Abstract
Purpose
There is no evidence of a dietary index that measures not only the quantity but also the quality of protein. The aim is to investigate the association between a new dietary protein quality index (PQI) and micronutrient intake adequacy in a Mediterranean cohort.
Design
We assessed 17,535 participants’ diet at baseline using a semi-quantitative FFQ. The PQI was calculated according to the ratio of protein (g/d) sources: [fish, seafood, lean meat, pulses, eggs, nuts, low-fat dairy, and whole grains]/[red and ultra-processed meats, whole-fat or semi-skimmed dairy, potatoes and refined grains]. Participants were classified into quintiles of PQI. We evaluated the intakes of Fe, Cr, I, K, Mg, Ca, P, Na, Se, Zn and vitamins A, B1, B2, B3, B6, B12, C, E and folic acid. Micronutrient adequacy was evaluated using DRIs. Logistic regression analysis was used to assess the micronutrient adequacy according to quintiles of PQI.
Results
In this cross-sectional analysis, a total of 24.2% and 4.3% participants did not to meet DRIs in ≥ 4 and ≥ 8 micronutrients, respectively. The odds of failing to meet ≥ 4 and ≥ 8 DRI were lower in participants in the highest quintile of protein quality (OR = 0.22; IC 95% = 0.18, 0.26; P-trend < 0.001; and OR = 0.08; IC 95% = 0.05, 0.14; P-trend < 0.001, respectively) as compared to participants in the lowest quintile.
Conclusion
Higher PQI was found to be strongly associated with better micronutrient intake adequacy in this Mediterranean cohort. The promotion of high-quality protein intake may be helpful for a more adequate intake of micronutrients. The odds of failing to meet certain numbers of DRIs were lower rather than saying lower risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dietary proteins play an important role in growth, weight management and satiety [1], metabolic and renal function [2], prevention of muscle loss and management of sarcopenia on healthy aging and bone health [3]. An adequate protein intake is also key to build healthier diets adherence [4]. In terms of quantity, for adults aged > 19 years the Recommended Dietary Allowance (RDA) for proteins is 0.8 g of good quality protein per kilogram of body weight per day, representing 10–35% of total daily energy intake [5, 6]. This recommended amount is intended to maintain relative energy balance with amino acid oxidation and urea excretion, and nitrogen/protein balance [6].
Protein quality definition has been traditionally based on the quantity and their digestibility and the variety of amino acids. In the early nineties, the Food and Drug Administration, FAO and WHO adopted the Protein Digestibility-Corrected Amino Acid Score which defined protein quality according to human amino acid needs and human’s ability to digest [7]. Afterward, the Digestible Indispensable Amino Acid Score (DIAAS) was considered a more accurate protein quality method because it provides the proportion of the amino acid absorbed at the end of the small intestine [8]. The protein quality is based on the distribution of amino acids contained in the protein and in what amount the limiting amino acids (amino acids present in extremely low amounts in a food in relation to dietary needs) are available [9]. According to these criteria to define protein quality, animal protein has been traditionally classified as better-quality protein sources as compared to vegetable proteins because of their digestibility and their amino acid composition [10].
However, traditional scores of protein quality have some limitations [8, 11]: they do not take into account the net effects on human and environmental health, their limited representation of commonly consumed plant-based foods within the assessment framework [12], and insufficient awareness of the digestibility of commonly consumed heat-treated and processed plant-based foods [12]. DIAAS scores are intended to measure food quality, but do not take into account the food's net effects on human health and environmental impact. The FAO emphasized in its latest report on healthy and sustainable dietary guidelines, that a diet with lower environmental impacts could have associated health benefits [13]. Changing animal to plant proteins would reduce greenhouse gasses emissions, land use, and saturated fat intake [13], and replacing animal protein to legumes would also increase the intake of folic acid, high-quality carbohydrates (dietary fiber) and several other nutrients. Therefore, there is growing evidence that highlights the need to redefine the concept of protein quality, taking quality into account at this point [14]. In fact, it is suggested that with a proper combination of food sources, plant proteins can provide greater reductions in saturated fat intake and greater increases in fiber, vitamin A, vitamin C, folate, Mg, and K compared to animal sources [15]. However, to the best of our knowledge, no specific score, considering this broader definition of protein quality has been proposed in the context of epidemiological studies.
An adequate protein intake should be promoted to achieve the required micronutrient intake [16]. Commonly consumed food sources of protein are more than just protein but also significant sources of essential nutrients. Sources of dietary protein frequently contribute substantially to intakes of nutrients, such as Ca, vitamin D, K, dietary fiber, Fe, and folic acid, which have been identified as nutrients of “concern” (i.e., intakes are often lower than recommended) [17]. Current evidence suggests that the consumption of a variety of protein food sources, both animal and plant-based, is important to meet nutrient recommendations [17, 18]. Two previous studies have shown that greater consumption of protein-containing foods increases micronutrient adequacy, but they did not explore the relevance of protein quality [19, 20]. In previous investigations within the Seguimiento Universidad de Navarra (SUN) cohort and the PREvención con DIeta MEDiterránea (PREDIMED) study, we showed an association between both the carbohydrate quality index and the fat quality index with better micronutrient adequacy [21,22,23]. However, as far as we know, no previous study has assessed the association between a protein source quality index and micronutrient intake.
Our aim was, first, to define a new score for assessing not only the quantity but also the quality of protein intake that takes into account the amino acid profile, the association with health and the environmental impact; and second, to investigate the cross-sectional association between this score and the intake adequacy of 19 micronutrients in the SUN cohort, a Mediterranean cohort of young adults in Spain.
Subjects and methods
Study design and population
The SUN Project is a dynamic and multipurpose prospective cohort study conducted in Spain among university graduates since December 1999. This selection of highly educated participants corresponds to the approach known as restriction in epidemiology and it was applied to control for confounding by socioeconomic status [24, 25]. We are inviting to participate all Spanish alumni of the University of Navarra and several other professional collectives with a university degree. We select only those university graduates who are willing to commit themselves for returning questionnaires every 2 years. This cohort assesses the associations between diet and lifestyle and the occurrence of several diseases and chronic conditions. The recruitment is permanently open, and participants are followed-up biennially using questionnaires distributed by post or electronic mail. Overall, most participants are young adults (median age: 35 years, 82% younger than 50 years). The majority are women (61%), married (50%) or single (46%), and are graduated in a health-related profession (55%). A baseline questionnaire collects information related to lifestyle, medical history, socio-demographics, anthropometric, and several diet variables. More detailed information about this cohort has been previously described elsewhere [24].
In this study, we used a cross-sectional design to assess the association between the Protein source Quality Index (PQI) and micronutrient adequation at baseline. As of December 2019, the dataset collected a total of 22,894 participants who had answered the baseline questionnaire. We excluded 2169 individuals with intake levels outside predefined limits of total energy intake: < 800 kcal/d for men and < 500 kcal/d for women; > 4000 kcal/d for men and > 3500 kcal/d for women [26]. Finally, we excluded 3190 participants whose intake levels were outside predefined intake values of any micronutrient (≥ 3 standard deviations from both sides of the mean). Therefore, the final sample comprised 17,535 participants (Fig. 1).
Ethics
All participants received at entry to the SUN project a detailed written information and gave their permission to participate in the study. Voluntary completion of the baseline self-administrated questionnaire was considered to imply informed consent. This study was conducted according to the Declaration of Helsinki guidelines, and it was approved by the Research Ethics Committee of the University of Navarra. The SUN project is registered at clinicaltrials.gov as NCT02669602.
Exposure assessment: the dietary Protein source Quality Index
At baseline, food intake was assessed using a 136-item semi-quantitative food frequency questionnaire (FFQ), considering the consumption frequency over the past year. This FFQ was validated in Spain and subsequently re-evaluated [24, 27, 28]. The consumption of foods was asked at each item of the FFQ with a single frequency response ranging from “never or almost never” to “ ≥ 6 times a day”. Daily consumption of every food item was estimated by multiplying its typical portion size with its frequency of consumption using an ad hoc computer program specifically developed for this aim [29, 30].
The following criteria were applied to define the dietary PQI [5, 30,31,32]. First, we selected the main protein sources according to their contribution of foods in total protein intake among all participants of the SUN cohort (n = 22,894 recruited at baseline). We chose the following 12 food groups: red and processed meats, full-fat dairy, whole grains, potatoes and refined grains, lean meats, lean fish, reduced-fat dairy, pulses, fatty fish, eggs, seafood and finally nuts. All these food groups contributed to 81.84% of total protein intake in our population (Supplemental Table 1).
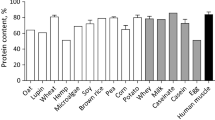
Second, we assessed the content of essential amino acids for each food source, and we determined the total quantity essential amino acid per 100 g of each food groups (Supplemental Table 2) using the German “Food Composition and Nutrition Tables (2008)” [32] and the USDA database [33]. Thus, we calculated essential amino acid content for each food group: histidine (His), isoleucine, (Ile) leucine (Leu), lysine (Lys), methionine (Met), phenylalanine (Phe), threonine, (Thr) tryptophan (Trp), and valine (Val). In this step we confirmed that the 12 food groups previously selected were the main contributors of essential amino acids.
Third, we classified protein-rich sources as healthy or unhealthy in accordance with Harvard and the American recommendations dietary guidelines [5, 34,35,36], and its climate impact measured as CO2 equivalent per kg edible weight according to the evidence [13]. Thus, the food group received one point for each one of the following criteria: high protein intake, high content of essential amino acids, consumption recommended for health reasons, and low climate impact with ≤ 4 kg CO2 equivalent per kg edible weight. Thus, to create the PQI, all the partial scores were added, and the final range was between 0 and 4. All foods or food groups with a score of 4 were assigned to the numerator (best quality) and those with ≤ 3 or fewer points to the denominator (Supplemental Table 3). Full-fat dairy products were located as unhealthy food groups due to its association with saturated fats and the risk of cardiovascular disease [37]. Red meats were also located as unhealthy food groups due to its consumption has been linked to major chronic diseases, such as diabetes, coronary heart disease, heart failure, stroke and cancer at various sites, and mortality [38]. Therefore, the dietary PQI was calculated using the following ratio: PQI = [proteins (g/d) from fish (lean and fatty) + seafood + lean meat + pulses + eggs + nuts + (low) fat dairy products + whole grains]/[proteins (g/d) from red and (ultra) processed meats + (whole and skimmed)fat dairy products + potatoes and refined grains].
Outcome assessment: micronutrient adequacy
In this study we assessed the following micronutrients: Fe, Cr, I, K, Mg, Ca, P, Na, Se, Zn and vitamins A, B1, B2, B3, B6, B12, C, E and folic acid. Baseline intake of these micronutrients was calculated using the FFQ and considering both the intake from foods and from dietary supplements. Micronutrient intakes were calculated as frequency multiplied by nutrient composition of specified portion size for each food item. It was used a computer-based program on available information in Spanish food composition tables [29, 30]. We used the Dietary References Intakes (DRI) values defined as quantitative estimates of nutrient intakes to be used for assessing and planning diets for healthy people [5, 14]. The DRI proposed by Institute of Medicine included four different values: Recommended Dietary Allowance (RDA), Adequate Intake (AI) values for nutrients having undetermined RDA, Estimated Average Requirement (EAR), and finally, Tolerable Upper Level values (UL).
We used the probabilistic approach to calculate the probability of intake inadequacy of all micronutrients with EAR values, as follows: z score = (estimated nutrient intake − EAR)/SD of the EAR. The z score corresponded to an estimated probability of inadequacy according to the normal distribution. This z score was not calculated for K and Cr because these micronutrients have AI values, but not EAR values [39]. Fe intake followed a skewed distribution, and for this reason we first log transformed its values.
Other co-variates
The baseline questionnaire in the SUN cohort includes several questions to collect sociodemographic data, lifestyle and health-related habits, self-reported anthropometric measures, family and personal medical history, and medication use. Physical activity information was gathered using the validated Spanish version of the Nurses’ Health Study and the Health Professionals Follow-up Study questionnaires [40]. Two subsamples of the SUN cohort were used to assess accuracy of self-reported weight and height [41] and physical activity [42]. We also used the Mediterranean Diet Score (MDS) [43] to assess the adherence to a Mediterranean diet pattern.
Statistical analyses
We calculated age and sex-adjusted baseline characteristics of participants using the Inverse Probability Weighting method. These variables were expressed as percentages and mean (SD) for categorical and continuous variables, respectively.
We used crude and multivariable logistic regressions models to assess the association between quintiles or deciles of the PQI and micronutrient intake adequacy at baseline using the EAR cut-off points and the probabilistic approach. We defined two different outcomes, according to two different cut-off points: ≥ 4 and ≥ 8 micronutrients with unmet DRI ≈25% and 50% respectively of the 19 micronutrients. We calculated odds ratios (ORs) of unmet micronutrient goals (≥ 4 or ≥ 8 micronutrients) with their 95% confidence interval (CIs) and we considered always the lowest quintile of the PQI as the reference category. Additionally, tests of linear trend across successive categories of PQI were conducted assigning the median value to each category and treating the variables as continuous.
We ran three multivariable-adjusted models: model 1 adjusted for age (continuous), sex and education level (graduate, master, and doctorate); model 2 additionally adjusted for energy intake (continuous); and model 3 additionally adjusted for the MDS (continuous), BMI (continuous), physical activity (continuous, MET-h/week), and smoking status (no smoking, former, current < 15 cig/d and current ≥ 15 cig/d). We did not adjust by socioeconomic status, because the baseline questionnaire does not collect this information.
We created a new variable combining the exposure to categories of PQI (Q1, merged Q2-Q4 and Q5) and adherence to MDS (in 2 groups categorized by the median) to evaluate the combined effect of the quality protein intake and Mediterranean diet adherence on unmet EAR for at least 50% of nutrients. We used as reference category the group of participants with best PQI and MDS. The likelihood ratio test was used to test the statistical significance of the interaction term between the MedDiet index categories and the PQI categories. As supplementary analysis, Student t tests were run to compare mean differences of inadequate minerals and vitamins intake between extreme quintiles of the PQI according to adherence to MDS. For this analysis we adjusted for total energy intake using the residual method [44].
Pearson’s correlation was applied to assess the association between each of the 19 micronutrients and animal protein (dairy protein, eggs, meat, fish, and processed and ultra-processed foods of animal origin), plant protein (vegetables, fruits, nuts, legumes, cereals, and soft drinks made with vegetable sources), and total protein (animal + plan protein). The total animal and plan protein was calculated using 85 and 47 items of FFQ, respectively. Pearson’s correlation was applied to assess the association of total protein, animal protein and plant protein with each of the 19 micronutrients.
We applied 4 sensitivity analyses. First, we analyzed the PQI adjusted for energy intake with the residual method; second, we analyze a modified PQI (Healthy Plate source Quality Index, HPPQI) based on the model for healthy proteins proposed in the Harvard’s Healthy Eating Plate [35]; third, no-excluding participants with implausible intakes; and fourth, applying different exclusions energy intakes criteria according to percentiles (P95; P99). For the HPPQI was calculated with the following ratio: HPPQI = [proteins (g/d) from seafood + poultry + pulses + nuts] / [proteins (g/d) from red and processed meats + cheese] [45].
Analyses were performed with STATA version 14.1 (STATA Corp., TX, USA). All P values are two-tailed and statistical significance was set at the conventional cut-off of P < 0.05.
Results
Age and sex-adjusted baseline characteristics of the 17,535 participants according to quintiles of the dietary PQI are summarized in Table 1. Participants with a higher PQI score were more likely to be single, former smokers, physically active, to follow a special diet, and to have higher baseline prevalence of hypertension, hypertriglyceridemia, and hypercholesterolemia; whereas they were less likely to snack between meals. Besides, those participants with higher PQI had also higher adherence to the MDS and higher consumption of fruits, nuts, fish, vegetables, lean meats, whole cereals and grains, reduced-fat dairy products and pulses; and a lower consumption of eggs, red and ultra-processed meats, and food products, full-fat dairy products and sugar-sweetened beverages (Table 1).
Table 2 shows age and sex-adjusted nutritional values of the study participants across the quintiles of the PQI. Participants with higher PQI had a lower intake of sugar, total fat, SFAs, cholesterol, and alcohol, whereas they presented slightly higher intake of MUFA and fiber. The intake of several micronutrients, including Ca, K, Mg, Zn, and vitamins A, B6, B12, C, D, E, and folic acid increased within the increasing quintiles of PQI, while Na intake was lower in the highest quintile. The contribution of different food groups on baseline essential amino acids is shown in Supplemental Table 2. Food groups were ordered according to their total amino acid content. Pulses, fish (fat and lean), seafood and meat (lean and red) were the main sources of amino acids.
Table 3 presents the ORs of not meeting ≥ 4 or ≥ 8 DRI according to the quintiles of PQI. When we used the probabilistic approach method to predict the risk of failing to meet DRI, participants in the highest quintile of PQI had a 74% (OR = 0.26; IC 95% = 0.21, 0.32; P for trend < 0.001) and 89% (OR = 0.11; IC 95% = 0.06, 0.18; P for trend < 0.001) lower odds of failing to meet ≥ 4 and ≥ 8 DRI, respectively, compared to the first quintile in model 3. When we repeated the analyses for failing to meet ≥ 4 or ≥ 8 DRI using the EAR cut-off point approach, the results were very similar. Moreover, we repeated the analyses using deciles to calculate the PQI to investigate the risk of not to meet ≥ 4 DRI (Fig. 2A) or ≥ 8 DRI (Fig. 2B). Results from this analysis supported the robustness of our main findings across quintiles of PQI, with a significant P for trend in both cases.
A, B OR and 95% confidence interval of unmet ≥ 4 or 8 Dietary Reference Intakes (DRI) respectively according to the deciles of protein source quality index in 17,535 participants of the SUN project (probabilistic approach). OR were adjusted for age (continuous), sex and education level (graduate, master, doctorate), energy intake (continuous), Mediterranean diet score (continuous), BMI (continuous), physical activity (metabolic equivalents-h/week), smoking status (no smoking, former, current < 15 cig/d, current ≥ 15 cig/d) and dietary supplement use (yes/no)
When we analyzed the prevalence of participants with unmet EAR for each micronutrient (Supplemental Table 4), we found higher percentages among participants in the lowest quintile of PQI.
Figure 3A, B shows the OR for unmet EAR for failing to meet ≥ 4 or ≥ 8 DRI according to the joint classification by PQI and MDS. No significant interaction was observed (P for interaction = 0.565) although participants with a higher PQI and higher adherence to the MedDiet presented a lower risk of unmet EAR compared to the lowest category of PQI and MedDiet. We also assessed the prevalence of inadequate micronutrient intake according to quintiles of PQI and stratified by level of adherence to the MedDiet. We observed that participants with higher adherence to MDS vs. lower adherence showed lower prevalence of inadequate Fe, Cr, K, Mg, Se and all vitamins (A, B complex, C, D and E) (P between groups < 0.001 in all except for B3 with P = 0.179 and B12 with P = 0.286), and statistically significant higher prevalence of inadequate, Ca and Zn in participants with higher vs. lower PQI score (Supplemental Tables 5 and 6).
A, B OR and 95% CI of unmet ≥ 4 or 8 Dietary Reference Intakes respectively according to PQI and adherence to Mediterranean diet (MedDiet) in 17,535 participants of the SUN Project. OR were adjusted for age (continuous), sex and education level (graduate, master, doctorate), energy intake (continuous), BMI (continuous), physical activity (MET-h/week), smoking status (no smoking, former, current < 15 cig/d, current ≥ 15 cig/d) and dietary supplement use (yes/no). Abbreviations: Q, Quintiles, MDS, Mediterranean Diet
Pearson’s correlations showed that total protein intake was strongly associated with animal protein because there is a high dietary content of animal food sources compared to plant protein (Supplemental Figure 1). A strong association of total protein was found with intakes of Mg, P, vitamins B1, B2, B3, and B6, present mainly in foods of animal origin, and a moderate association with intakes of vegetable protein, I, Zn, Na, K, Cr, folic acid and vitamin B12, and vitamin E in our cohort (Supplemental Figure 1). Intake of animal protein was moderately associated with all minerals and vitamin B1, B6 and B12, and strongly associated with vitamin B2 and B3 (found mainly in sources of animal origin). On the contrary, intake of vegetable protein was strongly associated with intakes of Fe, Mg, K, and vitamin B1, and moderately associated with the rest of the minerals except I and Na (Supplemental Figure 1).
Finally, we performed 4 sensitivity analyses: (I) adjusting for total energy intake using the residual method; (II) redefining the PQI using the HPPQI; (III) no-excluding participants with implausible intakes; and (IV) applying different exclusions energy intakes criteria according to percentiles (< P5 and > P95; < P1 and > P99). When we adjusted the score using the residual method, the results showed that a highest PQI had a 82% (OR = 0.18; IC 95% = 0.14, 0.24; P for trend < 0.001) and 97% (OR = 0.03; IC 95% = 0.01, 0.10; P for trend < 0.001) lower risk of falling to meet ≥ 4 or ≥ 8 DRI, respectively, as compared to the lowest quintile in the probabilistic approach model. When we used the cut-off approach model using the residual method results were apparently similar (OR = 0.22; IC 95% = 0.18, 0.26; P for trend < 0.001; and OR = 0.08; IC 95% = 0.05, 0.14; P for trend < 0.001, of falling to meet ≥ 4 or ≥ 8 DRI respectively). When we used the HPPQI, the odds of participants in the highest quintile of HPPQI of not meeting ≥ 4 or ≥ 8 DRI was lower than participants in the lowest HPPQI. The OR of unmet ≥ 4 DRI was 0.50 (IC 95% = 0.43, 0.59; P for trend < 0.001) for the cut-off points and 0.60 (IC 95% = 0.49, 0.73; P for trend < 0.001) for the probability approach. The OR of unmet ≥ 8 DRI was 0.55 (IC 95% = 0.41, 0.75; P for trend < 0.001) for the cut-off points approach and 0.49 (IC 95% = 0.30, 0.78; P for trend = 0.004) for the probabilistic approach. These results show that the odds of unmet DRI between extreme quintiles were lower when the quality of protein intake was measured with the dietary PQI than with the HPPQI. Lastly, after no-excluding participants with implausible energy intakes and after applying different exclusions energy intakes criteria according to percentiles (P95; P99), the results were very similar to our main analysis (Supplemental Figure 2).
Discussion
To our knowledge, the present study is the first to develop a score of a dietary PQI according to the content of essential amino acids, the health benefits and environmental impact of the protein sources, and to investigate the association between the PQI and the adequacy of micronutrient intake in a large Mediterranean cohort. Participants with higher PQI scores (PQI range in Q5 1.3 to 41.1) had lower energy intake with a higher consumption of protein groups with better quality (fish, white meat, legumes, eggs, nuts, low-fat dairy products, and whole grains) compared to those with a lower reference score (PQI range in Q1 0 to < 0.5). In addition, they had better lifestyles (more active, less snacking between meals, more special diets, and greater adherence to the MedDiet). Since total protein intake is relatively stable [46], the PQI likely promotes a higher intake of healthy proteins at the expense of reducing the intake of unhealthy proteins. We found that participants with higher PQI had a lower risk of having an inadequate intake of micronutrients. We found that the odds of not meeting ≥ 4 and ≥ 8 DRIs were lower when we controlled in multivariable model 2 for energy intake. These results suggest that total energy intake was an important confounding factor. When we adjusted in model 3 for different lifestyles, the odds of not meeting ≥ 4 and ≥ 8 DRIs were also lower, although less pronounced. In addition, those participants with better adherence to the MedDiet were more likely to meet micronutrient recommendations compared to those with lowest adherence. No significant interaction was observed between the PQI and the level of adherence to the MDS.
Few studies previously addressed the association between protein quantity with diet quality and micronutrient adequacy on adult population. In a cross-sectional study in the United States high protein density was associated with a greater probability of nutritional adequacy, independently of the intake of fruits and vegetables [19]. Findings from the French Individual and National Consumption Survey 2 suggested that plant protein is a robust marker of a healthy and quality diet, whereas total animal protein includes different subtypes of animal protein that largely vary in their relationship with diet quality [20]. Lastly, they conclude that plant-based protein intake is a general and robust marker of nutrient adequacy of the diet, and hence of a healthy diet. In other studies, Canadian and American adults who reported a higher consumption of proteins from plant-based foods has reported an enhanced micronutrient intake resulting in lower individuals who were below the EAR for vitamins B1, B6, and folic acid, Fe, Mg, P, and Zn compared with non-consumers [47, 48].
Dietary protein patterns constitute strong elements in the background structure of the dietary intake of a general population and are associated with different nutrient profiles [18]. In our study, a higher PQI is associated with higher protein consumption, but specifically it reflects a higher intake of healthy plant and animal protein sources with lower environmental impact (such as fish, lean meat, and reduced-fat dairy products) [49, 50]. One of the results of our study confirms that the relationship between animal protein and diet quality extends beyond the case of meat, and the intake of plant protein shows strong associations with patterns of micronutrient intake (Supplemental Figure 1). For this reason, a combined consumption of protein of animal and vegetable origin would be able to fill possible micronutrient lacks in the diet and it will ensure to achieve the necessary micronutrient profile. Our results suggest that multidimensional assessment of protein source quality also appears to be important in adequate micronutrient intake, and an approach based solely on protein quantity could limit health benefits and favor a higher environmental footprint. Thus, in agreement with other recent dietary quality indexes that have assessed the carbohydrate and fat quality [21], the quality of protein sources is strongly considered as a link to the micronutrient adequacy of the diet. Moreover, our results also justify the relevance of using a global assessment tool of nutrient adequacy when studying the relationship between the intake of animal- and vegetable-source proteins and the quality of the micronutrient contribution or other variables related to health. It should be noted that good quality of protein intake does not require the complete elimination of animal products.
Adequate dietary protein intake provides a source of micronutrients as well as amino acids, including the 9 essential amino acids. The dietary PQI was calculated according to the content of essential amino acids in each food group. Animal-source foods, such as meats, dairy products, eggs, fish or seafood, contain higher amounts of amino acids than plant-source foods, such as cereals, vegetables, potatoes, legumes, nuts, and seeds [8]. One of the reasons that defines the quality of protein in the diet refers to the concept of "limiting amino acid" [9]. The 2 amino acids most likely to be limiting are LYS and MET in pulses and cereals [9]. In this way, our index considers legumes and whole grains, advocating that both food groups can be part of a dietary pattern that, in addition to being healthy, provides an adequate number of micronutrients and in their proportion of quality amino acids. It is widely believed by the general population that many plant foods are completely lacking in specific amino acids, and therefore protein sufficiency cannot be supported by plant foods alone. However, all plant foods contain the 20 amino acids in the diet [9], as shown in Supplemental Figure 3. Thus, although the amount of essential amino acids is higher in foods of animal origin, the proportion of each amino acid essential in plant foods follows a similar distribution as in those of animal origin.
The MedDiet is an example that the combination of healthy animal-source proteins and vegetable-source proteins contribute to a sufficient amount of micronutrients in the diet, excellent sources of Zn, I, Se, Fe, Ca, K, P, Mg, Cr and vitamins B1, B2, B3, B6, B12, C, A, D and folic acid [19, 21, 51]. Several studies concluded that following a MedDiet pattern was associated with a lower risk of unmeet the EAR of micronutrients [21, 23]. In accordance with this, in our study those participants who adhered more to the MedDiet and scored a higher PQI would cover most of the micronutrients, but a possible inadequacy in I, Ca and Zn would have to be taken into account. To compensate the possible deficiency of these micronutrients, the substitution of meat for fish and seafood (main source of I); a higher consumption of small fish, such as sardines, anchovies, green leafy vegetables (secondary sources of Ca); and a higher consumption of nuts and legumes (secondary sources of Zn) could be recommended. Moreover, we found that regardless of the MedDiet, the effect of the PQI on the risk of nutritional inadequacy was not modified.
Our study has some limitations. First, to calculate the dietary PQI we did not take into account other food groups (fruits, vegetables, drinks, bakery, pastries and other processed products) associated with protein intake in the SUN cohort. However, the PQI includes those foods that contribute to the highest percentage of total protein intake (the 12 groups contribute 81.84% of total protein intake vs. an estimated mean of protein contribution of 86.84% according to the data available in the Spanish ANIBES study [52]). Similar percentage contribution was found in the National Health and Nutrition Examination Survey 2007–2010 [17] where the top food sources of protein achieved approximately 73% of total daily protein intake. Third, we used a self-reported FFQ to estimate food consumption and nutrient intake, which can be an important source of information bias. However, the FFQ is considered the most appropriate tool in epidemiology and the most practical and feasible tool to evaluate food habits in large epidemiological studies [53]. Besides, our sample comprised highly educated participants, so the data probably have fairly adequate quality [54], and the FFQ was previously validated in Spain and subsequently re-evaluated [24, 27, 28]. Fourth, there is currently a lack of scientific agreement on the health properties according to the type of dairy or red meat. Since the underpinning information in our study was collected from a FFQ, our score cannot disentangle any subtle differences between types of fat in dairy products (low-fat, semi-skim or whole dairy) and between red or processed meat. Fifth, total dietary intake of micronutrients could be underestimated, although we included the intake from foods and from dietary supplements in the data analysis (without considering the intake of fortified foods or medication that participants might be consuming). Sixth, our study assessed the probability of adequacy but did not indicate nutrient deficiencies which should be confirmed by biomarkers of nutrient intake. Seventh, the dietary PQI definition took into account the environmental effect according to the Dietary Guidelines for Americans (2020–2025) and FAO, but it did not assess the life cycle assessment that is a common choice for assessment the environmental impact of food measure as the resource use, pollutant emissions, and other potential impacts of foods [36]. Eighth, we did not collect information on the socioeconomic status of participants. Since all participants in the SUN cohort are university graduates, they are not very heterogeneous regarding their socioeconomic and educational status. However, we are not able to know whether lack of affordability of high-quality foods can be related to suboptimal intake of some micronutrients and to the overall health-related lifestyles in participants of our cohort. Ninth, we used international sources, such as the USDA and German food databases, to obtain information on essential amino acids, which may not ideally reflect the content of essential amino acids in our Spanish population.
The strengths of the present study are that all data were obtained from a Mediterranean cohort with a relatively large sample size and a high response rate (91%). Second, the components of dietary PQI were based on international evidence and recommendations. Third, our analysis was obtained using two different methods to estimate nutrient intake adequacy: the probabilistic approach and the EAR cut-point approach. Fourth, the FFQ was validated in Spain and subsequently re-evaluated [24, 27, 28].
In conclusion, it is possible to develop a quality indicator of protein intake considering not only quantity and amino acid content of proteins but also the health and environmental effects of each protein food source. A higher protein source quality is associated with better micronutrient intake adequacy in this long Mediterranean cohort. These results could contribute to the development of future dietary recommendations regarding the quantity and quality of protein intake. It would be interesting to incorporate the impact on human and environmental health into future international recommendations on protein intake. Protein consumption should be promoted, in moderate amounts and within the framework of a balanced diet the healthiest and sustainable foods. In addition, we believe that investigating this multidimensional concept of dietary protein quality should be transferred to other populations to analyze how it would influence nitrogen balance or body mass/protein balance using the PQI. Therefore, more studies are required in other populations to evaluate the efficacy and validity of this new dietary protein quality index. Further studies are required in other populations to evaluate the efficacy of this novel dietary quality index.
Availability of data and material
This study uses data from the Seguimiento Universidad de Navarra (SUN) cohort. All data and materials as well as software application or custom code used during the current study shall be made available from the corresponding author on reasonable request.
Abbreviations
- AI:
-
Adequate intake
- DRI:
-
Dietary References intakes
- EAR:
-
Estimated Average Requirement
- FFQ:
-
Food Frequency Questionnaire
- HPPQI:
-
Harvard's healthy eating Plate Protein source Quality Index
- His:
-
Histidine
- Ile:
-
Isoleucine
- Leu:
-
Leucine
- Lys:
-
Lysine
- Met:
-
Methionine
- MDS:
-
Mediterranean Diet Score
- MEDAS:
-
Mediterranean Diet Adherence Screener
- OR:
-
Odds Ratios
- Phe:
-
Phenylalanine
- PQI:
-
Protein source Quality Index
- PREDIMED:
-
PREvención con DIeta MEDiterránea
- RDA:
-
Recommended Dietary Allowance
- SUN:
-
Seguimiento Universidad de Navarra
- Thr:
-
Threonine
- Trp:
-
Tryptophan
- UL:
-
Tolerable upper level values
- Val:
-
Valine
References
Leidy HJ, Clifton PM, Astrup A et al (2015) The role of protein in weight loss and maintenance. Am J Clin Nutr. https://doi.org/10.3945/ajcn.114.084038
Rodriguez NR (2015) Introduction to Protein Summit 2.0: continued exploration of the impact of high-quality protein on optimal health. Am J Clin Nutr. https://doi.org/10.3945/ajcn.114.083980
Paddon-Jones D, Campbell WW, Jacques PF et al (2015) Protein and healthy aging. Am J Clin Nutr. https://doi.org/10.3945/ajcn.114.084061
Carbone JW, McClung JP, Pasiakos SM (2019) Recent advances in the characterization of skeletal muscle and whole-body protein responses to dietary protein and exercise during negative energy balance. Adv Nutr. https://doi.org/10.1093/advances/nmy087
Institute of Medicine of the National Academies (2005) Dietary reference intakes: dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients)
Nishimura Y, Højfeldt G, Breen L et al (2021) Dietary protein requirements and recommendations for healthy older adults: a critical narrative review of the scientific evidence. Nutr Res Rev. https://doi.org/10.1017/S0954422421000329
Food and Agriculture Organization (2013) Dietary protein quality evaluation in human nutrition: report of an FAO Expert Consultation. http://www.fao.org/documents/card/en/c/ab5c9fca-dd15–58e0–93a8-d71e028c8282
FAO Food Nutr Pap (2013) Dietary protein quality evaluation in human nutrition. Report of an FAQ Expert Consultation
Gardner CD, Hartle JC, Garrett RD et al (2019) Maximizing the intersection of human health and the health of the environment with regard to the amount and type of protein produced and consumed in the United States. Nutr Rev. https://doi.org/10.1093/nutrit/nuy073
Tomé D (2013) Digestibility issues of vegetable versus animal proteins: protein and amino acid requirements—functional aspects. Food Nutr Bull. https://doi.org/10.1177/156482651303400225
Schaafsma G (2012) Advantages and limitations of the protein digestibility-corrected amino acid score (PDCAAS) as a method for evaluating protein quality in human diets. Br J Nutr. https://doi.org/10.1017/S0007114512002541
Craddock JC, Genoni A, Strutt EF, Goldman DM (2021) Limitations with the Digestible Indispensable Amino Acid Score (DIAAS) with special attention to plant-based diets: a review. Curr Nutr Rep. https://doi.org/10.1007/s13668-020-00348-8
Gonzalez Fischer C, Garnett T (2016) Developments in national healthy and sustainable dietary guidelines: a state of play assessment (FAO)
Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes (2000) Dietary reference intakes: applications in dietary assessment. National Academies Press, Washington, D.C.
Katz DL, Doughty KN, Geagan K et al (2019) Perspective: the public health case for modernizing the definition of protein quality. Adv Nutr 10:755–764. https://doi.org/10.1093/advances/nmz023
Wolfe RR, Cifelli AM, Kostas G, Kim I-Y (2017) Optimizing protein intake in adults: interpretation and application of the recommended dietary allowance compared with the acceptable macronutrient distribution range. Adv Nutr 8:266–275. https://doi.org/10.3945/an.116.013821
Phillips SM, Fulgoni VL, Heaney RP et al (2015) Commonly consumed protein foods contribute to nutrient intake, diet quality, and nutrient adequacy. Am J Clin Nutr 101:1346S-1352S. https://doi.org/10.3945/ajcn.114.084079
de Gavelle E, Huneau J-F, Mariotti F (2018) Patterns of protein food intake are associated with nutrient adequacy in the General French Adult Population. Nutrients. https://doi.org/10.3390/nu10020226
Gwin JA, Karl JP, Lutz LJ et al (2019) Higher protein density diets are associated with greater diet quality and micronutrient intake in healthy young adults. Front Nutr. https://doi.org/10.3389/fnut.2019.00059
Camilleri GM, Verger EO, Huneau J-F et al (2013) Plant and animal protein intakes are differently associated with nutrient adequacy of the diet of French Adults. J Nutr. https://doi.org/10.3945/jn.113.177113
Zazpe I, Sánchez-Taínta A, Santiago S et al (2014) Association between dietary carbohydrate intake quality and micronutrient intake adequacy in a Mediterranean cohort: the SUN (Seguimiento Universidad de Navarra) Project. Br J Nutr 111:2000–2009. https://doi.org/10.1017/S0007114513004364
Martínez-González MA, Fernandez-Lazaro CI, Toledo E et al (2020) Carbohydrate quality changes and concurrent changes in cardiovascular risk factors: a longitudinal analysis in the PREDIMED-Plus randomized trial. Am J Clin Nutr 111:291–306. https://doi.org/10.1093/ajcn/nqz298
Sánchez-Tainta A, Zazpe I, Bes-Rastrollo M et al (2016) Nutritional adequacy according to carbohydrates and fat quality. Eur J Nutr 55:93–106. https://doi.org/10.1007/s00394-014-0828-3
Carlos S, de La Fuente-Arrillaga C, Bes-Rastrollo M et al (2018) Mediterranean diet and health outcomes in the SUN Cohort. Nutrients. https://doi.org/10.3390/nu10040439
Rothman KJ, Greenland S, Lash TL (2008) Design strategies to improve study accuracy. In: Rothman KJ, Greenland S, Lash TL (eds) Modern epidemiology, 3rd ed. Lippincott Williams and Wilkins, Philadelphia, PA
Willett WC (2013) Nutritional epidemiology, 3rd edn. Oxford University Press, New York, NY
de la Fuente-Arrillaga C, Ruiz ZV, Bes-Rastrollo M et al (2010) Reproducibility of an FFQ validated in Spain. Public Health Nutr 13:1364–1372. https://doi.org/10.1017/S1368980009993065
Martin-Moreno JM, Boyle P, Gorgojo L et al (1993) Development and validation of a food frequency questionnaire in Spain. Int J Epidemiol 22:512–519. https://doi.org/10.1093/ije/22.3.512
Moreiras O, Carbajal A, Cabrera L (2005) Tablas de composición de alimentos., Pirámide. Madrid
Mataix Verdú J (2003) Tabla de composición de alimentos españoles (Spanish Food Composition Table), 4th edn. Universidad de Granada, Granada
Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes, Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes (2014) NDL/FNIC food composition database home page. http://ndb.nal.usda.gov/
Souci SW, Fachmann W, Kraut H (2008) Food composition and nutrition tables, 7th revised and completed edition
U.S. Department of Agriculture Food data. https://fdc.nal.usda.gov
Harvard T.H. Chan School of Public Health (2019) What Should I Eat? Protein. https://www.hsph.harvard.edu/nutritionsource/what-should-you-eat/protein/
Healthy Eating Plate | The Nutrition Source | Harvard T.H. Chan School of Public Health. https://www.hsph.harvard.edu/nutritionsource/healthy-eating-plate/
2020–2025 Dietary Guidelines for Americans. U. S. Department of Agriculture and Department of Health and Human Services. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
(2021) Is low-fat or full-fat the better choice for dairy products?
Wolk A (2017) Potential health hazards of eating red meat. J Intern Med 281:106–122. https://doi.org/10.1111/joim.12543
Anderson GH, Peterson RD, Beaton GH (1982) Estimating nutrient deficiencies in a population from dietary records: the use of probability analyses. Nutr Res. https://doi.org/10.1016/S0271-5317(82)80049-3
Elosua R, Marrugat J, Molina L et al (1994) Validation of the Minnesota leisure time physical activity questionnaire in Spanish men. Am J Epidemiol 139:1197–1209. https://doi.org/10.1093/oxfordjournals.aje.a116966
Bes-Rastrollo M, Perez Valdivieso JR, Sanchez-Villegas A et al (2005) Validation of self-reported weight and body mass index of the participants of a cohort of university graduates. Rev Espanola Obesidad 3:352–358
Martínez-González MA, López-Fontana C, Varo JJ et al (2005) Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr 8:920–927. https://doi.org/10.1079/phn2005745
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348:2599–2608. https://doi.org/10.1056/NEJMoa025039
Willett WC (2013) Nutritional epidemiology: issues in analysis and presentation of dietary data, 3rd edn. Oxford University Press, New York, NY
Santiago S, Zazpe I, Fernandez-Lazaro CI et al (2021) Macronutrient Quality and All-Cause Mortality in the SUN Cohort. Nutrients. https://doi.org/10.3390/nu13030972
Lieberman HR, Fulgoni VL, Agarwal S et al (2020) Protein intake is more stable than carbohydrate or fat intake across various US demographic groups and international populations. Am J Clin Nutr 112:180–186. https://doi.org/10.1093/ajcn/nqaa044
Mudryj AN, Yu N, Hartman TJ et al (2012) Pulse consumption in Canadian adults influences nutrient intakes. Br J Nutr. https://doi.org/10.1017/S0007114512000724
Mitchell DC, Lawrence FR, Hartman TJ, Curran JM (2009) Consumption of dry beans, peas, and lentils could improve diet quality in the US population. J Am Diet Assoc. https://doi.org/10.1016/j.jada.2009.02.029
Drewnowski A, Rehm CD, Martin A et al (2015) Energy and nutrient density of foods in relation to their carbon footprint. Am J Clin Nutr. https://doi.org/10.3945/ajcn.114.092486
González-García S, Esteve-Llorens X, Moreira MT, Feijoo G (2018) Carbon footprint and nutritional quality of different human dietary choices. Sci Total Environ. https://doi.org/10.1016/j.scitotenv.2018.06.339
Santiago S, Zazpe I, Gea A et al (2018) Fat quality index and risk of cardiovascular disease in the sun project. J Nutr Health Aging 22:526–533. https://doi.org/10.1007/s12603-018-1003-y
Ruiz E, Ávila J, Valero T et al (2016) Macronutrient distribution and dietary sources in the Spanish population: findings from the ANIBES Study. Nutrients. https://doi.org/10.3390/nu8030177
Shim J-S, Oh K, Kim HC (2014) Dietary assessment methods in epidemiologic studies. Epidemiol Health. https://doi.org/10.4178/epih/e2014009
Winckers ANE, Mackenbach JD, Compernolle S et al (2015) Educational differences in the validity of self-reported physical activity. BMC Public Health 15:1299. https://doi.org/10.1186/s12889-015-2656-7
Acknowledgements
We thank other members of the SUN Group: Alonso A, Álvarez-Álvarez I, Balaguer A, Barbagallo M, Barrientos I, Barrio-López MT, Basterra-Gortari FJ, Battezzati A, Bazal P, Benito S, Bertoli S, Bes-Rastrollo M, Beulen Y, Beunza JJ, Buil-Cosiales P, Canales M, Carlos S, Carmona L, Cervantes S, Cristobo C, de Irala J, de la Fuente-Arrillaga C, de la Rosa PA, Delgado-Rodríguez M, Díaz-Gutiérrez J, Díez Espino J, Domínguez L, Donat-Vargas C, Donazar M, Eguaras S, Fernández-Montero A, Fresán U, Galbete C, García-Arellano A, García López M, Gutiérrez-Bedmar M, Goméz-Domingos AL, Gómez-Donoso C, Gómez-Gracia E, Goñi E, Guillén F, Henríquez P, Hernández A, Hershey MS, Hidalgo-Santamaría M, Hu E, Lahortiga F, Leone A, Llorca J, López del Burgo C, Marí A, Marques I, Martí A, Martín-Moreno JM, Martínez-Lapiscina EH, Mendonça R, Menéndez C, Molendijk M, Molero P, Murphy K, Muñoz M, Núñez-Córdoba JM, Pajares R, Papadaki A, Parletta N, Pérez de Ciriza P, Pérez Cornago A, Pérez de Rojas J, Pimenta AM, Pons J, Ramallal R, Razquin C, Rico A, Ruano C, Ruiz L, Ruiz Zambrana A, Salgado E, San Julián B, Sánchez D, Sánchez-Tainta A, Sánchez-Villegas A, Sayón-Orea C, Schlatter J, Serrano-Martinez M, Toledo J, Tortosa A, Valencia F, Vázquez Z, Zarnowiecki D. We thank very specially all participants in the SUN cohort for their long-standing and enthusiastic collaboration and our advisors from Harvard TH Chan School of Public Health Walter Willett, Alberto Ascherio, Frank B. Hu and Meir J. Stampfer who helped us to design the SUN Project, the PREDIMED study and the PREDIMED-PLUS on-going trial.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. The SUN Project has received funding from the Spanish Government-Instituto de Salud Carlos III, and the European Regional Development Fund (FEDER) (RD 06/0045, CIBER-OBN, Grants PI10/02658, PI10/02293, PI13/00615, PI14/01668, PI14/01798, PI14/01764, PI17/01795, PI20/00564, and G03/140), the Navarra Regional Government (27/2011, 45/2011, 122/2014), the National Plan on Drugs (2020/021), and the University of Navarra.
Author information
Authors and Affiliations
Contributions
The author’s contributions were as follows: IZ and MR-C conceived and designed the study, provided insight into the general statistical analysis, and conducted the review of the first draft and tables. MRC, IZ, SS, LG and CFA helped with the methodology. MAMG obtained funding contributed to the data collection. All authors reviewed and approved the manuscript and given the final approval version to be published. None of the authors reported a conflict of interest related to the study.
Corresponding author
Ethics declarations
Conflict of interest
All authors declared no conflicts of interest to disclose.
Ethics approval
Participants received written information about the specific data required in the questionnaires, the protection to safeguard their privacy, and the future feedback from the research team. We also informed the potential candidates of their right to refuse to participate in the SUN study or to withdraw their consent to participate at any time without reprisal, according to the principles of the Declaration of Helsinki. The Research Ethics Committee of the University of Navarra approved this method (number 2001_30) to request the informed consent of participants. This cohort is registered at clinicaltrials.gov as NCT02669602.
Consent to participate
All participants gave written, informed consent at enrollment.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de la O, V., Zazpe, I., de la Fuente-Arrillaga, C. et al. Association between a new dietary protein quality index and micronutrient intake adequacy: a cross-sectional study in a young adult Spanish Mediterranean cohort. Eur J Nutr 62, 419–432 (2023). https://doi.org/10.1007/s00394-022-02991-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02991-z