for controlling release of niacin from protein- and cellulose-chitosan based hydrogels. Int J Biol Macromol 150:228–237. https://doi.org/10.1016/j.ijbiomac.2020.02.056
Proksch E (2018) pH in nature, humans and skin. J Dermatol 45:1044–1052. https://doi.org/10.1111/1346-8138.14489
Hariri HH, Schlenoff JB (2010) Saloplastic macroporous polyelectrolyte complexes: cartilage mimics. Macromolecules 43:8656–8663. https://doi.org/10.1021/ma1012978
Gao Y, Wang Y, Dai Y et al (2022) Amylopectin based hydrogel strain sensor with good biocompatibility, high toughness and stable anti-swelling in multiple liquid media. Eur Polym J 164:110981. https://doi.org/10.1016/j.eurpolymj.2021.110981
Maciel VBV, Yoshida CMP, Franco TT (2015) Chitosan/pectin polyelectrolyte complex as a pH indicator. Carbohydr Polym 132:537–545. https://doi.org/10.1016/j.carbpol.2015.06.047
Hanna DH, El-Mazaly MH, Mohamed RR (2023) Synthesis of biodegradable antimicrobial pH-sensitive silver nanocomposites reliant on chitosan and carrageenan derivatives for 5-fluorouracil drug delivery toward HCT116 cancer cells. Int J Biol Macromol 231:123364. https://doi.org/10.1016/j.ijbiomac.2023.123364
El-Maadawy MW, Mohamed RR, Hanna DH (2022) Preparation of carrageenan/ chitosan-based (N, N, N-trimeth(yl chitosan chloride) silver nanocomposites as pH sensitive carrier for effective controlled curcumin delivery in cancer cells. OpenNano 7:100050. https://doi.org/10.1016/j.onano.2022.100050
Zhang M, Zhao X (2020) Alginate hydrogel dressings for advanced wound management. Int J Biol Macromol 162:1414–1428. https://doi.org/10.1016/j.ijbiomac.2020.07.311
Chang C, He M, Zhou J, Na N (2011) Swelling behaviors of pH- and salt-responsive cellulose-based hydrogels. Macromolecules 44:. https://doi.org/10.1021/ma102801f
Hanna DH, Hamed AA, Saad GR (2023) Synthesis and characterization of poly(3-hydroxybutyrate)/chitosan-graft poly (acrylic acid) conjugate hyaluronate for targeted delivery of methotrexate drug to colon cancer cells. Int J Biol Macromol 240:124396. https://doi.org/10.1016/j.ijbiomac.2023.124396
Porcel CH, Schlenoff JB (2009) Compact polyelectrolyte complexes: “saloplastic” candidates for biomaterials. Biomacromol 10:2968–2975. https://doi.org/10.1021/bm900373c
Rydzek G, Pakdel A, Witecka A et al (2018) pH-responsive saloplastics based on weak polyelectrolytes: from molecular processes to material scale properties. Macromolecules 51:4424–4434. https://doi.org/10.1021/acs.macromol.8b00609
Schaaf P, Schlenoff JB (2015) Saloplastics: processing compact polyelectrolyte complexes. Adv Mater 27:2420–2432. https://doi.org/10.1002/adma.201500176
Ozmen MM, Okay O (2005) Superfast responsive ionic hydrogels with controllable pore size. Polymer 46:8119–8127. https://doi.org/10.1016/j.polymer.2005.06.102
Naficy S, Dehghani F, Chew YV et al (2020) Engineering a porous hydrogel-based device for cell transplantation. ACS Appl Bio Mater 3:1986–1994. https://doi.org/10.1021/acsabm.9b01144
Zhang M, Zeng G, Pan Y, Qi N (2018) Difference research of pectins extracted from tobacco waste by heat reflux extraction and microwave-assisted extraction. Biocatal Agric Biotechnol 15:. https://doi.org/10.1016/j.bcab.2018.06.022
Trinca RB, Westin CB, da Silva JAF, Moraes ÂM (2017) Electrospun multilayer chitosan scaffolds as potential wound dressings for skin lesions. Eur Polym J 88:161–170. https://doi.org/10.1016/j.eurpolymj.2017.01.021
Sofos J (2007) Antimicrobial effects of sodium and other ions in foods: a review. J Food Saf 6:45–78. https://doi.org/10.1111/j.1745-4565.1984.tb00478.x
Jantsch J, Schatz V, Friedrich D et al (2015) Cutaneous Na+ storage strengthens the antimicrobial barrier function of the skin and boosts macrophage-driven host defense. Cell Metab 21:493–501. https://doi.org/10.1016/j.cmet.2015.02.003
Goy RC, de Britto D, Assis OBG (2009) A review of the antimicrobial activity of chitosan. Polímeros 19:241–247. https://doi.org/10.1590/S0104-14282009000300013
Qin C, Li H, Xiao Q et al (2006) Water-solubility of chitosan and its antimicrobial activity. Carbohydr Polym 63:367–374. https://doi.org/10.1016/j.carbpol.2005.09.023
Abu Elella MH, Sabaa Magdy W, Hanna DH et al (2020) Antimicrobial pH-sensitive protein carrier based on modified xanthan gum. J Drug Deliv Sci Technol 57:101673. https://doi.org/10.1016/j.jddst.2020.101673
Men’shikov DD, Lazareva EB, Popova TS et al (1997) Antimicrobial properties of pectins and their effects on antibiotics. Antibiot Khimioterapiia Antibiot Chemoterapy Sic 42:10–15
Xu R, Xia H, He W et al (2016) Controlled water vapor transmission rate promotes wound-healing via wound re-epithelialization and contraction enhancement. Sci Rep 6:24596. https://doi.org/10.1038/srep24596
Ujang Z, Rashid AHA, Suboh SK et al (2014) Physical properties and biocompatibility of oligochitosan membrane film as wound dressing. J Appl Biomater Funct Mater 12:155–162. https://doi.org/10.5301/jabfm.5000190
Jimenez-Kairuz A, Allemandi D, Manzo RH (2002) Mechanism of lidocaine release from carbomer-lidocaine hydrogels. J Pharm Sci 91:267–272. https://doi.org/10.1002/jps.10036
Acknowledgements
The authors acknowledge the collaborations made by Dra. Veronica Lassalle in Z-Pot determinations, Eng. Ulises Casado in DMA assays, Vanesa Fuchs in XRD measurements, and Lic. Andrés Torres Nicolini in TGA analysis.
Funding
This work was supported by the Universidad Nacional de Mar del Plata under Grant ING605/21; I + d + i Agency under Grant PICT 17- 0603, PICT 16–1905, PICT 2020–1917; and CONICET under Grant 112202101 00638CO for the fellowship to Micaela Ferrante.
Author information
Authors and Affiliations
Contributions
MF: Conceptualization, Formal analysis, data curation, investigation, methodology, writingoriginal draft, writing review; LG: Methodology, data curation, writing review; VA: Project administration, supervision, writing review; DG and EC: In vivo tests andmethodology; JG: Conceptualization, investigation, methodology, project administration, supervision, writing review.
Corresponding author
Ethics declarations
Ethical approval
All procedures involving animals were in compliance with the National Research Council's Guide for the Care and Use of Laboratory Animals. Also, the study protocols were approved by the Animal Ethics Committee of the School of Medicine at Buenos Aires University.
Competing interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferrante, M., Alvarez, V.A., Gende, L.B. et al. Polyelectrolyte complexes hydrogels based on chitosan/pectin/NaCl for potentially wound dressing: development, characterization, and evaluation. Colloid Polym Sci (2024). https://doi.org/10.1007/s00396-024-05261-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00396-024-05261-y