Abstract
Purpose
The aim of this systematic review with meta-analysis was to determine whether anthocyanin-rich foods are effective to improve cardiometabolic markers in individuals with metabolic syndrome (MetS), compared with placebo or control interventions.
Methods
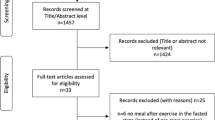
We searched MEDLINE, CENTRAL, Embase, LILACS, CINAHL, and Web of Science from their inception up to March 2022. We include clinical trials (randomized clinical trials, controlled clinical trials, and cross-over trials) with anthocyanin-rich foods versus placebo or control intervention that assessment cardiometabolic factors.
Results
We found 14 clinical trials that met the eligibility criteria, and we included 10 studies for the quantitative synthesis. For anthocyanin-rich foods versus control interventions, the mean difference (MD) for low-density lipoprotein (LDL) was − 7.98 mg/dL (CI = − 15.20 to − 0.77, GRADE: Very low). For homeostatic model assessment for insulin resistance (HOMA-IR), the MD was 0.04 (CI = 0.08 to 0.16, GRADE: Moderate). The MD for interleukin 6 was 0.00 pg/mL (CI = − 0.01 to 0.00, GRADE: Low). For tumor necrosis factor alpha (TNF-α), the standardized mean difference (SMD) was − 0.52 pg/mL (CI = 0.85 to 0.19 GRADE: Very low) when compared with the control interventions. The certainty of the evidence for the other outcomes it is very low.
Conclusion
Our findings suggest that anthocyanin-rich foods could improve certain cardiometabolic markers (e.g., TC, TG, LDL, and TNF-α) among individuals with MetS (with very low quality evidence according to GRADE), compared with placebo or other control interventions.
PROSPERO registration number
CRD42020187287.








Similar content being viewed by others
Data availability
Raw data that support the fndings of this study can be provided by the corresponding author upon reasonable request.
References
Kaur J (2014) A comprehensive review on metabolic syndrome. Cardiol Res Pract 2014:943162. https://doi.org/10.1155/2014/943162
Samson SL, Garber AJ (2014) Metabolic syndrome. Endocrinol Metab Clin North Am 43(1):1–23. https://doi.org/10.1016/j.ecl.2013.09.009
Nolan PB, Carrick-Ranson G, Stinear JW, Reading SA, Dalleck LC (2017) Prevalence of metabolic syndrome and metabolic syn-drome components in young adults: a pooled analysis. Prev Med Rep 19(7):211–215. https://doi.org/10.1016/j.pmedr.2017.07.004
Saklayen MG (2018) The global epidemic of the metabolic syndrome. Curr Hypertens Rep 20(2):12. https://doi.org/10.1007/s11906-018-0812-z
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, Rinfret S, Schiffrin EL, Eisenberg MJ (2010) The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol 56(14):1113–1132. https://doi.org/10.1016/j.jacc.2010.05.034
Grundy SM (2016) Metabolic syndrome update. Trends Cardiovasc Med 26:364–373. https://doi.org/10.1016/j.tcm.2015.10.004
Hulsmans M, Holvoet P (2010) The vicious circle between oxidative stress and inflammation in atherosclerosis. J Cell Mol Med 14:70–78. https://doi.org/10.1111/j.1582-4934.2009.00978.x
Xia X, Weng J (2010) Targeting metabolic syndrome: candidate natural agents. J Diabetes 2(4):243–249. https://doi.org/10.1111/j.1753-0407.2010.00090.x
Grundy S (2009) Advancing drug therapy of the metabolic syndrome. Nat Rev Drug Discov 8:341. https://doi.org/10.1038/nrd2894
Wallace TC, Giusti MM (2015) Anthocyanins. Adv Nutr 6(5):620–622. https://doi.org/10.3945/an.115.009233
Wallace TC, Slavin M, Frankenfeld CL (2016) Systematic review of anthocyanins and markers of cardiovascular disease. Nutrients 8(1):32. https://doi.org/10.3390/nu8010032
Kolehmainen M, Mykkänen O, Kirjavainen PV, Leppänen T, Moilanen E, Adriaens M et al (2012) Bilberries reduce low-grade inflammation in individuals with features of metabolic syndrome. Mol Nutr Food Res 56(10):1501–1510. https://doi.org/10.1002/mnfr.201200195
De Ferrars RM, Czank C, Zhang Q, Botting NP, Kroon PA, Cassidy A, Kay CD (2014) The pharmacokinetics of anthocya-nins and their metabolites in humans. Br J Pharmacol 171:3268–3282. https://doi.org/10.1111/bph.12676
Vendrame S, Klimis-Zacas D (2019) Potential factors influencing the effects of anthocyanins on blood pressure regulation in humans: a review. Nutrients 11(6):1431. https://doi.org/10.3390/nu11061431
Ahles S, Joris PJ, Plat J (2021) Effects of berry anthocyanins on cognitive performance, vascular function and cardiometabolic risk markers: a systematic review of randomized placebo-controlled intervention studies in humans. Int J Mol Sci 22(12):6482. https://doi.org/10.3390/ijms22126482
Curtis PJ, van der Velpen V, Berends L, Jennings A, Feelisch M, Umpleby AM et al (2019) Blueberries improve biomarkers of cardiometabolic function in participants with metabolic syndrome-results from a 6-month, double-blind, randomized con-trolled trial. Am J Clin Nutr 109(6):1535–1545. https://doi.org/10.1093/ajcn/nqy380
Poulsen NB, Lambert MNT, Jeppesen PB (2020) The effect of plant derived bioactive compounds on inflammation: a systematic review and meta-analysis. Mol Nutr Food Res 64(18):e2000473. https://doi.org/10.1002/mnfr.202000473
McCullough ML, Peterson JJ, Patel R, Jacques PF, Shah R, Dwyer JT (2012) Flavonoid intake and cardiovascular disease mortality in a prospective cohort of US adults. Am J Clin Nutr 95:454–464. https://doi.org/10.3945/ajcn.111.016634
Jennings A, Welch AA, Fairweather-Tait SJ, Kay C, Minihane AM, Chowienczyk P et al (2012) Higher anthocyanin intake is associated with lower arterial stiffness and central blood pressure in women. Am J Clin Nutr 96:781–788. https://doi.org/10.3945/ajcn.112.042036
Amiot MJ, Riva C, Vinet A (2016) Effects of dietary polyphenols on metabolic syndrome features in humans: a systematic review. Obes Rev 17(7):573–586. https://doi.org/10.1111/obr.12409
Yang L, Ling W, Du Z, Chen Y, Li D, Deng S, Liu Z, Yang L (2017) Effects of anthocyanins on cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 8(5):684–693. https://doi.org/10.3945/an.116.014852
Xu L, Tian Z, Chen H, Zhao Y, Yang Y (2021) Anthocyanins, anthocyanin-rich berries, and cardiovascular risks: systematic review and meta-analysis of 44 randomized controlled trials and 15 prospective cohort studies. Front Nutr 8:747884. https://doi.org/10.3389/fnut.2021.747884
Curtis PJ, Berends L, van der Velpen V, Jennings A, Haag L, Chandra P, Kay CD, Rimm EB, Cassidy A (2022) Blueberry anthocyanin intake attenuates the postprandial cardiometabolic effect of an energy-dense food challenge: results from a double blind, randomized controlled trial in metabolic syndrome participants. Clin Nutr 41(1):165–176. https://doi.org/10.1016/j.clnu.2021.11.030
Johnson SA, Navaei N, Pourafshar S, Jaime SJ, Akhavan NS, Alvarez-Alvarado S et al (2020) Effects of montmorency tart cherry juice consumption on cardiometabolic biomarkers in adults with metabolic syndrome: a randomized controlled pilot trial. J Med Food 23(12):1238–1247. https://doi.org/10.1089/jmf.2019.0240
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting system-atic reviews and meta-analysis of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2021) Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane. www.training.cochrane.org/handbook
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
DerSimonian R, Kacker R (2007) Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 28(2):105–114. https://doi.org/10.1016/j.cct.2006.04.004
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Pedro-Botet J, Rodríguez-Padial L, Brotons C, Esteban-Salán M, García-Lerín A, Pintó X, Lekuona I, Ordóñez-Llanos J (2018) Homogenization of the lipid profile values. Clin Investig Arterioscler 30(1):36–48. https://doi.org/10.1016/j.arteri.2017.12.001
Sterne JA, Egger M, Smith GD (2001) Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 323(7304):101–105. https://doi.org/10.1136/bmj.323.7304.101
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P et al (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Santesso N, Glenton C, Dahm P, Garner P, Akl EA, Alper B et al (2020) GRADE Working Group. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. J Clin Epidemiol 119:126–135. https://doi.org/10.1016/j.jclinepi.2019.10.014
Balshem H, Helfand M, Schunermann HJ, Oxman AD, Kunz R, Brozek J et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015
Basu A, Fu DX, Wilkinson M, Simmons B, Wu M, Betts NM, Du M, Lyons TJ (2010) Strawberries decrease atherosclerotic markers in subjects with metabolic syndrome. Nutr Res 30(7):462–469. https://doi.org/10.1016/j.nutres.2010.06.016
Basu A, Du M, Leyva MJ, Sanchez K, Betts NM, Wu M, Aston CE, Lyons TJ (2010) Blueberries decrease cardiovascular risk factors in obese men and women with metabolic syndrome. J Nutr 140(9):1582–1587. https://doi.org/10.3945/jn.110.124701
Basu A, Betts NM, Ortiz J, Simmons B, Wu M, Lyons TJ (2011) Low-energy cranberry juice decreases lipid oxidation and increases plasma antioxidant capacity in women with metabolic syndrome. Nutr Res 31(3):190–196. https://doi.org/10.1016/j.nutres.2011.02.003
Desai T, Roberts M, Bottoms L (2019) Effects of Montmorency tart cherry supplementation on cardio-metabolic markers in metabolic syndrome participants: a pilot study. J Funct Foods 57:286–298. https://doi.org/10.1016/j.jff.2019.04.005
de Mello VD, Lankinen MA, Lindström J, Puupponen-Pimiä R, Laaksonen DE, Pihlajamäki J et al (2017) Fasting serum hippuric acid is elevated after bilberry (Vaccinium myrtillus) consumption and associates with improvement of fasting glucose levels and insulin secretion in persons at high risk of developing type 2 diabetes. Mol Nutr Food Res 61(9):1700019. https://doi.org/10.1002/mnfr.201700019
Gurrola-Díaz CM, García-López PM, Sánchez-Enríquez S, Troyo-Sanromán R, Andrade-González I, Gómez-Leyva JF (2010) Effects of Hibiscus sabdariffa extract powder and preventive treatment (diet) on the lipid profiles of patients with metabolic syn-drome (MeSy). Phytomedicine 17(7):500–505. https://doi.org/10.1016/j.phymed.2009.10.014
Jeong HS, Hong SJ, Lee TB, Kwon JW, Jeong JT, Joo HJ et al (2014) Effects of black raspberry on lipid profiles and vascular endo-thelial function in patients with metabolic syndrome. Phytother Res 28(10):1492–1498. https://doi.org/10.1002/ptr.5154
Kim H, Simbo SY, Fang C, McAlister L, Roque A, Banerjee N et al (2018) Açaí (Euterpe oleracea Mart.) beverage consumption improves biomarkers for inflammation but not glucose- or lipid-metabolism in individuals with metabolic syndrome in a randomized, double-blinded, placebo-controlled clinical trial. Food Funct 9(6):3097–3103. https://doi.org/10.1039/C8FO00595H
Puupponen-Pimiä R, Seppänen-Laakso T, Kankainen M, Maukonen J, Törrönen R, Kolehmainen M et al (2013) Effects of ellagitannin-rich berries on blood lipids, gut microbiota, and urolithin production in human subjects with symptoms of metabolic syndrome. Mol Nutr Food Res 57(12):2258–2263. https://doi.org/10.1002/mnfr.201300280
Stull AJ, Cash KC, Champagne CM, Gupta AK, Boston R, Beyl RA et al (2015) Blueberries improve endothelial function, but not blood pressure, in adults with metabolic syndrome: a randomized, double-blind, placebo-controlled clinical trial. Nutrients 7(6):4107–4123. https://doi.org/10.3390/nu7064107
Fabroni S, Ballistreri G, Amenta M, Romeo FV, Rapisarda P (2016) Screening of the anthocyanin profile and in vitro pancreatic lipase inhibition by anthocyanin-containing extracts of fruits, vegetables, legumes and cereals. J Sci Food Agric 96(14):4713–4723. https://doi.org/10.1002/jsfa.7708
Wu YHS, Chiu CH, Yang DJ, Lin YL, Tseng JK, Chen YC (2013) Inhibitory effects of litchi (Litchi chinensis Sonn.) flower-water extracts on lipase activity and diet-induced obesity. J Funct Foods 5(2):923–929. https://doi.org/10.1016/j.jff.2013.02.002
Park S, Kang S, Jeong DY, Jeong SY, Park JJ, Yun HS (2015) Cyanidin and malvidin in aqueous extracts of black carrots fermented with Aspergillus oryzae prevent the impairment of energy, lipid and glucose metabolism in estrogen-deficient rats by AMPK activation. Genes Nutr 10(2):6. https://doi.org/10.1007/s12263-015-0455-5
Sato D, Kusunoki M, Seino N, Nishina A, Feng Z, Tsutsumi K, Nakamura T (2015) Black soybean extract reduces fatty acid contents in subcutaneous, but not in visceral adipose triglyceride in high-fat fed rats. Int J Food Sci Nutr 66(5):539–545. https://doi.org/10.3109/09637486.2015.1028907
Xie L, Su H, Sun C, Zheng X, Chen W (2018) Recent advances in understanding the anti-obesity activity of anthocyanins and their biosynthesis in microorganisms. Trends Food Sci Technol 72:13–24. https://doi.org/10.1016/j.tifs.2017.12.002
Haswell C, Ali A, Page R, Hurst R, Rutherfurd-Markwick K (2021) Potential of beetroot and blackcurrant compounds to improve metabolic syndrome risk factors. Metabolites 11(6):338. https://doi.org/10.3390/metabo11060338
Naseri R, Farzaei F, Haratipour P, Nabavi SF, Habtemariam S, Farzaei MH, Khodarahmi R, Tewari D, Momtaz S (2018) Anthocyanins in the management of metabolic syndrome: a pharmacological and biopharmaceutical review. Front Pharmacol 4(9):1310. https://doi.org/10.3389/fphar.2018.01310
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S et al (2010) Heart disease and stroke statisticse 2010 update: a report from the American Heart Association. Circulation 23(7):948e54. 121. https://doi.org/10.1161/CIRCULATIONAHA.109.192667
Henning SM, Niu Y, Lee NH, Thames GD, Minutti RR, Wang H et al (2004) Bioavailability and antioxidant activity of tea fla-vanols after consumption of green tea, black tea, or a green tea extract supplement. Am J Clin Nutr 80:1558–1564. https://doi.org/10.1093/ajcn/80.6.1558
Peters U, Poole C, Arab L (2001) Does tea affect cardiovascular disease? A meta-analysis. Am J Epidemiol 154:495–503. https://doi.org/10.1093/aje/154.6.495
Upton R (2001) Bilberry fruit Vaccinium myrtillus L. In: Standards of analysis, quality control, and therapeutics. American Herbal Pharmacopoeia and Therapeutic Compendium, Santa Cruz
Chow HH, Cai Y, Hakim IA, Crowell JA, Shahi F, Brooks CA, Dorr RT, Hara Y, Alberts DS (2003) Pharmacokinetics and safety of green tea polyphenols after multiple-dose administration of epigallocatechin gallate and polyphenon E in healthy individuals. Clin Cancer Res 9(9):3312–3319
Chow HH, Hakim IA, Vining DR, Crowell JA, Ranger-Moore J, Chew WM, Celaya CA, Rodney SR, Hara Y, Alberts DS (2005) Effects of dosing condition on the oral bioavailability of green tea catechins after single-dose administration of Polyphenon E in healthy individuals. Clin Cancer Res 11(12):4627–4633. https://doi.org/10.1158/1078-0432.CCR-04-2549
Fang J (2014) Bioavailability of anthocyanins. Drug Metab Rev 46:508–520. https://doi.org/10.1016/j.foodchem.2016.05.122
Funding
No funding was obtained to conduct this systematic review and meta-analysis.
Author information
Authors and Affiliations
Contributions
Conceptualization: FA-Q, HG-E. Data curation: WS-L, JM. Formal analysis: FA-Q, AB-P. Methodology: HG-E, AB-P, WS-L. Supervision: FA-Q, LP, JFL-G. Writing-original draft: FA-Q, WS-L, JM, LP, JFL-G. Writing- review and editing: FA-Q, AB-P, HG-E, WS-L, JM, LP, JFL-G.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Araya-Quintanilla, F., Beatriz-Pizarro, A., Sepúlveda-Loyola, W. et al. Effectiveness of anthocyanins rich foods on cardiometabolic factors in individuals with metabolic syndrome: a systematic review and meta-analysis. Eur J Nutr 62, 1923–1940 (2023). https://doi.org/10.1007/s00394-023-03142-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03142-8