Abstract
Purpose
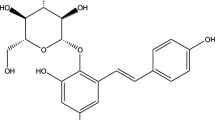
Glycyrrhizin (GL) and its metabolites 18α-glycyrrhetinic acid (18α-GA) and 18β-glycyrrhetinic acid (18β-GA) are used as traditional medicine and food sweeteners. As the major rout of their administration is oral way, therefore their impact on intestinal epithelial cells are investigated.
Methods
The effects of GL and its metabolites on cell viability using MTT assay, on cytotoxicity using LDH release, on integrity of intestinal epithelial cells by measuring the transepithelial electrical resistance (TEER) and Luciferase permeability tests, on the expression of tight junction proteins at mRNA and protein level by qPCR and western blot techniques, and ultimately on the rate of test compounds absorption via Caco-2 cells monolayer were investigated.
Results
MTT assay showed a concentration- and time-dependent decrease in metabolic activity of Caco-2 cells induced by GL, 18α-GA, and 18β-GA, while only 18β-GA increased the LDH leakage. The monolayer integrity of Caco-2 cells in TEER assay only was affected by 18β-GA. The permeability of paracellular transport marker was increased by 18α-GA and 18β-GA and not GL. In transport studies, only metabolites were able to cross from Caco-2 cells monolayer. qPCR analyses revealed that 18β-GA upregulated the expression of claudin-1 and -4, occludin, junctional adhesion molecules and zonula occludens-1, while 18α-GA upregulated only claudin-4. The expression of claudin-4 at protein level was downregulated non-significantly at 50 μM concentration of 18β-GA.
Conclusion
Our results suggest that 18β-GA may cause cellular damages at higher concentrations on gastrointestinal cells and requires a remarkable attention of the nutraceutical and pharmaceutical industries.






Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Change history
21 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00394-023-03114-y
References
Kim DH, Hong SW, Kim BT, Bae EA, Park HY, Han MJ (2000) Biotransformation of glycyrrhizin by human intestinal bacteria and its relation to biological activities. Arch Pharm Res 23:172–177. https://doi.org/10.1007/BF02975509
Scientific Committee on Food (2003) Opinion of the Scientific Committee on Food on Glycyrrhizinic Acid and its Ammonium Salt. Brussel- Belgium-Office: G-1 01/242.
Pastorino G, Cornara L, Soares S, Rodrigues F, Oliveira MB (2018) Liquorice (Glycyrrhiza glabra): a phytochemical and pharmacological review. Phytother Res 32:2323–2239. https://doi.org/10.1002/ptr.6178
Li H, Guo D, Zhang L, Feng X (2018) Glycyrrhizin attenuates histamine-mediated MUC5AC upregulation, inflammatory cytokine production, and aquaporin 5 downregulation through suppressing the NF-κB pathway in human nasal epithelial cells. Chem Biol Interact 285:21–26. https://doi.org/10.1016/j.cbi.2018.02.010
Fiore C, Eisenhut M, Krausse R, Ragazzi E, Pellati D, Armanini D, Bielenberg J (2008) Antiviral effects of Glycyrrhiza species. J Phytother Res 22:141–148. https://doi.org/10.1002/ptr.2295
Hoever G, Baltina L, Michaelis M, Kondratenko R, Baltina L, Tolstikov GA, Doerr HW, Cinatl J Jr (2005) Antiviral activity of glycyrrhizic acid derivatives against SARS-coronavirus. J Med Chem 48:1256–1259. https://doi.org/10.1021/jm0493008
Bordbar N, Karimi MH, Amirghofran Z (2012) The effect of glycyrrhizin on maturation and T cell stimulating activity of dendritic cells. Cell Imanol. 280:44–49. https://doi.org/10.1016/j.cellimm.2012.11.013
Adianti M, Aoki C, Komoto M, Deng L, Shoji I, Wahyuni TS, Lusida MI, Soetjipto K, Fuchino H, Kawahara N, Hotta H (2014) Anti-hepatitis C virus compounds obtained from Glycyrrhiza uralensis and other Glycyrrhiza species. Microbiol Immunol 58:180–187. https://doi.org/10.1111/1348-0421.12127
Feng J-H, Chen W, Zhao Y, Ju X-L (2009) Anti-tumor activity of oleanolic, ursolic and glycyrrhetinic acid. Open Nat Prod J 2:48–52. https://doi.org/10.2174/1874848100902010048
Schiller PC, D’Ippolito G, Brambilla R, Roos BA, Howard GA (2001) Inhibition of gap-junctional communication induces the trans-differentiation of osteoblasts to an adipocytic phenotype in vitro. J Biol Chem 276:14133–21413. https://doi.org/10.1074/jbc.M011055200
Ruiz-Meana M, Garcia-Dorado D, Lane S, Pina P, Inserte J, Mirabet M, Soler-Soler J (2001) Persistence of gap junction communication during myocardial ischemia. Am J Physiol Heart Circ Physiol 280:H2563–H2571. https://doi.org/10.1152/ajpheart.2001.280.6.H2563
Chung TH, Wang SM, Chang YC, Chen YL, Wu JC (2007) 18beta-glycyrrhetinic acid promotes src interaction with connexin43 in rat cardiomyocytes. J Cell Biochem 100:653–664. https://doi.org/10.1002/jcb.21018
Huang SH, Wu JC, Hwang RD, Yeo HL, Wang SM (2003) Effects of 18β-glycyrrhetinic acid on the junctional complex and steroidogenesis in rat adrenocortical cells. J cell biochem 90:33–41. https://doi.org/10.1002/jcb.10610
Falet JP, Elkrief A, Green L (2019) Hypertensive emergency induced by licorice tea. CMAJ 191:E581-e583. https://doi.org/10.1503/cmaj.180550
Lobner D (2000) Comparison of the LDH and MTT assays for quantifying cell death: validity for neuronal apoptosis? J Neurosci Methods 96:147–152. https://doi.org/10.1016/s0165-0270(99)00193-4 (PMID: 10720679)
Kim DH, Lee SW, Han MJ (1999) Biotransformation of glycyrrhizin to 18beta-glycyrrhetinic acid-3-O-beta-D-glucuronide by Streptococcus LJ-22, a human intestinal bacterium. Biol Pharm Bull 22:320–322. https://doi.org/10.1248/bpb.22.320
Lichtman SM (2001) Bacterial [correction of baterial] translocation in human’s. J Pediatr Gastroenterol Nutr 33:1–10. https://doi.org/10.1097/00005176-200107000-00001
Sharma S, Tripathi P, Sharma J, Dixit A (2020) Flavonoids modulate tight junction barrier functions in hyperglycemic human intestinal Caco-2 cells. Nutrition (Burbank, Los Angeles County, Calif.) 78:110792. https://doi.org/10.1016/j.nut.2020.110792
Shao Y, Wolf PG, Guo S, Guo Y, Gaskins HR, Zhang B (2017) Zinc enhances intestinal epithelial barrier function through the PI3K/AKT/mTOR signaling pathway in Caco-2 cells. J nutr Biochem 43:18–26. https://doi.org/10.1016/j.jnutbio.2017.01.013
Akbari P, Braber S, Varasteh S, Alizadeh A, Garssen J, Fink-Gremmels J (2017) The intestinal barrier as an emerging target in the toxicological assessment of mycotoxins. Arch Toxicol 91:1007–1029. https://doi.org/10.1007/s00204-016-1794-8
Vogel C, Abreu Rde S, Ko D, Le SY, Shapiro BA, Burns SC, Sandhu D, Boutz DR, Marcotte EM, Penalva LO (2010) Sequence signatures and mRNA concentration can explain two-thirds of protein abundance variation in a human cell line. Mol Syst Boil 6:400. https://doi.org/10.1038/msb.2010.59
Akbari P, Braber S, Gremmels H, Koelink PJ, Verheijden KA, Garssen J, Fink-Gremmels J (2014) Deoxynivalenol: a trigger for intestinal integrity breakdown. FASEB J 28(2414–2429):10. https://doi.org/10.1096/fj.13-238717
Shil A, Olusanya O, Ghufoor Z, Forson B, Marks J (2020) Artificial sweeteners disrupt tight junctions and barrier function in the intestinal epithelium through activation of the sweet taste receptor, T1R3. Nutrients 12(6):1862. https://doi.org/10.3390/nu12061862
Wang XX, Liu GY, Yang YF, Wu XW, Xu W, Yang XW (2017) Intestinal absorption of triterpenoids and flavonoids from glycyrrhizae radix et rhizoma in the human Caco-2 monolayer cell Model. Molecules (Basel, Switzerland) 22(10):1627. https://doi.org/10.3390/molecules22101627
Acknowledgements
The authors would like to thank Professor Johanna Fink-Gremmels and Dr. Peyman Akbari from Utrecht University, for their constructive comments.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MM carried out the experiments and wrote the first draft of the manuscript. MRP designed the study and participated in data collection and analyses. HM carried out experiments, participated in the statistical analyses and in the drafting of manuscript and discussed the results. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.

Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Malekinejad, M., Pashaee, M.R. & Malekinejad, H. 18β-Glycyrrhetinic acid altered the intestinal permeability in the human Caco-2 monolayer cell model. Eur J Nutr 61, 3437–3447 (2022). https://doi.org/10.1007/s00394-022-02900-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02900-4