Abstract
Background
While folic acid (FA) is widely used to treat elevated total homocysteine (tHcy), promoting vascular health by reducing vascular oxidative stress and modulating endothelial nitric oxide synthase, the optimal daily dose and individual variation by MTHFR C677T genotypes have not been well studied. Therefore, this study aimed to explore the efficacy of eight different FA dosages on tHcy lowering in the overall sample and by MTHFR C677T genotypes.
Methods
This multicentered, randomized, double-blind, controlled clinical trial included 2697 eligible hypertensive adults with elevated tHcy (≥ 10 mmol/L) and without history of stroke and cardiovascular disease. Participants were randomized into eight dose groups of FA combined with 10 mg enalapril maleate, taken daily for 8 weeks of treatment.
Results
The intent to treat analysis included 2163 participants. In the overall sample, increasing FA dosage led to steady tHcy reduction within the FA dosing range of 0–1.2 mg. However, a plateau in tHcy lowering was observed in FA dose range of 1.2–1.6 mg, indicating a ceiling effect. In contrast, FA doses were positively and linearly associated with serum folate levels without signs of plateau. Among MTHFR genotype subgroups, participants with the TT genotype showed greater efficacy of FA in tHcy lowering.
Conclusions
This randomized trial lent further support to the efficacy of FA in lowering tHcy; more importantly, it provided critically needed evidence to inform optimal FA dosage. We found that the efficacy of FA in lowering tHcy reaches a plateau if the daily dosage exceeds 1.2 mg, and only has a small gain by increasing the dosage from 0.8 to 1.2 mg.
ClinicalTrials.gov Identifier
NCT03472508 (Registration Date: March 21, 2018).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Folate, a water-soluble vitamin, includes endogenous food folate and its synthetic form, folic acid (FA) [1]. Previous studies have demonstrated the effectiveness of FA supplementation in preventing neural-tube defects (NTD) in newborns. Since 1996, nations such as the USA and Canada have introduced mandatory FA fortification of white flour [2]. Such regulations are currently widely in place in 53 countries worldwide [3]. However, despite the knowledge that FA supplementation reduces the risk of NTD such as spina bifida during the periconceptional period [4, 5], its efficacy on cardiovascular and cerebrovascular disease prevention remains controversial. A meta-analysis we conducted earlier using randomized trial data showed that in countries without FA fortification, FA supplementation considerably lowers the risk of stroke, whereas it presents limited benefit in fortified countries [6]. Furthermore, folic acid therapy in low doses, alike daily intake, and dietary fortification, can enhance vascular function by reducing vascular oxidative stress and modulating nitric oxide synthase [7]. Baseline folate differs by various factors such as fortification regulations and is particularly associated with homocysteine level [8].
Recent studies have determined elevated plasma total homocysteine (tHcy) level to be well-established modifiable risk factors for cerebral–cardiovascular disease [9,10,11]. Elevation of circulating tHcy concentrations is also closely related with numerous nutritional, hormonal, and genetic factors, and thus is associated with particular pathological conditions. Given that the majority of the body’s tHcy participates in the re-methylation process through one-carbon metabolism, which requires a folate-derived methyl donor, folic acid therapy has been proposed as a key strategy for lowering tHcy levels.
The primary carbon donor in the re-methylation of tHcy to methionine is 5-methyltetrahydrofolate, which is synthesized by methylenetetrahydrofolate reductase (MTHFR). However, a prevalent MTHFR mutation that replaces alanine with valine can render the enzyme thermolabile and results in increased plasma levels of tHcy. Those with thermolabile MTHFR may require a greater amount of folate to regulate plasma tHcy concentrations [12, 13]. The most compelling evidence supporting the effectiveness of reducing tHcy levels in preventing risk is observed in the China Stroke Primary Prevention Trial (CSPPT), which indicates that a 20% reduction in tHcy led to 7% decrease in the risk of incident stroke and composite cardiovascular disease [14]. Additionally, a subset of the CSPPT showed that the MTHFR C677T genotype modified the FA therapeutic effect [15]. With aligned long-term 0.8 mg/day FA therapy, about 30% of individuals with the TT genotype did not reach the folate threshold of ≥ 15 ng/mL, and only about 20% from the TT group achieved a tHcy level below10 μmol/L at the exit visit.
The Chinese population without mandatory FA fortification has a high proportion of insufficient folate intake (> 50%), hyperhomocysteinemia, and the MTHFR gene polymorphism [16, 17]. In particular, Chinese patients with hypertension accompanied by elevated tHcy (≥ 10 μmol/L) have a synergistically increased risk of stroke [18, 19]. Thus, stroke prevention strategies that target the lowering of tHcy levels in hypertensive patients are essentially needed. In addition, a post-mortem analysis by the CSPPT showed that in people with low levels of folic acid, a daily intake of 0.8 mg of folic acid was associated with a lower risk of malignant tumors associated with stress [20]. However, to date, there is a general lack of consensus on the optimal folic acid supplementation dosage, and the recommended supplementation strategies vary among different countries [21].
An urgent need for further investigation on folic acid therapy strategies, as well as the optimal FA dose required in tHcy lowering among the various MTHFR genotypes. Thus, the following folic acid dose titration study, the Precision Folic Acid Trial to lower homocysteine (PFAT-Hcy, ClinicalTrials.gov Identifier: NCT03472508), was designed. This is by far the first and largest folic acid intervention trial in Chinese adults with hypertension and elevated tHcy, a population exposed to higher stroke and cardiovascular disease risks. This paper lays down the essential background and conclusions for future research, which will provide high-quality evidence to inform clinical and public health guidelines on the optimal dose of folic acid for tHcy lowering, while considering individual MTHFR genotype.
Materials and methods
Study oversight
PFAT-Hcy is a multi-centered, randomized, double-blind, controlled clinical trial, conducted at Wuyuan, Anqing, and Lianyungang, China. The details of the protocol have been published elsewhere [22]. Briefly, inclusion criteria included men and women aged 45–75 years with hypertension, defined as resting seated systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg and/or taking antihypertensive medication, and elevated tHcy (≥ 10 μmol/L) during both the screening and recruitment visits conducted at least 1 day apart. Persons with a history of cardiovascular diseases were excluded, as were persons with any chronic disease that might interfere with folate or homocysteine metabolism (e.g., renal disease, thyroid disease, liver disease). Anyone taking dietary supplements containing B vitamins or compounds within 3 months of study initiation were excluded. Eligible patients were randomly assigned to one of eight doses of FA daily treatment group from 0 to 2.4 mg (0, 0.4, 0.6, 0.8, 1.2, 1.6, 2.0, 2.4 mg). The trial was conducted between August 2017 and October 2018. The primary end point was tHcy lowering. Follow-up visits were completed at the end of the 2nd, 4th, 6th, and 8th week of treatment.
Ethics approval
This study was approved by the Medical Ethics Committee of the Second Affiliated Hospital of Nanchang University’s Local Ethical Review process (2018–02–2). Written informed consents were provided by all study participants.
Physical examination, demographic characteristics, and laboratory assays
During the first screening visit, which priors the treatment visit, physical examination was conducted to assess patients’ clinical diagnosis and eligibility for inclusion in the study. Other demographic information and information related to this study’s inclusion/exclusion criteria were also obtained.
Fasting (overnight) venous blood samples (8 mL each) and spot urine samples (10 mL) were collected at baseline and at the end of the 4th and 8th week after the double-blind treatment began. The TaqMan assay was used to detect the MTHFR C677T (rs1801133) polymorphisms using the ABI Prism 7900HT sequence detection system (Life Technologies). Serum folate, vitamin B12, and B6 were measured using a chemiluminescent immunoassay (New Industrial) at a commercial laboratory at both the baseline and exit visit during the run-in period and the double-blind treatment period. Serum fasting lipids and glucose, creatinine, and tHcy were measured using automatic clinical analyzers (Beckman Coulter) at the central laboratory of the Shenzhen Tailored Medical Laboratory at both the baseline and exit visit [23, 24]. While they were not analyzed in this study, these laboratory results will be used in future statistical analyses and in the final report. In addition, serum 5-methyltetrahydrofolate (5-MeTHF), unmetabolized folic acid, S-adenosinemethionine (SAM), and S-adenosinehomocysteine (SAH) were measured for future further analysis.
Efficacy indicator
The primary efficacy indicator was the percentage decrease in blood tHcy levels by the end of the 8th week from baseline [tHcy percent decrease = (baseline tHcy-end tHcy)/baseline tHcy*100%]. Secondary efficacy indicators include the magnitude of decrease in tHcy by the end of the 8th week from baseline [absolute tHcy reduction (mmol/L) = baseline tHcy-end tHcy] and percentage and magnitude of increase in blood folate levels by the end of the 8th week from baseline.
Statistical analysis
Based on a previous study, tHcy lowering rate for enalapril folic acid tablet 10/0.8 mg was anticipated to be 11–12%, whereas the control group (enalapril) almost stayed the same [15]. To achieve 80% power while maintaining a type I error rate of 0.00625 for pairwise comparisons among eight groups with Bonferroni correction (0.05/8 = 0.00625), a minimum of 165 participants per group would be required. Further considering potential cases of withdrawal, shedding, and low compliance (10–20%), the total sample size for this study was 1600 cases with 200 participants per group. Based on all dose groups, 0.8 mg is the intermediate dose group, and the calculated sample size can meet the research hypothesis. This trial, with a sample size of 2163 eligible participants in the final analysis, was adequately powered to address the primary study hypothesis.
Means (SD) and proportions were calculated for the population characteristics by FA dosage. Curve fitting by nonlinear regression was used to assess the adequate folic acid dose: mean relative changes in plasma tHcy concentration were plotted by dose of folic acid, and nonlinear regression was used to find the best-fit curve through the relative decreases in tHcy concentrations. In the exploratory analyses, a possible interaction with the MTHFR C677T genotype on the efficacy of folic acid and tHcy lowering was investigated. R software, version 2.15.1 (http://www.R-project.org/), was used for all statistical analyses.
Results
Baseline characteristics
A total of 2697 eligible participants were randomized to eight dosages of daily folate treatment groups. After excluding those with missing tHcy and/or folate data at either baseline or the exit visit (n = 534), 2163 eligible participants were included in the final analysis (Fig. 1). The baseline characteristics of the total population and by FA dosages are presented in Table 1, of which 45.4% were males (n = 981), mean age was 64.9 (SD 8.3) years, mean baseline tHcy level was 14.1 (11.9–17.5) µmol/L, and mean folate was 10.6 (7.2–15.3) ng/mL. These baseline characteristics indicate that a successful randomization within different treatment groups was carried out (Table 1).
Percentage and absolute change of tHcy level reduction
Table 2 presents the absolute change value and percentage change of tHcy levels from baseline to the exit visit in the total population and in each FA treatment group stratified by MTHFR C677T genotypes. In the total population, with increasing doses of folate supplementation ranging from 0 to 2.4 mg, tHcy levels presented an overall decreasing association from 1.8 µmol/L in absolute change in tHcy levels for the 0.4 mg FA treatment group to 3.0 µmol/L in absolute change for the 2.4 FA treatment group. However, the greatest percentage of tHcy lowering was observed between the FA treatment groups 0.4–0.8 mg (change rate in tHcy: 7.4–9.9%) and in the 2.4 mg FA treatment group (change rate in tHcy: 11.2%).
When stratified by the MTHFR C677T genotypes CC, CT, and TT, an essentially higher tHcy-lowering effect was found in participants with the TT genotype and baseline tHcy > 15 μmol/L. With the increasing doses of folate supplementation from 0 to 2.4 mg, tHcy levels presented an overall decreasing association in all three genotype groups. The CC group showed the greatest fluctuations in the tHcy levels between the FA treatment doses of 1.2–1.6 mg, in the CT group between the FA doses 1.6–2.0 mg, and in the TT group between the FA doses 1.2–2.0 mg. The greatest tHcy-lowering rate was observed in the CC group at FA treatment 0.8 mg/day (tHcy lowering: 10.1%), in the CT group at 1.2 mg/day (tHcy lowering: 11.8%), and in the TT group at 2.4 mg/day (tHcy lowering: 20.2%).
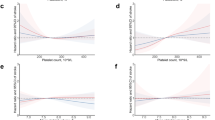
Figure 2 illustrates the fitted smoothing curves of tHcy change rate/absolute value with doses of folate therapy in the total population (A and C) and stratified by the MTHFR genotypes (B and D) after 8 weeks of intervention after adjusting for sex, age, BMI, smoking status, systolic blood pressure (SBP), center, fasting blood glucose (FBG), high-density lipoprotein cholesterol (HDL-C), estimated glomerular filtration rate (eGFR), MTHFR, and folate levels. Changes/plateaus can be roughly observed between folic acid doses 1.2–1.6 mg/day in the total population.
Adjusted fitted smoothing curves of serum total homocysteine (A–D) and folate (E, F) change and change rate for different doses of folic acid intervention at 8 weeks. A and B groups represent the change rate of total homocysteine in the overall population and subgroups stratified by MTHFR genotypes, respectively, across different doses of folic acid intervention at 8 weeks. C and D groups represent the absolute change of total homocysteine in the overall population and subgroups stratified by MTHFR genotypes, respectively. E and F groups represent the change of folate levels in the overall population and subgroups stratified by MTHFR genotypes, respectively, with varying folic acid dosage. Adjusted for age, sex, body mass index, systolic blood pressure, smoking status, center, high-density lipoprotein cholesterol, fasting blood glucose, MTHFR C677T, estimated glomerular filtration rate, and baseline folate level. Homocysteine and folate changes were defined as baseline − exit. Change rate were defined as (baseline − exit)/baseline)
Supplemental Tables 1 and 2 present the effects of different doses of folic acid treatment on tHcy change rates (Supplemental Table 1) and change values (Supplemental Table 2) in the total population and stratified by the MTHFR C677T genotype. In both tables, linear and quadratic associations between different doses of folic acid treatment with tHcy change rate and change in the total population were found to be significant after adjusting for covariates. The quadratic association presented a β value of − 4.48 (0.93)/− 0.62(0.24) for change rate and change, respectively, in the total population. The P value for joint effect (df = 2) was found to be significant (< 0.001). Similar results were identified in the MTHFR C677T stratified groups, with significant and negative β values in both the linear and quadratic associations between different doses of folic acid treatment with change rate/change value in tHcy levels.
Changes in serum folate levels
Table 3 presents the change in serum folate levels from baseline to the exit visit for each treatment group in the total population and stratified by the MTHFR C677T genotypes. Both the total population and the genotype subgroups showed a dose-dependent increase in folic acid levels. Figure 2 shows the fitted smoothing curves of folate change with dose of folic acid in the total population (E) and stratified by the MTHFR C677T genotypes (F). These results are in accordance with the results in Table 3, showing that increases in folate change value is associated with a higher dose of folic acid treatment.
Adverse events
The frequencies of reported adverse events, according to the Medical Dictionary for Regulatory Activities Primary System Organ Classification (SOC), and drug-related adverse events were not significantly different among the total sample (Table 4) or the subgroups stratified by the MTHFR C677T genotypes (Supplemental Tables 3–5). Furthermore, no statistical differences were found between the treatment groups with regard to other safety outcomes, such as adverse events leading to drug withdrawal, abnormal laboratory test results with clinical significance, and any serious adverse events.
Sensitivity analysis
Supplemental Fig. 1 illustrates the fitted smoothing curves of tHcy change rate/absolute value with dose of folate therapy stratified by males and females (A and B) after 8 weeks of intervention with adjustment for age, sex, BMI, SBP, smoking status, center, HDL-C, FBG, MTHFR, eGFR, and folate levels. Changes/plateaus were roughly observed between folic acid doses 1.2–1.6 mg/day regardless of sex.
Supplemental Fig. 2 presents the adjusted smoothing curves of tHcy change (C and D) and the tHcy change rate (A and B) with doses of folic acid treatment in the total population (A and C), and for the MTHFR genotype stratified groups (B and D) with data from patients who had > 80% compliance (n = 1752). The results appear similar to the aforementioned results in Fig. 2.
Discussion
This study investigated the interactive effect of the MTHFR C677T gene variant and serum folate levels on the tHcy-lowering response to short-term, varying doses of FA supplementation, in a population without mandatory FA fortification. To the best of our knowledge, this study is the first randomized, double-blinded trial to test the feasibility and effectiveness of different doses of FA supplementation for lowering tHcy and metabolites in the FA–tHcy metabolic pathway and the genetic interaction of the MTHFR C677T genotype in Chinese patients. This study found that after 8 weeks of folic acid supplementation, tHcy decreased by 9.2% in general. Combined with the results of CSPPT, which contains a similar population and found that 0.8 mg daily FA treatment increased folate levels and led to an average of tHcy levels reduction of 11%, these studies confirmed the stability of the current population.
This study explored a stable dose–effect relationship between 0 and 1.2 mg/day FA therapy on tHcy lowering. However, further increases in folate dose brought about a plateau. Wald et al. reported that serum tHcy levels decreased with increasing folic acid dosage and reached maximum efficacy at a dosage of 0.8 mg/day FA supplementation with a 23% reduction in tHcy among a population in Great Britain with ischemic heart disease [25]. A meta-analysis showed that a 1 mg/day folic acid dose generated the most tHcy-lowering efficacy, with no further reduction in tHcy levels with increasing dosages [21]. FA treatment ranging from 0.5 to 5.0 mg lowered tHcy levels by 25%. Studies that demonstrated promising results with reductions in tHcy levels have shown that the efficacy is more prominent among patients with high baseline tHcy levels or low folate levels before treatment [21]. A daily dose of approximately 400 μg is the minimum dose required for adequate tHcy reduction [26]. A 2010 study found that folic acid supplementation (0, 100, 400, 1000, or 2000 μg/day) had no dose–response relationship between FA and tHcy concentrations, but the data indicated that healthy, older adults (aged 60–90 years) can improve their folate status through supplementation [27].
This study found that the interaction between folic acid supplementation and tHcy exhibited distinct patterns for different MTHFR C677T genotypes among this population of Chinese hypertensive adults, along with different folic acid and tHcy levels at baseline across groups. In the TT group, lower doses of folic acid therapy (0.4–0.8 mg/day) were associated with maximum tHcy-lowering efficacy. The TT group had a steeper slope compared with the CC/CT group, and the fitted curve did not reach a plateau until 1.6 mg/day of folic acid supplement. The more effective tHcy-lowering capacity of folic acid therapy in the TT group can be explained by the fact that the highest baseline tHcy levels and the lowest folic acid levels were found in the TT group compared with the CC/CT group. The fitted curves for the correlation between folic acid treatment dose and changes in tHcy levels in different MTHFR C677T genotypes intersected at 1.0 mg/day of folic acid dose. In the CT group, the fitted curve reached a plateau at 1.0–1.2 mg/day of folic acid supplementation, and increased dose was found to be associated with a poorer tHcy reduction response. In the CC group, the fitted curve reached a plateau between 1.2 and 1.6 mg/day of folic acid supplement. The variability of tHcy reduction with folic acid treatment is in accordance with the results of the CSPPT, which determined an effect modification among the MTHFR genotypes in the efficacy of FA treatment. A post hoc analysis of the CSPPT found a more pronounced L-shaped curve between tHcy and serum folate levels in participants with the TT genotype compared with those with the CC and CT genotypes, requiring a higher folate level (at least 15 ng/mL) to eliminate genotypic tHcy differences. Our study results contribute to determining optimal folic acid intervention strategies in stroke risk prevention for hypertensive patients, especially in China where the effect of tHcy on first stroke is significantly modified by the methylenetetrahydrofolate reductase C677T genotype.
Our findings suggest a dose-dependent relationship between folate levels and folic acid supplementation. With increasing doses of folic acid supplementation, folate levels were elevated with no observed plateau, while the decreases in tHcy levels showed a significant plateau. The underlying mechanism can be explained by the differences in physical and chemical properties of synthetic folic acid. Folates are water-soluble vitamins that provide one-carbon units for the regulation of gene expression, nucleotide synthesis, and production of amino acids and neurotransmitters [28]. Available forms of synthetic folic acid include FA, folinic acid (formyl tetrahydrofolate), and 5-methyltetrahydrofolate (5-MTHFR). Folic acid from fortified foods and supplements differs from folate from natural sources, in that it requires dihydrofolate reductase (DHFR) for conversion to tetrahydrofolate to be active in one-carbon metabolism [29]. In areas that have FA fortification or synthetic FA recommendation [30, 31], circulating unmetabolized FA (UMFA) and 5-methyl-THF accounts for about 4% and 85% of total folate, respectively [32].
In a large national study with randomly selected US adults, both low and high serum total folates (total folate, UMFA, non-methyl folate, 5-mTHF, and MeFox [pyrazino-s-triazine derivative of 4ahydroxy-5-methyltetrahydrofolate]) were associated with a higher risk of all-cause, cardiovascular disease (CVD), and cause-specific mortality, including 5-mTHF insufficiency [33]. A study of major depressive disorder found that L-5-MeTHF improved symptoms in treatment-resistant major depressive disorder [34]. The MIREC (Maternal–Infant Research on Environmental Chemicals) study observed that the consumption of FA supplements by women resulted in a significantly increased total folate in breast milk. However, the increase in total milk folate was attributed to higher UMFA concentration, but not to reduced folates [35]. The higher proportion of UMFA in breast milk compared to 5-methylTHF in women consuming 400 μg FA daily suggests that higher doses exceed the physiological capacity to metabolize FA, resulting in preferential absorption of FA in breast milk. Our study population was characterized by low baseline levels of folate and with no FA fortification. The presence of a plateau in tHcy lowering within the range of 0.8–1.2 mg/day dose of folic acid therapy and the constant increase in folate levels for all doses indicate that caution should be taken for the use of higher folic acid doses for general population supplementation.
Folic acid therapy is frequently simultaneously considered with other B vitamins in metabolic cycles. The interpretation of clinical trial results for vitamin therapy to reduce tHcy levels is heavily reliant on folate levels, B12 status, and renal function [36, 37]. Most previous studies have adopted multiple vitamin B supplements with folate as the main component, for it has been shown that folate contributes the most to tHcy lowering, and additional supplements of B12 and B6 can lower tHcy levels by 7% [38].
No sex differences on the association between folic acid therapy and tHcy changes were observed in this study. A sensitivity analysis in the population with > 80% adherence showed the same patterns as the main study result.
Even in countries where fortified folic acid supplementation policies exist, most people still rely on food supplements, and a smaller proportion is aware of or adheres to the recommended daily intake levels [39]. Variation have been noted between countries in terms of the utilization, awareness, and beliefs toward FA supplement policies. Our study results highlighted the importance of evaluating and monitoring the utilization of supplements during antenatal care to facilitate appropriate usage. However, a systematic review demonstrated that in countries with mandatory food fortification policies, women who take FA supplements may surpass the upper tolerable limit of FA [40]. A recent study also found that excessive folic acid intake in parental mice increased DNA mutations and epigenetic changes in offspring embryos [41]. The problems of folic acid dosage, form, suitable population, and duration of supplementation have been plagued and are still ongoing.
Mammals, with the absence of folate biosynthesis, primarily meet their folate requirements through the diet. Historically, folate deficiency caused by poor nutrition has been one of the most widespread vitamin deficiencies and has persisted in countries that do not have mandatory FA fortification [42]. Future studies are critically needed to determine the optimal approaches in various pathological conditions. This study showed a precise dosage recommendation for a rural Chinese population with H-type hypertension, depending on the MTHFR C677T genotype.
This RCT has some limitations. The sample size was modest, although adequate power was expected based on the power estimation, for addressing the primary and secondary outcomes. This trial had only 8 weeks of treatment and follow-up. Although this duration is adequate for our primary and secondary outcomes, we were unable to evaluate long-term outcomes such as stroke incidence. The current analysis does not specifically confirm the proportion of people who might have actually met the target tHcy level window. Efforts are needed to try to increase the proportion of the whole population meeting the standards. To achieve a higher proportion of people with reduced levels, future analysis and research are required.
Conclusion
In this population of rural Chinese adults with H-type hypertension, the optimal tHcy change rate corresponded to a folic acid dose range of 0–1.2 mg. A higher dose of FA had no effect on further lowering tHcy in the total population, with the exception of participants with the TT genotype. Further research is urgently needed to establish a safe and cost-effective FA regimen that is tailored to individual genetic profiles and folate nutritional status, to address stroke and CVD, which are major clinical and public health problems in China and many other developing countries.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- FA:
-
Folic acid
- NTD:
-
Neural-tube defects
- tHcy:
-
Total homocysteine
- MTHFR :
-
Methylenetetrahydrofolate reductase
- 5-MeTHF:
-
5-Methyltetrahydrofolate
- BMI:
-
Body mass index
- SBP:
-
Systolic blood pressure
- HDL-C:
-
High-density lipoprotein cholesterol
- FBG:
-
Fasting blood glucose
- eGFR:
-
Estimated glomerular filtration rate
- UMFA:
-
Unmetabolized folic acid
- CVD:
-
Cardiovascular disease
References
Menon S, Nasir B, Avgan N et al (2016) The effect of 1 mg folic acid supplementation on clinical outcomes in female migraine with aura patients. J Headache Pain 17:60
Jacques PF, Selhub J, Bostom AG et al (1999) The effect of folic acid fortification on plasma folate and total homocysteine concentrations. N Engl J Med 340:1449–1454
Centers for Disease C, Prevention (2010) CDC Grand Rounds: additional opportunities to prevent neural tube defects with folic acid fortification. MMWR Morb Mortal Wkly Rep 59:980–984
Czeizel AE, Dudás I (1992) Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 327:1832–1835
Crider KS, Bailey LB, Berry RJ (2011) Folic acid food fortification-its history, effect, concerns, and future directions. Nutrients 3:370–384
Wang X, Qin X, Demirtas H et al (2007) Efficacy of folic acid supplementation in stroke prevention: a meta-analysis. Lancet 369:1876–1882
Shirodaria C, Antoniades C, Lee J et al (2007) Global improvement of vascular function and redox state with low-dose folic acid: implications for folate therapy in patients with coronary artery disease. Circulation 115:2262–2270
Boushey CJ, Beresford SA, Omenn GS et al (1995) A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. probable benefits of increasing folic acid intakes. JAMA 274:1049–1057
Ganguly P, Alam SF (2015) Role of homocysteine in the development of cardiovascular disease. Nutr J 14:6
Graham IM, Daly LE, Refsum HM et al (1997) Plasma homocysteine as a risk factor for vascular disease. The European Concerted Action Project. JAMA 277:1775–1781
Zhang ZY, Gu X, Tang Z et al (2021) Homocysteine, hypertension, and risks of cardiovascular events and all-cause death in the Chinese elderly population: a prospective study. J Geriatr Cardiol 18:796–808
Frosst P, Blom HJ, Milos R et al (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10:111–113
Jacques PF, Bostom AG, Williams RR et al (1996) Relation between folate status, a common mutation in methylenetetrahydrofolate reductase, and plasma homocysteine concentrations. Circulation 93:7–9
Huang X, Li Y, Li P et al (2017) Association between percent decline in serum total homocysteine and risk of first stroke. Neurology 89:2101–2107
Huang X, Qin X, Yang W et al (2018) MTHFR gene and serum folate interaction on serum homocysteine lowering: prospect for precision folic acid treatment. Arterioscler Thromb Vasc Biol 38:679–685
Qin X, Li J, Cui Y et al (2012) MTHFR C677T and MTR A2756G polymorphisms and the homocysteine lowering efficacy of different doses of folic acid in hypertensive Chinese adults. Nutr J 11:2
Bao H, Huang X, Li P et al (2023) Combined use of amlodipine and folic acid are significantly more efficacious than amlodipine alone in lowering plasma homocysteine and blood pressure among hypertensive patients with hyperhomocysteinemia and intolerance to ACEI: a multicenter, randomized, double-blind, parallel-controlled clinical trial. J Clin Hypertens (Greenwich) 25:689–699
Jiang S, Li J, Zhang Y et al (2017) Methylenetetrahydrofolate reductase C677T polymorphism, hypertension and risk of stroke: a prospective, nested case-control study. Int J Neurosci 127:253–260
Ortel TL, Neumann I, Ageno W et al (2020) American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 4:4693–4738
Li H, He P, Zhang Y et al (2022) Self-perceived psychological stress, baseline folate levels, folic acid treatment, and incident risk of cancer: secondary analysis of CSPPT. Precis Nutr. https://doi.org/10.1097/PN1099.0000000000000006
Collaboration HLT (1998) Lowering blood homocysteine with folic acid based supplements: meta-analysis of randomised trials. Homocysteine Lowering Trialists’ Collaboration. BMJ 316:894–898
Bao H, Huang X, Liu L et al (2022) A randomized, double-blind, controlled trial on the homocysteine-lowering effects of different doses of folic acid among patients with hypertension and elevated homocysteine according to methylenetetrahydrofolate reductase C677T genotypes: rationale and methods. Precis Nutr. https://doi.org/10.1097/PN9.0000000000000004
Chen P, Tang L, Song Y et al (2023) Association of folic acid dosage with circulating unmetabolized folic acid in Chinese adults with H-type hypertension: a multicenter, double-blind, randomized controlled trial. Front Nutr 10:1191610
Huo Y, Li J, Qin X et al (2015) Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA 313:1325–1335
Wald DS, Bishop L, Wald NJ et al (2001) Randomized trial of folic acid supplementation and serum homocysteine levels. Arch Intern Med 161:695–700
van Oort FV, Melse-Boonstra A, Brouwer IA et al (2003) Folic acid and reduction of plasma homocysteine concentrations in older adults: a dose-response study. Am J Clin Nutr 77:1318–1323
Anderson CA, Jee SH, Charleston J et al (2010) Effects of folic acid supplementation on serum folate and plasma homocysteine concentrations in older adults: a dose-response trial. Am J Epidemiol 172:932–941
Tibbetts AS, Appling DR (2010) Compartmentalization of Mammalian folate-mediated one-carbon metabolism. Annu Rev Nutr 30:57–81
Plumptre L, Masih SP, Ly A et al (2015) High concentrations of folate and unmetabolized folic acid in a cohort of pregnant Canadian women and umbilical cord blood. Am J Clin Nutr 102:848–857
Kelly P, McPartlin J, Goggins M et al (1997) Unmetabolized folic acid in serum: acute studies in subjects consuming fortified food and supplements. Am J Clin Nutr 65:1790–1795
Pfeiffer CM, Sternberg MR, Fazili Z et al (2015) Unmetabolized folic acid is detected in nearly all serum samples from US children, adolescents, and adults. J Nutr 145:520–531
Fazili Z, Pfeiffer CM, Zhang M (2007) Comparison of serum folate species analyzed by LC-MS/MS with total folate measured by microbiologic assay and Bio-Rad radioassay. Clin Chem 53:781–784
Liu M, Zhang Z, Zhou C et al (2021) Relationship of several serum folate forms with the risk of mortality: a prospective cohort study. Clin Nutr 40:4255–4262
Jain R, Manning S, Cutler AJ (2020) Good, better, best: clinical scenarios for the use of L-methylfolate in patients with MDD. CNS Spectr 25:750–764
Page R, Robichaud A, Arbuckle TE et al (2017) Total folate and unmetabolized folic acid in the breast milk of a cross-section of Canadian women. Am J Clin Nutr 105:1101–1109
Spence JD (2016) Metabolic vitamin B12 deficiency: a missed opportunity to prevent dementia and stroke. Nutr Res 36:109–116
Spence JD, Stampfer MJ (2011) Understanding the complexity of homocysteine lowering with vitamins: the potential role of subgroup analyses. JAMA 306:2610–2611
Lonn E, Yusuf S, Arnold MJ et al (2006) Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med 354:1567–1577
Yang Q, Cogswell ME, Hamner HC et al (2010) Folic acid source, usual intake, and folate and vitamin B-12 status in US adults: National Health and Nutrition Examination Survey (NHANES) 2003–2006. Am J Clin Nutr 91:64–72
Ledowsky C, Mahimbo A, Scarf V et al (2022) Women taking a folic acid supplement in countries with mandatory food fortification programs may be exceeding the upper tolerable limit of folic acid: a systematic review. Nutrients 14:2715
Cao X, Xu J, Lin YL et al (2023) Excess folic acid intake increases DNA de novo point mutations. Cell Discov 9:22
Bailey RL, West KP Jr, Black RE (2015) The epidemiology of global micronutrient deficiencies. Ann Nutr Metab 66(Suppl 2):22–33
Acknowledgements
We thank all the study participants in this study.
Funding
The study was supported by funding from the following: the National Natural Science Foundation of China (81960074); Key R&D Projects, Jiangxi (20203BBGL73173); Key R&D Plan-Key Projects (20212BBG71012); the Jiangxi Provincial Health Commission (202130440); and the Jiangxi Science and Technology Innovation Platform Project (20165BCD41005).
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: XC, YH, XW, XH, and HB; methodology: XC, YH, XW, XH, and HB; formal analysis: XH, HB, LL, JL, CD, TC, YS, YW, and ZZ; investigation: HB, XH, LL; JL, CD, YS, ZZ, CJ, LX, XQ, BW, NZ, PC, YZ, and JL; writing—original draft: XH, CD, and TC; writing—review and editing: HW, XW, NS, and XC; supervision: YH, HW, XW, and XC; project administration: XC, YH, and GT; funding acquisition: XC and XH. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Xiao Huang reports grants from the National Natural Science Foundation of China (81960074); Key R&D Projects, Jiangxi (20203BBGL73173); Key R&D Plan-Key Projects (20212BBG71012); and the Jiangxi Provincial Health Commission (202130440). Dr. Xiaoshu Cheng reports grant from the Jiangxi Science and Technology Innovation Platform Project (20165BCD41005). All other authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, X., Bao, H., Ding, C. et al. Optimal folic acid dosage in lowering homocysteine: Precision Folic Acid Trial to lower homocysteine (PFAT-Hcy). Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03344-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03344-8