Abstract
Purpose
The objective of the study was to evaluate the anti-obesity effect of Lactobacillus rhamnosus LS-8 and Lactobacillus crustorum MN047, and illustrate the potential functional mechanism about the alleviation of high fat and high fructose diet (HFFD) induced obesity and related metabolic abnormalities.
Methods
C57BL/6J mice were subjected to a standard or HFFD with or without supplementation of L. rhamnosus LS-8 and L. crustorum MN047 for 10 weeks. Obesity related metabolic indices including glucose tolerance, insulin resistance, serum lipid, liver function, hormones and inflammatory cytokines were assessed by standard protocols. For the monitoring of inflammatory response and lipid metabolism, transcriptional levels were profiled in liver and/or adipose tissues. Furthermore, gut microbiota composition analyses in the fecal samples were performed using 16S rRNA gene sequencing, and gut microbial metabolites, including lipopolysaccharide (LPS) and short-chain fatty acids (SCFAs), were also tested for the assessment of the relationship between gut microbiota variation and inflammatory response.
Results
Administration with L. rhamnosus LS-8 and L. crustorum MN047 significantly mitigated body weight gain and insulin resistance, and inflammatory response (TNF-α, IL-1β and IL-6 levels in serum and corresponding mRNA levels in adipose tissues) was significantly inhibited in these two strains-treated mice. Moreover, L. rhamnosus LS-8 and L. crustorum MN047 could partially normalized mRNA expression levels involved in lipid metabolism including Pparγ, Srebp-1c, CD36, Fabp2 and FAS. In addition, these two strains manipulated gut microbiota by decreasing the abundance of Bacteroides and Desulfovibrio and increasing that of Lactobacillus and Bifidobacterium, which in turn raised the levels of feces SCFAs and lowered the levels of circulating LPS.
Conclusion
These results indicated that L. rhamnosus LS-8 and L. crustorum MN047 supplementation possessed the anti-obesity effect on the HFFD fed mice by alleviating inflammatory response and regulating gut microbiota, which further suggested that these two probiotics can be considered as an alternative dietary supplement in combination with the preventive and therapeutic strategies against obesity and related complications.
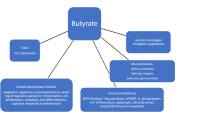
Graphic abstract








Similar content being viewed by others
References
Shang H, Sun J, Chen YQ (2016) Clostridium Butyricum CGMCC0313.1 modulates lipid profile, insulin resistance and colon homeostasis in obese mice. PLoS One 11(4):e0154373. https://doi.org/10.1371/journal.pone.0154373
Li X, Xu Q, Jiang T, Fang S, Wang G, Zhao J, Zhang H, Chen W (2016) A comparative study of the antidiabetic effects exerted by live and dead multi-strain probiotics in the type 2 diabetes model of mice. Food Funct 7(12):4851–4860. https://doi.org/10.1039/C6FO01147K
Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB (2010) Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. Diabetes Care 33(11):2477–2483. https://doi.org/10.2337/dc10-1079
Pan Y-Y, Zeng F, Guo W-L, Li T-T, Jia R-B, Huang Z-R, Lv X-C, Zhang J, Liu B (2018) Effect of Grifola frondosa 95% ethanol extract on lipid metabolism and gut microbiota composition in high-fat diet-fed rats. Food Funct. https://doi.org/10.1039/C8FO01116H
Kang JG, Park C-Y (2012) Anti-obesity drugs: a review about their effects and safety. Diabetes Metab J 36(1):13–25. https://doi.org/10.4093/dmj.2012.36.1.13
Xu HY, Barnes GT, Yang Q, Tan Q, Yang DS, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Investig 112(12):1821–1830. https://doi.org/10.1172/jci200319451
Shoelson SE, Herrero L, Naaz A (2007) Obesity, inflammation, and insulin resistance. Gastroenterology 132(6):2169–2180. https://doi.org/10.1053/j.gastro.2007.03.059
Saltiel AR, Olefsky JM (2017) Inflammatory mechanisms linking obesity and metabolic disease. J Clin Investig 127(1):1–4. https://doi.org/10.1172/jci92035
Oh DY, Morinaga H, Talukdar S, Bae EJ, Olefsky JM (2012) Increased macrophage migration into adipose tissue in obese mice. Diabetes 61(2):346–354. https://doi.org/10.2337/db11-0860
Roselli M, Finamore A, Brasili E, Rami R, Nobili F, Orsi C, Zambrini AV, Mengheri E (2018) Beneficial effects of a selected probiotic mixture administered to high fat-fed mice before and after the development of obesity. J Funct Foods 45:321–329. https://doi.org/10.1016/j.jff.2018.03.039
Hsieh FC, Lan CC, Huang TY, Chen KW, Chai CY, Chen WT, Fang AH, Chen YH, Wu CS (2016) Heat-killed and live Lactobacillus reuteri GMNL-263 exhibit similar effects on improving metabolic functions in high-fat diet-induced obese rats. Food Funct 7(5):2374–2388. https://doi.org/10.1039/c5fo01396h
Kamei N, Tobe K, Suzuki R, Ohsugi M, Watanabe T, Kubota N, Ohtsuka-Kowatari N, Kumagai K, Sakamoto K, Kobayashi M, Yamauchi T, Ueki K, Oishi Y, Nishimura S, Manabe I, Hashimoto H, Ohnishi Y, Ogata H, Tokuyama K, Tsunoda M, Ide T, Murakami K, Nagai R, Kadowaki T (2006) Overexpression of monocyte chemoattractant protein-1 in adipose tissues causes macrophage recruitment and insulin resistance. J Biol Chem 281(36):26602–26614. https://doi.org/10.1074/jbc.M601284200
Bianconi V, Sahebkar A, Atkin SL, Pirro M (2018) The regulation and importance of monocyte chemoattractant protein-1. Curr Opin Hematol 25(1):44–51. https://doi.org/10.1097/moh.0000000000000389
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, Biddinger SB, Dutton RJ, Turnbaugh PJ (2014) Diet rapidly and reproducibly alters the human gut microbiome. Nature 505(7484):559. https://doi.org/10.1038/nature12820
Martinez-Guryn K, Hubert N, Frazier K, Urlass S, Musch MW, Ojeda P, Pierre JF, Miyoshi J, Sontag TJ, Cham CM, Reardon CA, Leone V, Chang EB (2018) Small intestine microbiota regulate host digestive and absorptive adaptive responses to dietary lipids. Cell Host Microbe 23(4):458. https://doi.org/10.1016/j.chom.2018.03.011
Nicholson JK, Holmes E, Kinross J, Burcelin R, Gibson G, Jia W, Pettersson S (2012) Host-gut microbiota metabolic interactions. Science 336(6086):1262–1267. https://doi.org/10.1126/science.1223813
Engevik MA, Versalovic J (2017) Biochemical features of beneficial microbes: foundations for therapeutic microbiology. Microbiol Spectr 5(5):35. https://doi.org/10.1128/microbiolspec.BAD-0012-2016
Delzenne NM, Cani PD (2011) Interaction between obesity and the gut microbiota: relevance in nutrition. In: Cousins RJ, Bier DM, Bowman BA (eds) Annual review of nutrition, vol 31. Annual Reviews, Palo Alto, pp 15–31. https://doi.org/10.1146/annurev-nutr-072610-145146
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Waget A, Delmee E, Cousin B, Sulpice T, Chamontin B, Ferrieres J, Tanti JF, Gibson GR, Casteilla L, Delzenne NM, Alessi MC, Burcelin R (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56(7):1761–1772. https://doi.org/10.2337/db06-1491
Mei XR, Zhang XY, Wang ZG, Gao ZY, Liu G, Hu HL, Zou L, Li XL (2016) Insulin sensitivity-enhancing activity of phlorizin is associated with lipopolysaccharide decrease and gut microbiota changes in obese and type 2 diabetes (db/db) mice. J Agric Food Chem 64(40):7502–7511. https://doi.org/10.1021/acs.jafc.6b03474
Kadooka Y, Sato M, Imaizumi K, Ogawa A, Ikuyama K, Akai Y, Okano M, Kagoshima M, Tsuchida T (2010) Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Eur J Clin Nutr 64(6):636–643. https://doi.org/10.1038/ejcn.2010.19
Park DY, Ahn YT, Park SH, Huh CS, Yoo SR, Yu R, Sung MK, McGregor RA, Choi MS (2013) Supplementation of Lactobacillus curvatus HY7601 and Lactobacillus plantarum KY1032 in diet-induced obese mice is associated with gut microbial changes and reduction in obesity. PLoS One. https://doi.org/10.1371/journal.pone.0059470
Kim B, Park KY, Ji Y, Park S, Holzapfel W, Hyun CK (2016) Protective effects of Lactobacillus rhamnosus GG against dyslipidemia in high-fat diet-induced obese mice. Biochem Biophys Res Commun 473(2):530–536. https://doi.org/10.1016/j.bbrc.2016.03.107
Zhang LH, Wang L, Yi LH, Wang X, Zhang Y, Liu JY, Guo X, Liu L, Shao CE, Lu X (2017) A novel antimicrobial substance produced by Lactobacillus rhamnous LS-8. Food Control 73:754–760. https://doi.org/10.1016/j.foodcont.2016.09.028
Yi L, Luo L, Lü X (2018) Efficient exploitation of multiple novel bacteriocins by combination of complete genome and peptidome. Front Microbiol 9:1567. https://doi.org/10.3389/fmicb.2018.01567
Balakumar M, Prabhu D, Sathishkumar C, Prabu P, Rokana N, Kumar R, Raghavan S, Soundarajan A, Grover S, Batish VK, Mohan V, Balasubramanyam M (2018) Improvement in glucose tolerance and insulin sensitivity by probiotic strains of Indian gut origin in high-fat diet-fed C57BL/6J mice. Eur J Nutr 57(1):279–295. https://doi.org/10.1007/s00394-016-1317-7
Haffner SM, Greenberg AS, Weston WM, Chen HZ, Williams K, Freed MI (2002) Effect of rosiglitazone treatment on nontraditional markers of cardiovascular disease in patients with type 2 diabetes mellitus. Circulation 106(6):679–684. https://doi.org/10.1161/01.cir.0000025403.20953.23
Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, Fu H, Xue X, Lu C, Ma J (2018) Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science 359(6380):1151–1156. https://doi.org/10.1126/science.aao5774
Magoc T, Salzberg SL (2011) FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics 27(21):2957–2963. https://doi.org/10.1093/bioinformatics/btr507
Wang Q, Garrity GM, Tiedje JM, Cole JR (2007) Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol 73(16):5261–5267. https://doi.org/10.1128/aem.00062-07
Schloss PD, Westcott SL, Ryabin T, Hall JR, Hartmann M, Hollister EB, Lesniewski RA, Oakley BB, Parks DH, Robinson CJ, Sahl JW, Stres B, Thallinger GG, Van Horn DJ, Weber CF (2009) Introducing mothur: open-Source, platform-independent, community-supported software for describing and comparing microbial communities. Appl Environ Microbiol 75(23):7537–7541. https://doi.org/10.1128/aem.01541-09
Zubiría MG, Gambaro SE, Rey MA, Carasi P, Serradell MDLÁ, Giovambattista A (2017) Deleterious metabolic effects of high fructose intake: the preventive effect of Lactobacillus kefiri administration. Nutrients 9(5):470. https://doi.org/10.3390/nu9050470
Liu ZG, Qiao QL, Sun YL, Chen YW, Ren B, Liu XB (2017) Sesamol ameliorates diet-induced obesity in C57BL/6J mice and suppresses adipogenesis in 3T3-L1 cells via regulating mitochondria-lipid metabolism. Mol Nutr Food Res. https://doi.org/10.1002/mnfr.201600717
Lee E, Jung SR, Lee SY, Lee NK, Paik HD, Lim SI (2018) Lactobacillus plantarum strain Ln4 attenuates diet-induced obesity, insulin resistance, and changes in hepatic mrna levels associated with glucose and lipid metabolism. Nutrients 10(5):643. https://doi.org/10.3390/nu10050643
Pothuraju R, Sharma RK, Kumar KP, Chagalamarri J, Jangra S, Bhakri G, De S (2016) Anti-obesity effect of milk fermented by Lactobacillus plantarum NCDC 625 alone and in combination with herbs on high fat diet fed C57BL/6J mice. Benef Microbes 7(3):1. https://doi.org/10.3920/BM2015.0083
Li C, Ding Q, Nie SP, Zhang YS, Xiong T, Xie MY (2014) Carrot juice fermented with Lactobacillus plantarum NCU116 ameliorates type 2 diabetes in rats. J Agric Food Chem 62(49):11884. https://doi.org/10.1021/jf503681r
Pan WW, Myers MG (2018) Leptin and the maintenance of elevated body weight. Nat Rev Neurosci 19(2):95–105. https://doi.org/10.1038/nrn.2017.168
Friedman JM, Halaas JL (1998) Leptin and the regulation of body weight in mammals. Nature 395(6704):763–770. https://doi.org/10.1038/27376
Grunfeld C, Zhao C, Fuller J, Pollock A, Moser A, Friedman J, Feingold KR (1996) Endotoxin and cytokines induce expression of leptin, the ob gene product, in hamsters—a role for leptin in the anorexia of infection. J Clin Investig 97(9):2152–2157. https://doi.org/10.1172/jci118653
Liu Y, Palanivel R, Rai E, Park M, Gabor TV, Scheid MP, Xu AM, Sweeney G (2015) Adiponectin stimulates autophagy and reduces oxidative stress to enhance insulin sensitivity during high-fat diet feeding in mice. Diabetes 64(1):36–48. https://doi.org/10.2337/db14-0267
Hosogai N, Fukuhara A, Oshima K, Miyata Y, Tanaka S, Segawa K, Furukawa S, Tochino Y, Komuro R, Matsuda M, Shimomura I (2007) Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Diabetes 56(4):901–911. https://doi.org/10.2337/db06-0911
Cranford TL, Enos RT, Velazquez KT, McClellan JL, Davis JM, Singh UP, Nagarkatti M, Nagarkatti PS, Robinson CM, Murphy EA (2016) Role of MCP-1 on inflammatory processes and metabolic dysfunction following high-fat feedings in the FVB/N strain. Int J Obes 40(5):844–851. https://doi.org/10.1038/ijo.2015.244
Torres S, Fabersani E, Marquez A, Gauffin-Cano P (2018) Adipose tissue inflammation and metabolic syndrome. The proactive role of probiotics. Eur J Nutr. https://doi.org/10.1007/s00394-018-1790-2
Zhu J, Tang HY, Zhang ZH, Zhang Y, Qiu CF, Zhang L, Huang PE, Li F (2017) Kaempferol slows intervertebral disc degeneration by modifying LPS-induced osteogenesis/adipogenesis imbalance and inflammation response in BMSCs. Int Immunopharmacol 43:236–242. https://doi.org/10.1016/j.intimp.2016.12.020
Cani PD, Delzenne NM (2011) The gut microbiome as therapeutic target. Pharmacol Ther 130(2):202–212. https://doi.org/10.1016/j.pharmthera.2011.01.012
Moya-Pérez A, Neef A, Sanz Y (2015) Bifidobacterium pseudocatenulatum CECT 7765 reduces obesity-associated inflammation by restoring the lymphocyte-macrophage balance and gut microbiota structure in high-fat diet-fed mice. PLoS One. https://doi.org/10.1371/journal.pone.0126976
Li KK, Tian PJ, Wang SD, Lei P, Qu L, Huang JP, Shan YJ, Li BL (2017) Targeting gut microbiota: Lactobacillus alleviated type 2 diabetes via inhibiting LPS secretion and activating GPR43 pathway. J Funct Foods 38:561–570. https://doi.org/10.1016/j.jff.2017.09.049
Singh DP, Khare P, Bijalwan V, Baboota RK, Singh J, Kondepudi KK, Chopra K, Bishnoi M (2017) Coadministration of isomalto-oligosaccharides augments metabolic health benefits of cinnamaldehyde in high fat diet fed mice. BioFactors 43(6):821–835. https://doi.org/10.1002/biof.1381
Kang C, Wang B, Kaliannan K, Wang XL, Lang HD, Hui SC, Huang L, Zhang Y, Zhou M, Chen MT, Mi MT (2017) Gut microbiota mediates the protective effects of dietary capsaicin against chronic low-grade inflammation and associated obesity induced by high-fat diet. mBio 8(3):14. https://doi.org/10.1128/mBio.00470-17
Moreno-Navarrete JM, Ortega F, Serino M, Luche E, Waget A, Pardo G, Salvador J, Ricart W, Fruhbeck G, Burcelin R, Fernandez-Real JM (2012) Circulating lipopolysaccharide-binding protein (LBP) as a marker of obesity-related insulin resistance. Int J Obes 36(11):1442–1449. https://doi.org/10.1038/ijo.2011.256
Hersoug LG, Moller P, Loft S (2016) Gut microbiota-derived lipopolysaccharide uptake and trafficking to adipose tissue: implications for inflammation and obesity. Obes Rev 17(4):297–312. https://doi.org/10.1111/obr.12370
Bomhof MR, Saha DC, Reid DT, Paul HA, Reimer RA (2014) Combined effects of oligofructose and Bifidobacterium animalis on gut microbiota and glycemia in obese rats. Obesity 22(3):763–771. https://doi.org/10.1002/oby.20632
Thiennimitr P, Yasom S, Tunapong W, Chunchai T, Wanchai K, Pongchaidecha A, Lungkaphin A, Sirilun S, Chaiyasut C, Chattipakorn N (2018) Lactobacillus paracasei HII01, xylooligosaccharides and synbiotics reduced gut disturbance in obese rats. Nutrition 54:40–47. https://doi.org/10.1016/j.nut.2018.03.005
Linden DR (2014) hydrogen sulfide signaling in the gastrointestinal tract. Antioxid Redox Signal 20(5):818–830. https://doi.org/10.1089/ars.2013.5312
Floch MH (2010) The effect of probiotics on host metabolism the microbiota and fermentation. J Clin Gastroenterol 44:S19–S21. https://doi.org/10.1097/MCG.0b013e3181dd4fb7
Chen YT, Lin YC, Lin JS, Yang NS, Chen MJ (2018) Sugary kefir strain Lactobacillus mali APS1 ameliorated hepatic steatosis by regulation of SIRT-1/Nrf-2 and gut microbiota in rats. Mol Nutr Food Res. https://doi.org/10.1002/mnfr.201700903
Liang Y, Lin C, Zhang Y, Deng Y, Liu C, Yang Q (2018) Probiotic mixture of Lactobacillus and Bifidobacterium alleviates systemic adiposity and inflammation in non-alcoholic fatty liver disease rats through Gpr109a and the commensal metabolite butyrate. Inflammopharmacology 26(4):1051–1055
Acknowledgements
This work was financially supported by Special Fund for Agro-scientific Research in the Public Interest [Grant No. 201503135].
Author information
Authors and Affiliations
Contributions
TW and XL designed the study and wrote the manuscript; HY and YL performed the experiments; XL and XW analyzed the data; YS and YY interpreted the results of experiments; BL and YZ prepared figures. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflicts of interest.
Ethical standards
All animal experiments were carried out in accordance with the Guide for the Care and Use of Laboratory Animals: Eighth Edition, ISBN-10: 0-309-15396-4, and experimental procedures were approved by the Animal Ethics Committee of Xi’an Jiaotong University.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, T., Yan, H., Lu, Y. et al. Anti-obesity effect of Lactobacillus rhamnosus LS-8 and Lactobacillus crustorum MN047 on high-fat and high-fructose diet mice base on inflammatory response alleviation and gut microbiota regulation. Eur J Nutr 59, 2709–2728 (2020). https://doi.org/10.1007/s00394-019-02117-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-02117-y