Abstract
Purpose
Accurate height and weight measurement can be challenging in older adults and complicates nutritional status assessment. Other parameters like the neutrophil-to-lymphocyte ratio (NLR) and the lymphocyte count (LC) could be an option to these measurements. We aimed to test these variables as subrogates of body mass index (BMI) or calf-circumference (CC) for malnutrition screening in community-dwelling older adults.
Methods
This is a secondary analysis from the Salud, Bienestar y Envejecimiento (SABE) survey from Ecuador (2009). Includes data on demographics, health-related factors, physical assessments, and complete blood count, allowing to calculate NLR and LC to be used as part of the Mini Nutritional Assessment (MNA), instead of the BMI. Consequently, 4 models were included: standard MNA, MNA-CC, MNA-NLR and MNA-LC. Finally, age, sex, and comorbidities were considered as confounding variables.
Results
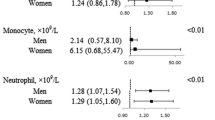
In our analysis of 1,663 subjects, 50.81% were women. Positive correlations with standard MNA were found for MNA-NLR (Estimate = 0.654, p < 0.001) MNA-CC (Estimate = 0.875, p value < 0.001) and MNA-LC (Estimate = 0.679, p < 0.001). Bland-Altman plots showed the smallest bias in MNA-CC. Linear association models revealed varying associations between MNA variants and different parameters, being MNA-NLR strongly associated with all of them (e.g. Estimate = 0.014, p = 0.001 for albumin), except BMI.
Conclusion
The newly proposed model classified a greater number of subjects at risk of malnutrition and fewer with normal nutrition compared to the standard MNA. Additionally, it demonstrated a strong correlation and concordance with the standard MNA. This suggests that hematological parameters may offer an accurate alternative and important insights into malnutrition.



Similar content being viewed by others
References
Pot AM, Rabheru K, Chew M (2023) Person-centred long-term care for older persons: a new Lancet Commission. Lancet 401(10390):1754–1755. https://doi.org/10.1016/S0140-6736(23)00920-0
Norman K, Haß U, Pirlich M (2021) Malnutrition in older adults-recent advances and remaining challenges. Nutrients 13(8). https://doi.org/10.3390/nu13082764
Cesari M, Araujo de Carvalho I, Amuthavalli Thiyagarajan J, Cooper C, Martin FC, Reginster JY et al (2018) Evidence for the domains supporting the construct of intrinsic capacity. J Gerontol Biol Sci Med Sci 73(12):1653–1660. https://doi.org/10.1093/gerona/gly011
At J, Bryce R, Prina M, Acosta D, Ferri CP, Guerra M et al (2015) Frailty and the prediction of dependence and mortality in low- and middle-income countries: a 10/66 population-based cohort study. BMC Med. ;13:138. https://doi.org/0.1186/s12916-015-0378-4
Cereda E (2012) Mini nutritional assessment. Curr Opin Clin Nutr Metab Care 15(1):29–41. https://doi.org/10.1097/MCO.0b013e32834d7647
Keller U (2019) Nutritional laboratory markers in Malnutrition. J Clin Med 8(6). https://doi.org/10.3390/jcm8060775
Tsai AC, Chang TL, Yang TW, Chang-Lee SN, Tsay SF (2010) A modified mini nutritional assessment without BMI predicts nsutritional status of community-living elderly in Taiwan. J Nutr Health Aging 14(3):183–189. https://doi.org/10.1007/s12603-010-0046-5
Faria SS, Fernandes PC Jr., Silva MJ, Lima VC, Fontes W, Freitas-Junior R et al (2016) The neutrophil-to-lymphocyte ratio: a narrative review. Ecancermedicalscience 10:702. https://doi.org/10.3332/ecancer.2016.702
Buonacera A, Stancanelli B, Colaci M, Malatino L (2022) Neutrophil to lymphocyte ratio: an emerging marker of the relationships between the Immune System and diseases. Int J Mol Sci 23(7). https://doi.org/10.3390/ijms23073636
Kaya T, Açıkgöz SB, Yıldırım M, Nalbant A, Altaş AE, Cinemre H (2019) Association between neutrophil-to-lymphocyte ratio and nutritional status in geriatric patients. J Clin Lab Anal 33(1):e22636. https://doi.org/10.1002/jcla.22636
Rojas WF, Pn EL, Fornasini M et al (2009) S T, P B, EncuestaNacional de Salud, Bienestar y Envejecimiento SABE I Ecuador. –20102010
Amano T, Gallegos CA, Waters WF, Freire WB (2021) Ethnic disparities in Nutritional Status among older adults: evidence from the Survey of Health, Welfare and Aging (SABE) Ecuador. J Gerontol Soc Work 64(2):106–119. https://doi.org/10.1080/01634372.2020.1814476
SENPLADES ECUADOR (2009) Encuesta de Salud, Bienestar y Envejecimiento
Orces CH (2015) Vitamin D status among older adults residing in the Littoral and Andes Mountains in Ecuador. Sci World J 2015:545297. https://doi.org/10.1155/2015/545297
Khosla T, Lowe CR (1967) Indices of obesity derived from body weight and height. Br J Prev Soc Med 21(3):122–128. https://doi.org/10.1136/jech.21.3.122
WHO (2006) Global database on body Mass Index: BMI classification. World Health Organization, Geneva
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S et al (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15(2):116–122. https://doi.org/10.1016/s0899-9007(98)00171-3
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9(3):179–186
Patrizio E, Calvani R, Marzetti E, Cesari M (2021) Physical Functional Assessment in older adults. J Frailty Aging 10(2):141–149. https://doi.org/10.14283/jfa.2020.61
Garcia-Cifuentes E, David-Pardo DG, Borda MG, Perez-Zepeda MU, Cano-Gutiérrez CA (2017) TWO-WAY bridge between muscular dysfunction and cognitive impairment: secondary analyses of SABE - Bogota Study. J Frailty Aging 6(3):141–143. https://doi.org/10.14283/jfa.2017.17
Altman DG (1990) Practical Statistics for Medical Research. Chapman and Hall/CRC, New York
Allard JP, Aghdassi E, McArthur M, McGeer A, Simor A, Abdolell M et al (2004) Nutrition risk factors for survival in the elderly living in Canadian long-term care facilities. J Am Geriatr Soc 52(1):59–65. https://doi.org/10.1111/j.1532-5415.2004.52011.x
Lee L-C, Tsai AC-h (2012) Mini-nutritional-assessment (MNA) without body Mass Index (BMI) predicts functional disability in elderly Taiwanese. Arch Gerontol Geriatr 54(3):e405–e10. https://doi.org/10.1016/j.archger.2011.12.006
Donini LM, Poggiogalle E, Morrone A, Scardella P, Piombo L, Neri B et al (2013) Agreement between different versions of MNA. J Nutr Health Aging 17(4):332–338. https://doi.org/10.1007/s12603-013-0005-z
Michaud M, Balardy L, Moulis G, Gaudin C, Peyrot C, Vellas B et al (2013) Proinflammatory cytokines, aging, and age-related diseases. J Am Med Dir Assoc 14(12):877–882. https://doi.org/10.1016/j.jamda.2013.05.009
Karakonstantis S, Kalemaki D, Tzagkarakis E, Lydakis C (2018) Pitfalls in studies of eosinopenia and neutrophil-to-lymphocyte count ratio. Infect Dis 50(3):163–174. https://doi.org/10.1080/23744235.2017.1388537
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A et al (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20(1):38–45
Ng TP, Nyunt MSZ, Gao Q, Wee SL, Yap P, Yap KB (2017) Elderly Nutritional indicators for Geriatric Malnutrition Assessment (ENIGMA): development and validation of a nutritional prognostic index. Clin Nutr ESPEN 22:54–63. https://doi.org/10.1016/j.clnesp.2017.08.012
Ng T-P, Hai S, Gao Q, Gwee X, Chua DQL, Yap P et al (2022) The Elderly Nutritional Index for Geriatric Malnutrition Assessment (ENIGMA): concurrent, construct and predictive validity in an external evaluation cohort of community-dwelling older persons. Br J Nutr 128(3):509–520. https://doi.org/10.1017/S0007114521003433
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397. https://doi.org/10.1016/j.jamda.2013.03.022
Gómez-Gómez ME, Zapico SC, Frailty C, Decline (2019) Neurodegenerative diseases and Nutrition interventions. Int J Mol Sci 20(11). https://doi.org/10.3390/ijms20112842
Santamaria-Garcia H, Sainz-Ballesteros A, Hernandez H, Moguilner S, Maito M, Ochoa-Rosales C et al (2023) Factors associated with healthy aging in latin American populations. Nat Med 29(9):2248–2258. https://doi.org/10.1038/s41591-023-02495-1
Albala C, Lebrão ML, León Díaz EM, Ham-Chande R, Hennis AJ, Palloni A et al (2005) [The Health, Well-Being, and aging (SABE) survey: methodology applied and profile of the study population]. Rev Panam Salud Publica 17(5–6):307–322. https://doi.org/10.1590/s1020-49892005000500003
Acknowledgements
We want to thank the people, researchers, and technical staff that made the SABE Ecuador study possible.
Funding
This paper represents independent research supported by the Norwegian government, through hospital owner Helse Vest (Western Norway Regional Health Authority). Also, funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
Author information
Authors and Affiliations
Contributions
Conceptualization: M.G.B. and S.S.L.; Methodology: M.G.B. and M.U.P.Z.; Formal analysis: J.P.B.; Writing - original draft preparation: M.G.B. and S.S.L.; Validation: M.G.B., S.S.L., P.L.S., J.P.B., L.C.V., F.J.T.S., D.A., A.M.M., M.U.P.Z.; Writing - review and editing: P.L.S., J.P.B., L.C.V., F.J.T.S., D.A., A.M.M., M.U.P.Z.; Funding acquisition: D.A.; Resources: D.A.; Supervision: D.A., A.M.M., M.U.P.Z. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study received ethical approval from the ethics and scientific committee of the Ageing Institute at Hospital Universitario San Ignacio and the Pontificia Universidad Javeriana ethics committee. SABE Ecuador was authorized by the Ecuadoran ministry of health authorities. All research procedures were conducted in accordance with the ethical standards outlined in the 1964 Declaration of Helsinki and its subsequent amendments. Measures were taken to protect the identity of the study subjects.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Borda, M.G., Salazar-Londoño, S., Lafuente-Sanchis, P. et al. Neutrophil-to-lymphocyte ratio and lymphocyte count as an alternative to body mass index for screening malnutrition in older adults living in the community. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03392-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03392-0