Abstract
Purpose
Eating disorders (ED) and anxiety impact food choices. In addition, comorbid anxiety seems to increase ED symptoms and severity. However, the association between such comorbidity and dietary intake is unknown. This population-based, cross-sectional study aimed to assess macronutrient intake according to mental health status (i.e., no disorder, pure and comorbid anxiety and ED).
Methods
The study included N = 24,771 participants (74% female, mean age = 53.2 ± 13.7 years) in the NutriNet-Santé cohort, who completed once the trait subscale of the State-Trait Anxiety Inventory (STAI-T; high anxiety: ≥ 40 points) between 2013 and 2016 and the SCOFF questionnaire screening for ED in 2014. The Expali algorithm was applied to categorize ED (no ED; restrictive: RS; bulimic: BL; hyperphagic: HP; other ED). Participants were divided into ten groups by crossing their anxiety status (two groups: low or high) and their ED status (five groups). Macronutrient intakes were evaluated from ≥ 3 24-h dietary records. Analyses of covariance (ANCOVA) and Dunnett-Hsu tests (reference = no disorder) were performed.
Results
Significant differences in macronutrient intake were seen between the pure and comorbid forms, especially for RS and HP. Compared to the “no disorder” group, a significantly higher percentage of energy from carbohydrates, higher intakes of total carbohydrates, simple sugars, and plant-based protein, lower intakes of total fat, saturated and monounsaturated fatty acids, and cholesterol were observed in the comorbid anxiety + RS group, but not in the pure RS group. In contrast, significantly lower intakes of added sugar and plant-based protein, and a higher intake of cholesterol were observed in the pure HP group, but not in the comorbid anxiety + HP group. For BL and other ED, similar results were observed between the pure and comorbid forms.
Conclusion
This large epidemiological study provided some support for differences in macronutrient intake between individuals with pure or comorbid anxiety and ED. Differences in intake were largely dependent on ED type. Future prospective studies and studies using clinically defined anxiety and ED are needed to elucidate causality as well as potential effect modification of the observed associations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite their considerable deleterious impact on daily life, frequent comorbidity, and increasing share of the global disease burden [1], mental disorders continue to receive insufficient research attention [2]. Among nearly twenty disorder categories in the DSM-5, feeding and eating disorders (ED) are characterized by a long-term disturbance in eating-related behaviors that has a substantial effect on physical and psychosocial functioning [3]. Restrictive disorders, especially anorexia nervosa (AN), bulimic disorders, and binge-eating disorders (BED) are considered typical ED and have been the main focus of ED research [4]. An ED-related increased mortality risk in young adulthood has been reported [5]. Yet, ED prevalence in middle age is not uncommon [6, 7]. Moreover, individuals suffering from ED often present with mental comorbidity, especially anxiety disorders [3, 5], which occur more frequently in that subgroup than in the general population [8].
Comorbidity is defined as the presence/accumulation of ≥ 2 distinct health conditions (physical and/or mental) in the same individual; it is linked with increased symptom severity, poorer health outcomes [9] and reduced quality of life [10]. In the case of ED, comorbid anxiety has been associated with worse ED psychopathology and increased ED symptom severity relative to pure ED or to comorbid depression [11, 12]. Longitudinal evidence has shown that mental comorbidity in ED can predict poor outcomes, including greater risk for relapse and premature death [13].
Whereas by definition ED feature problematic dietary intake [3], anxiety status, especially trait anxiety, has also been shown to impact dietary intake [14,15,16]. Individuals with AN avoid high-energy food rich in sugar and fat [17, 18], whereas intake of such foods seems to be positively associated with BED [18,19,20]. As regards anxiety disorders, epidemiological studies suggest an inverse association between diet quality and risk of anxiety, although nutritional interventions are needed to confirm this effect [16]. Recent research revealed a decrease in total caloric intake and an increase in sugar consumption among young adults self-reporting anxiety symptoms [21]. However, there is a paucity of research on the link between macronutrient intake and anxiety [14,15,16]. Despite reported associations between trait anxiety and food/nutrient intake [14, 15, 17, 19, 20], possible mediating and/or moderating effects of anxiety regarding ED [22,23,24], and the high ED-anxiety comorbidity [3], no study, to our knowledge, has investigated dietary/nutrient intake among individuals with such comorbidity. We hypothesized that individuals with anxiety and/or ED have different macronutrient intakes from people without these disorders, and that unfavorable dietary intake (underscored by reduced nutrient diversity) is more pronounced in the case of mental comorbidity. Therefore, the aim of this population-based cross-sectional study was to evaluate macronutrient intakes according to the presence of anxiety and/or ED in pure or comorbid form, in a large adult sample.
Material and methods
The NutriNet-Santé web-cohort
NutriNet-Santé is a French ongoing prospective web-cohort launched in 2009. Details about its design, protocol, and main research goals can be found elsewhere [25]. Briefly, media announcements (e.g., television, radio, Internet, printed press) are used to recruit adults aged 18 years and older from the general population. Apart from age, the inclusion criteria pertain to comprehension of written French and ability to follow an Internet-based protocol (https://etude-nutrinet-sante.fr/). NutriNet-Santé was approved by the Institutional Review Board of the French Institute for Health and Medical Research and by the National Commission on Informatics and Liberty. The cohort is registered (# NCT03335644) at https://www.ClinicalTrials.gov. Interested volunteers provide informed consent before enrolling in the cohort.
At inclusion and yearly thereafter, participants are asked to fill out a set of five questionnaires (described below) gathering data on socio-demographic and lifestyle characteristics, anthropometrics, physical activity, diet, and health status. In addition, participants are asked to complete one nutrition- or health-related questionnaire per month, as part of the follow-up.
Measures
Dietary data
Macronutrient intake was the main outcome in this analysis. In NutriNet-Santé, dietary intake is evaluated at baseline and every six months thereafter, each time using three non-consecutive 24-h dietary records. The dietary data collection tool has been validated against both dietitian interviews and various nutritional status biomarkers [26,27,28]. For each diet assessment day, participants were asked to report each food, beverage, and/or composite dish consumed, including the portion size/quantity, preparation method, and meal setting (place, time, etc.). Estimation of portion sizes is aided by validated photographs [29]. Next, NutriNet-Santé has its own food composition table that includes > 3500 items; it was used to estimate mean daily energy and nutrient intake [30]. All collected dietary data were weighted to respect the 5:7 and 2:7 ratios of weekdays and weekend days. For this analysis, each participant’s dietary macronutrient intake was averaged across a minimum of three 24-h dietary records completed over a 2.5-year window around the anxiety assessment date (described below); it was energy-adjusted using the residual method [31]. Individuals with aberrant daily energy values (< 500 kcal [32]), with fewer than three 24-h records and pregnant females at any of the dietary assessment points, were excluded from the analysis. Likewise, individuals with prevalent or incident diabetes mellitus (type 1 or type 2) were ineligible for this study due to potential dietary specificities, especially regarding the intake of carbohydrates.
The following outcome variables related to macronutrient intake were selected: percentage energy in the total diet from carbohydrates, protein and fat, respectively; mean total carbohydrates (g/day); mean complex carbohydrates (g/day); mean simple sugars (g/day); mean added sugars (g/day); mean total protein (g/day); mean animal protein (g/day); mean plant-based protein (g/day); mean total fat (g/day); mean saturated fatty acids (SFA) (g/day); mean monounsaturated fatty acids (MUFA) (g/day); mean polyunsaturated fatty acids (PUFA) (g/day); mean total cholesterol (mg/day); and mean total fiber (g/day).
Anxiety assessment
Anxiety was assessed during the period 2013–2016 by self-reports on the French version of the State-Trait Anxiety Inventory Form Y (STAI) which has been validated for use with general-population adults [33]. A total of 119,451 participants received the questionnaire, of whom 40,809 completed it once. STAI is one of the most widely used tools for the assessment of general anxiety proneness (as a state and as a trait), distinguishing it from depression [34]. State and trait anxiety are assessed by separate sets of 20 questions scored on a 4-point Likert scale from “Almost never” to “Almost always”; each set has its own psychometric evaluation. The higher the score, the greater the proneness to anxiety. Considering the objectives of this study and for purposes of consistency with prior research [14, 15], only the trait-anxiety subscale (STAI-T) was used for this analysis. It evaluates trait anxiety, characterized by a relatively stable tendency to exhibit tension and anxiety (i.e., state anxiety) in a variety of situations. Trait anxiety measured by the STAI-T has been highly correlated with the generalized anxiety disorder [35]. As in prior studies, and given the lack of an established cut-off value, participants were considered as having “high trait anxiety” if their total score was ≥ 40 points or as having “low trait anxiety” if their total score was < 40 points [14].
ED assessment
Screening for ED took place in 2014 via the validated self-administered 5-item SCOFF questionnaire [36, 37]. In total, 125,279 enrollees received the SCOFF, of whom 51,073 returned a completed questionnaire. Participants who did not complete the SCOFF in 2014 but did so in 2017 were also included in the study. Each of the five items is a Yes/No question, with two or more positive responses indicating a strong likelihood of ED; the score has been shown to approximate actual ED point prevalence [38]. Next, the Expali validated algorithmic tool, based on the SCOFF score and Body mass index (BMI, kg/m2), was used to identify four ED types: restrictive (RS; including AN, atypical AN, and restrictive food intake disorder), bulimic (BL; including bulimia nervosa and low-frequency/short-duration bulimia nervosa), hyperphagic (HP; including BED and low-frequency/short-duration BED), and other (not otherwise specified) ED [39].
Mental health status with regard to anxiety and ED
Mental health status (i.e., no disorder, pure or comorbid ED and anxiety) was the main exposure in this analysis. Participants were divided into ten groups by cross-tabulating their anxiety status (low or high) and their ED status (no disorder, RS, BL, HP, or other ED). Therefore, the following ten groups were modeled as the exposure: no disorder; pure anxiety; pure RS; anxiety + RS; pure BL; anxiety + BL; pure HP; anxiety + HP; other ED only; and anxiety + other ED.
Covariate data
A validated socio-demographic questionnaire was used to collect self-reported data on age, sex, educational level, socio-professional category, marital status, alcohol use, and smoking status [40]. The International Physical Activity Questionnaire assessed physical activity levels based on an established scoring protocol [41]. Self-reported height and weight data were collected using a validated anthropometrics questionnaire [42], which allowed the calculation of BMI and its main categories (underweight: < 18.5, normal weight: 18.5–24.9, overweight: 25.0–29.9, and obese: ≥ 30.0). As all of the above questionnaires are administered at baseline and annually thereafter; in the present analysis we used covariate data collected within a 2.5-year window around the STAI-T completion date.
Statistical analysis
Descriptive characteristics across mental health status reflect number (percent) from chi-squared tests (categorical variables) and mean (± SD) from ANOVA (continuous variables). The associations between mental health status (exposure) and macronutrient intake (outcome) were assessed using analyses of covariance (ANCOVA) adjusted for age (years, continuous scale), sex, alcohol consumption (g ethanol/day, continuous scale), smoking status (never, former, current smoker), physical activity level (low, moderate, high), educational level (less than high school, high school diploma or equivalent, college/undergraduate degree, graduate degree), socio-professional category (homemaker/disabled/unemployed, student, manual/blue collar worker, office work/administrative staff, professional/executive staff, retired), marital status (living alone or married/cohabiting), and number of 24-h dietary records (continuous scale). The underlying assumptions of the ANOVA/ANCOVA were checked and interpretation of the results was guided by published empirical evidence [43, 44]. Next, many-to-one comparisons applying the Dunnett-Hsu’s method (reference = no disorder) were performed. The main tests were two-sided and p < 0.050 was considered as evidence for statistical significance. SAS version 9.4 (SAS Institute, Inc., Cary NC, USA) was used for all statistical analyses.
Results
Description of sample
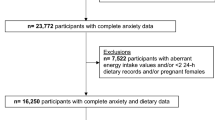
In total, 35,472 participants completed both the STAI-T and SCOFF questionnaires (n = 33,193 with SCOFF in 2014; n = 1559 with SCOFF in 2017). Among them, those with fewer than three 24-h dietary records, with aberrant energy intake values and/or pregnant females (n = 7222) were excluded from the analysis. Next, participants with diabetes mellitus (n = 1171) and those lacking complete covariate data (n = 2308) were also excluded. Thus, 24,771 participants were included in the analysis (Fig. 1) (74.0% female; mean age = 53.2 ± 13.7 years). Participants included in the analysis were generally older, more likely to be retired, to report higher levels of physical activity, and were less likely to be obese or current smokers compared to those who were excluded from the analysis (all p < 0.001; data not tabulated). The individuals in our sample were divided into ten groups according to their mental health status, as follows: no disorder n = 13,881; pure anxiety n = 7977; pure RS n = 55; anxiety + RS n = 152; pure BL n = 236; anxiety + BL n = 461; pure HP n = 631; anxiety + HP n = 974; other ED n = 181; and anxiety + other ED n = 223.
Descriptive characteristics across mental health status are presented in Table 1. In general, individuals with a mental health disorder (anxiety or ED) were more likely to be female, younger (except for HP and other ED), current smokers (except for HP), to live alone, and to consume less alcohol compared to those without a disorder (all p < 0.001). In the full sample, the mean number of 24-h dietary records was 8.8 ± 3.5. Overall, individuals with RS had the lowest caloric intake, which was 1595.1 (± 495.9) Kcal/day in the case of pure RS and 1438.7 (± 385.1) Kcal/day in the case of comorbid RS.
Association between mental health status and macronutrient intake
The main results in the form of least-squares (LS) means (standard error) are summarized in Table 2. Overall, ANCOVA revealed significant differences in mean intake across the ten groups for all macronutrients (p < 0.001) except for PUFA (p > 0.185). The detailed results from the main analysis are presented in Supplementary Figs. S1 to S16.
We observed that the anxiety + RS group had a significantly higher percentage of energy from carbohydrates (LS mean Δ = + 4.6%/day, p < 0.001), higher intakes of total carbohydrates (LS mean Δ = + 14.2 g/day, p < 0.001), simple sugars (LS mean Δ = + 12.9 g/day, p < 0.001), plant-based protein (LS mean Δ = + 3.1 g/day, p < 0.001), lower intakes of total fat (LS mean Δ = −6.6 g/day, p < 0.001), SFA (LS mean Δ = −3.6 g/day, p < 0.001), MUFA (LS mean Δ = −2.8 g/day, p < 0.001), and cholesterol (LS mean Δ = −46.8 mg/day, p < 0.001) in comparison with the “no disorder” group, whereas the results for the pure RS group were not significant. Both the pure RS and anxiety + RS groups had a significantly higher percentage of energy from protein (LS mean Δ = + 1.5%/day, p < 0.002; LS mean Δ = + 0.9%/day, p < 0.004, respectively), a lower percentage of energy from fat (LS mean Δ = −2.3%/day, p < 0.017; LS mean Δ = −5.3%/day, p < 0.001, respectively), and a higher intake of fiber (LS mean Δ = + 2.4 g/day, p < 0.008; LS mean Δ = + 4.9 g/day, p < 0.001, respectively) compared to the “no disorder” group.
The anxiety + BL group had a significantly higher percentage of energy from protein (LS mean Δ = + 0.7%/day, p < 0.001), a lower percentage of energy from fat (LS mean Δ = −0.8%/day, p < 0.020), and a higher intake of protein (LS mean Δ = + 1.9 g/day, p < 0.001) than the “no disorder” group, whereas the results for the pure BL were not significant. Both pure and comorbid BL had significantly higher intakes of plant-based protein (LS mean Δ = + 1.5 g/day, p < 0.001; LS mean Δ = + 0.9 g/day; p < 0.005, respectively), fiber (LS mean Δ = + 2.3 g/day; p < 0.001, LS mean Δ = + 1.4 g/day; p < 0.001, respectively), and a lower intake of SFA (LS mean Δ = −1.6 g/day, p < 0.003; LS mean Δ = −1.2 g/day, p < 0.001, respectively) compared to the “no disorder” group.
Next, the pure HP group had significantly lower intakes of added sugars (LS mean Δ = −2.0 g/day, p < 0.011), plant-based protein (LS mean Δ = −0.7 g/day, p < 0.013), and a higher intake of cholesterol (LS mean Δ = + 19.8 mg/day, p < 0.001) in comparison with the “no disorder” group. Both pure and comorbid HP were associated with significantly lower percentage of energy from carbohydrates (LS mean Δ = −1.3%/day, p < 0.001; LS mean Δ = −0.7%/day, p < 0.004, respectively), higher percentage of energy from protein (LS mean Δ = + 1.3%/day, p < 0.001; LS mean Δ = + 0.9%/day, p < 0.001, respectively), lower intakes of total carbohydrates (LS mean Δ = −6.0 g/day, p < 0.001; LS mean Δ = − 2.9 g/day, p < 0.002, respectively), simple sugars (LS mean Δ = −3.4 g/day, p < 0.001; LS mean Δ = −2.1 g/day, p < 0.030, respectively), higher intakes of total protein (LS mean Δ = + 4.3 g/day, p < 0.001; LS mean Δ = + 3.1 g/day, p < 0.001, respectively), and animal protein (LS mean Δ = + 5.0 g/day, p < 0.001; LS mean Δ = + 3.5 g/day, p < 0.001, respectively) compared to the “no disorder” group.
The anxiety + other ED group had a significantly higher intake of protein (LS mean Δ = + 2.7%/day, p < 0.006), whereas the results for the other ED group were not significant. Both pure and comorbid other ED had higher % protein (LS mean Δ = −0.7%/day, p < 0.020; LS mean Δ = −0.8%/day, p < 0.001, respectively), and higher intakes of animal protein (LS mean Δ = + 3.0 g/day, p < 0.031; LS mean Δ = + 3.3 g/day, p < 0.004, respectively) compared to the “no disorder” group.
Finally, the pure anxiety group had a significantly higher percentage of energy from carbohydrates (LS mean Δ = + 0.6%/day, p < 0.001), a lower percentage of energy from protein (LS mean Δ = −0.2%/day, p < 0.002), higher intakes of total carbohydrates (LS mean Δ = + 1.1 g/day, p < 0.033), complex carbohydrates (LS mean Δ = + 1.2 g/day, p < 0.003), added sugars (LS mean Δ = + 0.9 g/day, p < 0.001), lower intakes of protein (LS mean Δ = −0.5 g/day, p < 0.033), and fiber (LS mean Δ = −0.2 g/day, p < 0.014) compare to the “no disorder” group.
Discussion
This large population-based cross-sectional study revealed some significant differences in macronutrient intake according to mental health status regarding anxiety and ED. The observed differences largely depended on ED type.
Our main hypotheses that individuals with anxiety and/or ED would display different macronutrient intake compared to their counterparts without mental disorders and that unfavorable dietary intake (e.g., reduced diversity) would be more pronounced in the case of comorbidity were only partially supported. The strongest support for our hypotheses was found for RS. Generally, the difference in macronutrient intake between pure and comorbid forms seemed to be well pronounced in RS and much less pronounced in BL and other ED. Even though macronutrient intake exhibited similar trends across pure and comorbid ED, we observed a number of differences in terms of significance levels and absolute values in comparison with the “no disorder” group.
To our knowledge, this is the first epidemiological study investigating dietary intake across pure and comorbid anxiety-ED conditions among adults recruited from the general population. Prior research has reported that individuals with depression and anxiety, especially in the case of comorbidity, have a lower dietary quality than healthy controls [45]. Another previous study—based on a sample of 27,111 middle-aged male smokers—reported dietary intake according to the presence of pure or comorbid mental disorders [46]. These authors studied depression, anxiety, insomnia, and the comorbidity of all three disorders and did not find marked differences in micro- or macronutrient intake according to mental health status [46].
Several case–control studies have reported that compared to healthy controls, people with AN (i.e., the most common form of RS) were less likely to prefer/consume fat, animal protein, and were more likely to consume plant-based protein [17, 18] and vegetables [47, 48], which is consistent with the results of our study. We found that fiber intake was higher in both pure and comorbid RS, whereas the pure anxiety group had a significantly lower fiber intake in comparison with the “no disorder” group. It has been evoked that a high-fiber diet might be used by individuals suffering from AN to alleviate symptoms of gastroparesis [49]. In addition, the inverse association between dietary fiber intake and anxiety reported in some studies [50] might not be universal but rather dependent on sex and obesity status [51]. Moreover, we found that the restrictive eating behaviors and reduced dietary diversity that are typical of AN were more pronounced in comorbid than in pure RS. The lower intake of total fat, SFA, MUFA, and dietary cholesterol and the higher intake of plant-based protein observed only in the group with anxiety-RS comorbidity but not in pure RS group, suggested that dietary homogeneity (e.g., exclusion of red meat and meat products) is more pronounced in the case of comorbidity. A literature review reported that the more anxious individuals with AN were, the more likely they were to engage in restrictive eating behaviors to avoid weight gain [52]. Also, the observed higher intake of simple sugars, but not added sugars, among those with anxiety-RS comorbidity may reflect their preference for plant-based foods such as fruit (i.e., a source of fructose).
In our study, the highest intake of cholesterol was seen in those with pure HP; it was nearly 20 mg/day higher than that observed in the “no disorder” group. Findings based on a nationally-representative sample of U.S. adults indicated that among the three main ED types, only BED (i.e., the most common form of HP) was associated with high cholesterol intake [53], which is consistent with our results. Interestingly, unlike pure HP, cholesterol intake in the anxiety + HP group was not significantly different from that in the “no disorder” group. Likewise, the differences from the “no disorder” group in added sugar intake were −0.8 g/day (p > 0.618) and −2.0 g/day (p < 0.011) for comorbid and pure HP, respectively. These results suggest that comorbidity might not have a harmful impact on dietary intake among individuals suffering from HP. Research with obese females revealed that BED mediated the association between anxiety and caloric intake [54]. A community-based study also reported that anxiety status partly explained the variance of binge-eating symptoms, which suggested that anxiety might have a role in the development and maintenance of BED [24]. However, these authors indicated that binge-eating might attenuate anxiety symptoms [24], which could help explain the present findings. As regards BL, the fact that individuals could also present AN and BED-like behaviors [18] might obscure any substantial differences between the pure and comorbid forms.
In terms of potential psychosocial mechanisms of the observed associations, the results of network analyses have suggested that ED and anxiety (measured with STAI-T) might be linked through avoidance of social eating and low self-esteem [55]. It has also been shown that anxiety disorders were more closely linked with the severity of ED symptoms than were affective or substance-related disorders [56]. Regarding physiological mechanisms, there is a growing body of diet-mental health research exploring disruptions in circadian rhythm, gut-brain axis regulation, and hormonal homeostasis, leading to systemic and neuro-inflammation and oxidative stress [57, 58].
This study is subject to some limitations. First, the cross-sectional design does not allow for causal or chronological inference. Prior research has shown that dietary intake and mental health status can mutually impact each other [14, 15, 58, 59]. Future prospective research in this domain is needed to shed light not only on causality but also on the potential bidirectional association between macronutrient intake and comorbidity of anxiety and ED. Even though the present cross-sectional data did not permit the establishment of the chronological sequence of anxiety and ED onset, it appears that anxiety is more likely to precede ED than vice versa [60, 61]. Second, our study is based on trait anxiety which is regarded as a relatively stable personality characteristic. Even though trait anxiety and ED were assessed with validated tools, neither one could be considered as representing a clinical diagnosis. The proportion of participants with high anxiety proneness or with ED in our study was somewhat higher than the respective proportions reported by recent literature reviews [62, 63]. Yet, it should be kept in mind that these disorders are likely under-diagnosed in the general population [4, 5, 64]. Next, categorizing participants into ten groups according to their mental health status resulted in several groups with a relatively small number of individuals (e.g., pure RS: n = 55), which may have had an impact on the available statistical power. Further, in spite of the large number of covariates used for statistical adjustment, residual unmeasured confounding (e.g., ethnoracial status, family history of anxiety or ED) could not be excluded. Finally, as with any epidemiological cohort, NutriNet-Santé relies on voluntary participation, which might introduce selection bias and might limit generalizability, as it includes a higher proportion of females and individuals of higher socio-economic status compared to the respective proportions found in the general French population [65]. Likewise, dietary intake in the cohort exhibited some differences compared to that found in a representative sample of the French population [66].
Despite these limitations, the study presents several important strengths. To our knowledge, it is the first epidemiological study to reveal associations between comorbidity of anxiety-ED and macronutrient intake. All data were collected with validated questionnaires, using a very large and diverse sample of adults recruited from the general population. Moreover, macronutrient intakes were estimated based on a mean of nearly nine 24-h dietary records, validated against dietitian interviews and various biomarkers of nutritional status [26,27,28]. Given the high prevalence of mental comorbidity, the results of our study can be used for public health needs assessment. Our findings could help guide future epidemiological research, interventions, and policy development in the field of mental health, which is attracting attention in the Covid-19 pandemic context [67] yet is still far from being a public health priority [2].
Conclusions
This large population-based epidemiological study found some support for differences in macronutrient intake among individuals with pure or comorbid anxiety and ED and those without either disorder; these differences depended primarily on the ED type. Future prospective studies using clinically defined anxiety and ED featuring mediation and moderation analyses are needed to elucidate causality as well as potential effect modification of the observed associations.
Abbreviations
- AN:
-
Anorexia nervosa
- ANCOVA:
-
Analysis of covariance
- BED:
-
Binge-eating disorders
- BL:
-
Bulimic eating disorders
- BMI:
-
Body mass index
- ED:
-
Eating disorders
- HP:
-
Hyperphagic eating disorders
- LS mean:
-
Least-squares mean value
- MUFA:
-
Monounsaturated fatty acids
- PUFA:
-
Polyunsaturated fatty acids
- RS:
-
Restrictive eating disorders
- SFA:
-
Saturated fatty acids
- STAI-T:
-
Trait subscale of the State-Trait Anxiety Inventory
References
Rehm J, Shield KD (2019) Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep 21:10. https://doi.org/10.1007/s11920-019-0997-0
Saxena S, Kestel D, Sunkel C et al (2019) Countdown global mental health 2030. Lancet 393:858–859. https://doi.org/10.1016/S0140-6736(19)30424-6
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn (DSM-5). American Psychiatric Association, Washington, DC
Hilbert A (2019) Binge-eating disorder. Psychiatr Clin N Am 42:33–43. https://doi.org/10.1016/j.psc.2018.10.011
Keski-Rahkonen A, Mustelin L (2016) Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry 29:340–345. https://doi.org/10.1097/YCO.0000000000000278
Andreeva VA, Tavolacci M-P, Galan P et al (2019) Sociodemographic correlates of eating disorder subtypes among men and women in France, with a focus on age. J Epidemiol Commun Health 73:56–64. https://doi.org/10.1136/jech-2018-210745
Ng ISF, Cheung KCK, Chou K-L (2013) Correlates of eating disorder in middle-aged and older adults: evidence from 2007 British National Psychiatric Morbidity Survey. J Aging Health 25:1106–1120. https://doi.org/10.1177/0898264313494798
Swinbourne JM, Touyz SW (2007) The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev J Eat Disord Assoc 15:253–274. https://doi.org/10.1002/erv.784
Valderas JM, Starfield B, Sibbald B et al (2009) Defining comorbidity: implications for understanding health and health services. Ann Fam Med 7:357–363. https://doi.org/10.1370/afm.983
Watson HJ, Swan A, Nathan PR (2011) Psychiatric diagnosis and quality of life: the additional burden of psychiatric comorbidity. Compr Psychiatry 52:265–272. https://doi.org/10.1016/j.comppsych.2010.07.006
Elran-Barak R, Goldschmidt AB (2021) Differences in severity of eating disorder symptoms between adults with depression and adults with anxiety. Eat Weight Disord EWD 26:1409–1416. https://doi.org/10.1007/s40519-020-00947-y
Lydecker JA, Grilo CM (2021) Psychiatric comorbidity as predictor and moderator of binge-eating disorder treatment outcomes: an analysis of aggregated randomized controlled trials. Psychol Med. https://doi.org/10.1017/S0033291721001045
Keshishian AC, Tabri N, Becker KR et al (2019) Eating disorder recovery is associated with absence of major depressive disorder and substance use disorders at 22-year longitudinal follow-up. Compr Psychiatry 90:49–51. https://doi.org/10.1016/j.comppsych.2019.01.002
Kose J, Cheung A, Fezeu LK et al (2021) A comparison of sugar intake between individuals with high and low trait anxiety: results from the Nutrinet-Santé study. Nutrients 13:1526. https://doi.org/10.3390/nu13051526
Kose J, Fezeu LK, Touvier M et al (2021) Dietary macronutrient intake according to sex and trait anxiety level among non-diabetic adults: a cross-sectional study. Nutr J 20:78. https://doi.org/10.1186/s12937-021-00733-1
Kris-Etherton PM, Petersen KS, Hibbeln JR et al (2021) Nutrition and behavioral health disorders: depression and anxiety. Nutr Rev 79:247–260. https://doi.org/10.1093/nutrit/nuaa025
Schebendach JE, Uniacke B, Walsh BT et al (2019) Fat preference and fat intake in individuals with and without anorexia nervosa. Appetite 139:35–41. https://doi.org/10.1016/j.appet.2019.04.008
Segura-García C, De Fazio P, Sinopoli F et al (2014) Food choice in disorders of eating behavior: correlations with the psychopathological aspects of the diseases. Compr Psychiatry 55:1203–1211. https://doi.org/10.1016/j.comppsych.2014.02.013
Bragg MA, White MA (2013) Examining the relationship between soda consumption and eating disorder pathology. Adv Eat Disord Abingdon U K Print 1:10. https://doi.org/10.1080/21662630.2013.742317
Goodman EL, Breithaupt L, Watson HJ et al (2018) Sweet taste preference in binge-eating disorder: a preliminary investigation. Eat Behav 28:8–15. https://doi.org/10.1016/j.eatbeh.2017.11.005
Keck MM, Vivier H, Cassisi JE et al (2020) Examining the role of anxiety and depression in dietary choices among college students. Nutrients 12:2061. https://doi.org/10.3390/nu12072061
Christian CB, Ngo BK, Brosof LC, Levinson CA (2021) Social appearance anxiety moderates the relationship between thin-ideal internalization and eating disorder symptoms cross-sectionally and prospectively in adolescent girls. Eat Weight Disord EWD 26:2065–2070. https://doi.org/10.1007/s40519-020-01050-y
Lim MC, Parsons S, Goglio A, Fox E (2021) Anxiety, stress, and binge eating tendencies in adolescence: a prospective approach. J Eat Disord 9:94. https://doi.org/10.1186/s40337-021-00444-2
Rosenbaum DL, White KS (2015) The relation of anxiety, depression, and stress to binge eating behavior. J Health Psychol 20:887–898. https://doi.org/10.1177/1359105315580212
Hercberg S, Castetbon K, Czernichow S et al (2010) The Nutrinet-Santé study: a web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health 10:242. https://doi.org/10.1186/1471-2458-10-242
Lassale C, Castetbon K, Laporte F et al (2015) Validation of a web-based, self-administered, non-consecutive-day dietary record tool against urinary biomarkers. Br J Nutr 113:953–962. https://doi.org/10.1017/S0007114515000057
Lassale C, Castetbon K, Laporte F et al (2016) Correlations between fruit, vegetables, fish, vitamins, and fatty acids estimated by web-based nonconsecutive dietary records and respective biomarkers of nutritional status. J Acad Nutr Diet 116:427-438.e5. https://doi.org/10.1016/j.jand.2015.09.017
Touvier M, Kesse-Guyot E, Méjean C et al (2011) Comparison between an interactive web-based self-administered 24 h dietary record and an interview by a dietitian for large-scale epidemiological studies. Br J Nutr 105:1055–1064. https://doi.org/10.1017/S0007114510004617
Le Moullec N, Deheeger M, Preziosi P (1996) Validation du manuel-photos utilisé pour l’enquête alimentaire de l’étude SU. VI. MAX [Validation of the photo manual used for the food survey of the SU. VI. MAX study]. Cah Nutr Diét 31:158–164
Etude NutriNet-Santé (2013) Table de composition des aliments (Food composition table). Économica, Paris
Willett W (2012) Nutritional epidemiology. Oxford University Press, Oxford
Raatz SK, Jahns L, Johnson LK et al (2015) Nutritional adequacy of dietary intake in women with anorexia nervosa. Nutrients 7:3652–3665. https://doi.org/10.3390/nu7053652
Langevin V, Boini S, François M, Riou A (2012) Inventaire d’anxiété état-trait forme Y (State-Trait Anxiety Inventory (STAI-Y)). Réf En Santé Au Trav 131:161–164
Spielberger C, Gorsuch R, Lushene R et al (1983) Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press, Palo Alto
Chambers JA, Power KG, Durham RC (2004) The relationship between trait vulnerability and anxiety and depressive diagnoses at long-term follow-up of Generalized Anxiety Disorder. J Anxiety Disord 18:587–607. https://doi.org/10.1016/j.janxdis.2003.09.001
Garcia FD, Grigioni S, Allais E et al (2011) Detection of eating disorders in patients: validity and reliability of the French version of the SCOFF questionnaire. Clin Nutr 30:178–181. https://doi.org/10.1016/j.clnu.2010.09.007
Morgan JF, Reid F, Lacey JH (1999) The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 319:1467–1468. https://doi.org/10.1136/bmj.319.7223.1467
Botella J, Sepúlveda AR, Huang H, Gambara H (2013) A meta-analysis of the diagnostic accuracy of the SCOFF. Span J Psychol 16:E92. https://doi.org/10.1017/sjp.2013.92
Tavolacci M-P, Gillibert A, Zhu Soubise A et al (2019) Screening four broad categories of eating disorders: suitability of a clinical algorithm adapted from the SCOFF questionnaire. BMC Psychiatry 19:366. https://doi.org/10.1186/s12888-019-2338-6
Vergnaud AC, Touvier M, Méjean C et al (2011) Agreement between web-based and paper versions of a socio-demographic questionnaire in the NutriNet-Santé study. Int J Public Health 56:407–417. https://doi.org/10.1007/s00038-011-0257-5
Craig CL, Marshall AL, Sjöström M et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB
Lassale C, Péneau S, Touvier M et al (2013) Validity of web-based self-reported weight and height: results of the Nutrinet-Santé study. J Med Internet Res 15:e152. https://doi.org/10.2196/jmir.2575
Blanca MJ, Alarcón R, Arnau J (2017) Non-normal data: is ANOVA still a valid option? Psicothema. https://doi.org/10.7334/psicothema2016.383
Blanca MJ, Alarcón R, Arnau J et al (2018) Effect of variance ratio on ANOVA robustness: might 1.5 be the limit? Behav Res Methods 50:937–962. https://doi.org/10.3758/s13428-017-0918-2
Gibson-Smith D, Bot M, Brouwer IA et al (2018) Diet quality in persons with and without depressive and anxiety disorders. J Psychiatr Res 106:1–7. https://doi.org/10.1016/j.jpsychires.2018.09.006
Hakkarainen R, Partonen T, Haukka J et al (2004) Food and nutrient intake in relation to mental wellbeing. Nutr J 3:14. https://doi.org/10.1186/1475-2891-3-14
Jáuregui Lobera I (2009) Choice of diet in patients with anorexia nervosa. Nutr Hosp. https://doi.org/10.3305/nh.2009.24.6.4552
Misra M, Tsai P, Anderson EJ et al (2006) Nutrient intake in community-dwelling adolescent girls with anorexia nervosa and in healthy adolescents. Am J Clin Nutr 84:698–706
Mehler PS, Brown C (2015) Anorexia nervosa—medical complications. J Eat Disord 3:11. https://doi.org/10.1186/s40337-015-0040-8
Taylor AM, Holscher HD (2020) A review of dietary and microbial connections to depression, anxiety, and stress. Nutr Neurosci 23:237–250. https://doi.org/10.1080/1028415X.2018.1493808
Saghafian F, Sharif N, Saneei P et al (2021) Consumption of dietary fiber in relation to psychological disorders in adults. Front Psychiatry 12:587468. https://doi.org/10.3389/fpsyt.2021.587468
Lloyd EC, Haase AM, Foster CE, Verplanken B (2019) A systematic review of studies probing longitudinal associations between anxiety and anorexia nervosa. Psychiatry Res 276:175–185. https://doi.org/10.1016/j.psychres.2019.05.010
Udo T, Grilo CM (2019) Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. Int J Eat Disord 52:42–50. https://doi.org/10.1002/eat.23004
Peterson RE, Latendresse SJ, Bartholome LT et al (2012) Binge eating disorder mediates links between symptoms of depression, anxiety, and caloric intake in overweight and obese women. J Obes 2012:407103. https://doi.org/10.1155/2012/407103
Forrest LN, Sarfan LD, Ortiz SN et al (2019) Bridging eating disorder symptoms and trait anxiety in patients with eating disorders: a network approach. Int J Eat Disord 52:701–711. https://doi.org/10.1002/eat.23070
Spindler A, Milos G (2007) Links between eating disorder symptom severity and psychiatric comorbidity. Eat Behav 8:364–373. https://doi.org/10.1016/j.eatbeh.2006.11.012
Godos J, Currenti W, Angelino D et al (2020) Diet and mental health: review of the recent updates on molecular mechanisms. Antioxid Basel Switz 9:E346. https://doi.org/10.3390/antiox9040346
Murphy M, Mercer JG (2013) Diet-regulated anxiety. Int J Endocrinol 2013:701967. https://doi.org/10.1155/2013/701967
Mörkl S, Wagner-Skacel J, Lahousen T et al (2020) The role of nutrition and the gut-brain axis in psychiatry: a review of the literature. Neuropsychobiology 79:80–88. https://doi.org/10.1159/000492834
Kaye WH, Bulik CM, Thornton L et al (2004) Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry 161:2215–2221. https://doi.org/10.1176/appi.ajp.161.12.2215
Swinbourne J, Hunt C, Abbott M et al (2012) The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatry 46:118–131. https://doi.org/10.1177/0004867411432071
Galmiche M, Déchelotte P, Lambert G, Tavolacci MP (2019) Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr 109:1402–1413. https://doi.org/10.1093/ajcn/nqy342
Remes O, Brayne C, van der Linde R, Lafortune L (2016) A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav 6:e00497. https://doi.org/10.1002/brb3.497
DeMartini J, Patel G, Fancher TL (2019) Generalized anxiety disorder. Ann Intern Med 170:ITC49–ITC64. https://doi.org/10.7326/AITC201904020
Andreeva VA, Salanave B, Castetbon K et al (2015) Comparison of the sociodemographic characteristics of the large NutriNet-Santé e-cohort with French census data: the issue of volunteer bias revisited. J Epidemiol Commun Health 69:893–898. https://doi.org/10.1136/jech-2014-205263
Andreeva VA, Deschamps V, Salanave B et al (2016) Comparison of dietary intakes between a large online cohort study (Etude NutriNet-Santé) and a nationally representative cross-sectional study (Etude Nationale Nutrition Santé) in France: addressing the issue of generalizability in e-epidemiology. Am J Epidemiol 184:660–669. https://doi.org/10.1093/aje/kww016
Gloster AT, Lamnisos D, Lubenko J et al (2020) Impact of COVID-19 pandemic on mental health: an international study. PLoS ONE 15:e0244809. https://doi.org/10.1371/journal.pone.0244809
Acknowledgements
The authors thank Prof. Pierre Déchelotte and Dr. Françoise Radat for their respective involvement in the assessment of eating disorders and general anxiety in the NutriNet-Santé cohort, and Dr. Marie-Pierre Tavolacci for providing the Expali algorithmic tool. The authors also thank Cédric Agaesse (dietary data manager), Alexandre De-Sa and Rebecca Lutchia (dietitians); Younes Esseddik (IT manager), Thi Hong Van Duong, Régis Gatibelza, Jagatjit Mohinder and Aladi Timera (computer scientists); Julien Allegre, Nathalie Arnault, Laurent Bourhis, Nicolas Dechamp (biostatisticians), and Fabien Szabo de Edelenyi, Ph.D. (biostatistics team manager); Maria Gomes (NutriNet-Santé participant support) and Nathalie Druesne-Pecollo, Ph.D. (operations coordinator) for their technical contribution to the cohort. Finally, the authors thank all the volunteers of the NutriNet-Santé cohort.
Funding
The NutriNet-Santé study is supported by the French Ministry of Solidarity and Health, the National Agency for Public Health (Santé Publique France), the National Institute for Health and Medical Research (INSERM), the National Research Institute for Agriculture, Food and Environment (INRAE), the National Conservatory of Arts and Crafts (CNAM), the Center for Epidemiological Research and Statistics (CRESS) and Sorbonne Paris Nord University. Junko Kose is funded by a doctoral fellowship provided by the French Ministry of Education via Sorbonne Paris Nord University. Indira Paz Graniel is supported by a doctoral grant from the Spanish Ministry of Universities (# EST19/00261). The funders had no role in the design of the study; in the collection, analysis, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Author information
Authors and Affiliations
Contributions
SH, PG, and MT designed and implemented the NutriNet-Santé cohort study; PG and VAA implemented the STAI questionnaire and coordinated anxiety data collection; SP and VAA implemented the SCOFF questionnaire and coordinated eating disorder data collection; VAA conceptualized the study, designed the analytic strategy, and provided theoretical and empirical guidance; JK performed the literature review, statistical analyses and led the writing; all authors assisted with interpretation of the data, critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript and its submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The NutriNet-Santé study is conducted according to the Declaration of Helsinki guidelines. It was approved by the Institutional Review Board of the French Institute for Health and Medical Research (INSERM # 00000388FWA00005831) and by the National Commission on Informatics and Liberty (CNIL # 908450 and # 909216). NutriNet-Santé is registered (# NCT03335644) at http://www.ClinicalTrials.gov. Electronic informed consent was obtained from all individuals prior to inclusion in the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kose, J., Paz Graniel, I., Péneau, S. et al. A population-based study of macronutrient intake according to mental health status with a focus on pure and comorbid anxiety and eating disorders. Eur J Nutr 61, 3685–3696 (2022). https://doi.org/10.1007/s00394-022-02923-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02923-x