Abstract
Purpose
Minerals and vitamins are essential for optimal growth and development, particularly during the first years of life. Therefore, regularly evaluating their intake makes sense. For this purpose, we report the data from the Nutri-Bébé 2013 survey in comparison with the European Food Safety Authority Adequate Intake (AI), or Average Requirement, (AR) according to age.
Methods
This observational, nationally representative, cross-sectional survey was conducted in 1035 non-breastfed French children aged 0.5–35 months. Dietary intake was recorded using a food diary on three non-consecutive days, framed by two face-to-face interviews.
Results
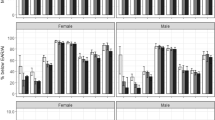
The intake of zinc, magnesium and water-soluble vitamins most of the time met the recommendations. From the first weeks of life, sodium intake exceeded the AI, with a maximum median intake of 1137 mg/day after the age of 30 months. However, it has decreased since 2005. Calcium median intake often exceeded the AI or AR, reaching a maximum of 780 mg/day between 18 and 23 months. Median vitamin A intake always exceeded the AI or AR but exceeded the recommended upper limit in only a few cases. After 2 years, median iron intake was clearly below the AR, i.e. lower than 6.0 mg/day. Dietary vitamin D intake was below the AI, thereby justifying adequate supplementation. Vitamin E intake was below the AI in 50–75% of toddlers.
Conclusion
This survey highlights excessive sodium intake as well as a shortfall of iron, vitamin D, and vitamin E intakes. The potential consequences of these discrepancies with respect to health outcomes remain to be assessed.




Similar content being viewed by others
Abbreviations
- AI:
-
Adequate Intake
- ANSES:
-
Agence Nationale de Sécurité Sanitaire de l’Alimentation, de l’Environnement et du Travail (French Agency for Food, Environmental and Occupational Health and Safety)
- AR:
-
Average requirement
- Ca:
-
Calcium
- CAPI:
-
Computer-assisted personal interviews
- CIQUAL:
-
Centre d’Informations sur la Qualité des Aliments (Information Center on Food Quality)
- CREDOC:
-
Centre de Recherche pour l’Étude et l’Observation des Conditions de Vie (Research Centre for the Study and Observation of Living Conditions)
- d:
-
Day
- DI:
-
Daily dietary Intake
- DRVs:
-
Dietary reference values
- EFSA:
-
European Food Safety Authority
- FOF:
-
Follow-on-formula
- FSB:
-
Foods intended specifically for babies
- GUM:
-
Growing-up-milk
- IF:
-
Infant Formula
- IFN:
-
Institut Français de Nutrition (French Institute of Nutrition)
- INCA:
-
(Enquête) Individuelle et Nationale sur les Consommations Alimentaires (Individual and National Food Consumption Survey)
- NE:
-
Niacin equivalent
- INSEE:
-
Institut National de la Statistique et des Études Economiques (National Institute of Statistics and Economic Studies)
- IOM:
-
Institute of Medicine
- mo:
-
Months
- NS:
-
No significant difference
- PRI:
-
Population reference intake
- RE:
-
Retinol equivalent
- SD:
-
Standard deviation
- SFAE:
-
Secteur Français des Aliments de l’Enfance (French Organisation for Children’s Foods)
- UL:
-
Upper limit
- WHO:
-
World Health Organization
- YCF:
-
Young child formula
References
Field CJ (2009) Early risk determinants and later health outcomes: implications for research prioritization and the food supply. Am J Clin Nutr 89:1533S–1539S. https://doi.org/10.3945/ajcn.2009.27113H
Simeoni U, Bocquet A, Briend A, Chouraqui JP, Darmaun D, Dupont C, Feillet F, Frelut ML, Girardet JP, Goulet O, Hankard R, Rieu D, Rozé JC, Turck D, Vidailhet M, Comité de nutrition de la Société française de pédiatrie, (2016) Early origins of adult disease. Arch Pediatr 23:443–446. https://doi.org/10.1016/j.arcped.2016.01.009
Bailey RL, West KP Jr, Black RE (2015) The epidemiology of global micronutrient deficiencies. Ann Nutr Metab 66(Suppl 2):22–33. https://doi.org/10.1159/000371618
WHO guideline (2016) Use of multiple micronutrient powders for point-of-use fortification of foods consumed by infants and young children aged 6–23 months and children aged 2–12 years. World Health Organization, Geneva. Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/nutrition/publications/micronutrients/guidelines/mmpowders-infant6to23mons-children2to12yrs/en/. Accessed 17 Oct 2018
Boggio V, Lestradet H, Astier-Dumas M, Machinot S, Suquet M, Klepping J (1984) Characteristics of the dietary intake of French children from 3 to 24 months of age. Arch Pediatr 41:499–505
Boggio V, Fantino M (1991) Recent trends in nutritional intake in French infants: comparison of 2 national surveys conducted in 1981 and 1989. In: Journées parisiennes de pédiatrie. Médecine Sciences Flammarion, Paris, pp 275–282
Boggio V, Grossiord A, Guyon S, Fuchs F, Fantino M (1999) Food consumption of infants and young children in France in 1997. Arch Pediatr 6:740–747
Fantino M, Gourmet E (2008) Energy consumption and nutritional intake in non breast-fed children under 36 months old. Arch Pediatr 15:34–49. https://doi.org/10.1016/j.arcped.2008.03.002
Chouraqui JP, Tavoularis G, Emery Y, Francou A, Hébel P, Bocquet M, Hankard R, Turck D (2018) The French national survey on food consumption of children under 3 years of age—Nutri-Bébé 2013: design, methodology, population sampling and feeding practices. Public Health Nutr 21:502–514. https://doi.org/10.1017/S1368980017002518(Epub 2017 Nov 2)
Chouraqui JP, Tavoularis G, Simeoni U, Ferry C, Turck D (2019) Food, water, energy, and macronutrient intake of non-breastfed infants and young children (0–3 years). Eur J Nutr. https://doi.org/10.1007/s00394-018-1883-y(Epub ahead of print)
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2013) Scientific opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA J 11(10):3408. https://doi.org/10.2903/j.efsa.2013.3408. www.efsa.europa.eu/efsajournal. Accessed 10 Aug 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2015) Scientific opinion on dietary reference values for calcium. EFSA J 13(5):4101–4748. https://doi.org/10.2903/j.efsa.2015.4101. www.efsa.europa.eu/efsajournal. Accessed 20 Nov 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2015) Scientific opinion on dietary reference values for phosphorus. EFSA J 13(7):4185. https://doi.org/10.2903/j.efsa.2015.4185. www.efsa.europa.eu/efsajournal. Accessed 20 Nov 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2015) Scientific opinion on dietary reference values for magnesium. EFSA J 13(7):4186. https://doi.org/10.2903/j.efsa.2015.4186. www.efsa.europa.eu/efsajournal. Accessed 22 Nov 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2015) Scientific opinion on dietary reference values for iron. EFSA J 13(10):4254–4369. https://doi.org/10.2903/j.efsa.2015.4254. www.efsa.europa.eu/efsajournal. Accessed 22 Nov 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2014) Scientific opinion on dietary reference values for zinc. EFSA J 12(10):3844–3920. https://doi.org/10.2903/j.efsa.2014.3844. www.efsa.europa.eu/efsajournal. Accessed 22 Nov 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2015) Scientific opinion on dietary reference values for vitamin A. EFSA J 13(3):4028–4112. https://doi.org/10.2903/j.efsa.2015.4028. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2016) Scientific opinion on dietary reference values for vitamin D. EFSA J NNNN. https://doi.org/10.2903/j.efsa.2016.NNN. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2016) Scientific opinion on dietary reference values for thiamin. EFSA J 14(12):4653. https://doi.org/10.2903/j.efsa.2016. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2014) Scientific opinion on dietary reference values for niacin. EFSA J 12(7): 3759. https://doi.org/10.2903/j.efsa.2014.3759. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2016) Scientific opinion on dietary reference values for vitamin B6. EFSA J 14(6): 4485. https://doi.org/10.2903/j.efsa.2016.4485. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2014) Scientific opinion on dietary reference values for folate. EFSA J 12(11): 3893. https://doi.org/10.2903/j.efsa.2014.3893. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies) (2015) Scientific opinion on dietary reference values for cobalamin (vitamin B12). EFSA J 13(7):4150. https://doi.org/10.2903/j.efsa.2015.4150. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
European Food Safety Authority (2009) General principles for the collection of national food consumption data in the view of a pan-European dietary survey. EFSA J 7(12): 1435. http://www.efsa.europa.eu. Accessed 17 Oct 2012
Centre d’Information sur la Qualité des Aliments (2012) Table CIQUAL http://www.afssa.fr/TableCIQUAL/. But replaced by a new one in 2016: https://pro.anses.fr/tableciqual/. Accessed 8 March 2013
EFSA NDA Panel (EFSA Panel on Panel on Dietetic Products Nutrition and Allergies) (2014) scientific opinion on dietary reference values for iodine. EFSA J 12(5):3660. https://doi.org/10.2903/j.efsa.2014.3660. www.efsa.europa.eu/efsajournal. Accessed 13 Feb 2015
Mihatsch WA, Braegger C, Bronsky J, Campoy C, Domellöf M, Fewtrell M, Mis NF, Hojsak I, Hulst J, Indrio F, Lapillonne A, Mlgaard C, Embleton N, van Goudoever J, ESPGHAN Committee on Nutrition, (2016) Prevention of vitamin K deficiency bleeding in newborn infants: a position paper by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 63:123–129. https://doi.org/10.1097/MPG.0000000000001232
EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA) (2010) Scientific opinion on principles for deriving and applying dietary reference values. EFSA J 8(3):1458. https://doi.org/10.2903/j.efsa.2010.1458. www.efsa.europa.eu. Accessed 10 Aug 2017
Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes; Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes (2000) Dietary reference intakes: applications in dietary assessment. National Academies Press, Washington (DC). https://doi.org/10.17226/9956
EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA) (2006) Scientific committee on food. Tolerable upper intake levels for vitamins and minerals. http://www.efsa.europa.eu/sites/default/files/efsa_rep/blobserver_assets/ndatolerableuil.pdf. Accessed 6 Dec 2018
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2012) Scientific opinion on the tolerable upper intake level of vitamin D. EFSA J 10(7):2813. https://doi.org/10.2903/j.efsa.2012.2813. www.efsa.europa.eu/efsajournal. Accessed 6 Dec 2018
Agence Nationale de Sécurité Sanitaire de l’Alimentation, de l’Environnement et du Travail (ANSES) (2017) Étude individuelle nationale des consommations alimentaires 3 (INCA 3). https://www.anses.fr/fr/system/files/NUT2014SA0234Ra.pdf. Accessed 6 Dec 2017
Butte NF, Fox MK, Briefel RR, Siega-Riz AM, Dwyer JT, Deming DM, Reidy KC (2010) Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed dietary reference intakes. J Am Diet Assoc 110:S27–S37. https://doi.org/10.1016/j.jada.2010.09.004
Tian N, Zhang Z, Loustalot F, Yang Q, Cogswell ME (2013) Sodium and potassium intakes among US infants and preschool children, 2003–2010. Am J Clin Nutr 98:1113–1122. https://doi.org/10.3945/ajcn.113.060012
Gibson S, Sidnell A (2014) Nutrient adequacy and imbalance among young children aged 1–3 years in the UK. Nutr Bull 39:172–180. https://doi.org/10.1111/nbu.12087
Cribb VL, Warren JM, Emmett PM (2012) Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr 66:104–110. https://doi.org/10.1038/ejcn.2011.137
Maalouf J, Cogswell ME, Yuan K, Martin C, Gunn JP, Pehrsson P, Merritt R, Bowman B (2015) Top sources of dietary sodium from birth to age 24 mo, United States, 2003–2010. Am J Clin Nutr 101:1021–1028. https://doi.org/10.3945/ajcn.114.099770
Girardet JP, Rieu D, Bocquet A, Bresson JL, Briend A, Chouraqui JP, Darmaun D, Dupont C, Frelut ML, Hankard R, Goulet O, Simeoni U, Turck D, Vidailhet M, Comité de nutrition de la Société française de pédiatrie (2014) Salt intake in children. Arch Pediatr 21:521–528. https://doi.org/10.1016/j.arcped.2014.02.007
Newberry SJ, Chung M, Anderson CAM, Chen C, Fu Z, Tang A, Zhao N, Booth M, Marks J, Hollands S, Motala A, Larkin JK, Shanman R, Hempel S (2018) Sodium and potassium intake: effects on chronic disease outcomes and risks. Comparative effectiveness review no. 206. Agency for Healthcare Research and Quality No. 18-EHC009-EF. https://www.ncbi.nlm.nih.gov/books/NBK519328/. Accessed 6 Dec 2018
Messerli FH, Hofstetter L, Bangalore S (2018) Salt and heart disease: a second round of “bad science”? Lancet 392(10146):456–458. https://doi.org/10.1016/S0140-6736(18)31724-0
Fomon SJ, Ziegler EE (1999) Renal solute load and potential renal solute load in infancy. J Pediatr 134:11–14
Nomura K, Asayama K, Jacobs L, Thijs L, Staessen JA (2017) Renal function in relation to sodium intake: a quantitative review of the literature. Kidney Int 92:67–78. https://doi.org/10.1016/j.kint.2016.11.032
Iwahori T, Miura K, Ueshima H (2017) Time to consider use of the sodium-to-potassium ratio for practical sodium reduction and potassium increase. Nutrients. https://doi.org/10.3390/nu9070700
Birch LL, Doub AE (2014) Learning to eat: birth to age 2 years. Am J Clin Nutr 99:723S–728S. https://doi.org/10.3945/ajcn.113.069047
Haut conseil de la santé publique (2017) Pour une politique nationale nutrition santé en France PNNS 2017–2021. https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=632. Accessed 6 May 2018
Atkins LA, McNaughton SA, Campbell KJ, Szymlek-Gay EA (2016) Iron intakes of Australian infants and toddlers: findings from the Melbourne Infant Feeding, Activity and Nutrition Trial (InFANT) Program. Br J Nutr 115:285–293. https://doi.org/10.1017/S0007114515004286
Cusick SE, Georgieff MK, Rao R (2018) Approaches for reducing the risk of early-life irondeficiency-induced brain dysfunction in children. Nutrients 10(2):1. https://doi.org/10.3390/nu10020227
McClung JP (2018) Iron, zinc, and physical performance. Biol Trace Elem Res 188:135–139. https://doi.org/10.1007/s12011-018-1479-7.30112658
Haskell MJ (2012) The challenge to reach nutritional adequacy for vitamin A: β-carotene bioavailability and conversion-evidence in humans. Am J Clin Nutr 96:1193S–1203S. https://doi.org/10.3945/ajcn.112.034850
Novotny JA, Harrison DJ, Pawlosky R, Flanagan VP, Harrison EH, Kurilich AC (2010) Beta-carotene conversion to vitamin A decreases as the dietary dose increases in humans. J Nutr 140:915–918. https://doi.org/10.3945/jn.109.116947
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA) (2014) Scientific opinion on the essential composition of infant and follow-on formulas. EFSA J 12(7):3760. https://doi.org/10.2903/j.efsa.2014.3760. https://www.efsa.europa.eu/fr/efsajournal/pub/3760. Accessed 18 Sept 2017
Commission delegated regulation (EU) 2016/127 of 25 September 2015 supplementing Regulation (EU) No 609/2013 of the European Parliament and of the Council as regards the specific compositional and information requirements for infant formula and follow-on formula and as regards requirements on information relating to infant and young child feeding. Official Journal of the European Union, L 25. http://data.europa.eu/eli/reg_del/2016/127/oj. Accessed 2 Feb 2016
Vidailhet M, Rieu D, Feillet F, Bocquet A, Chouraqui JP, Darmaun D, Dupont C, Frelut ML, Girardet JP, Hankard R, Rozé JC, Siméoni U, Turck D, Briend A (2017) Vitamin A in pediatrics: an update from the Nutrition Committee of the French Society of Pediatrics. Arch Pediatr 24:288–297. https://doi.org/10.1016/j.arcped.2016.11.021
Mason J, Greiner T, Shrimpton R, Sanders D, Yukich J (2015) Vitamin A policies need rethinking. Int J Epidemiol 44:283–292. https://doi.org/10.1093/ije/dyu194
Vidailhet M, Mallet E, Bocquet A, Bresson JL, Briend A, Chouraqui JP, Darmaun D, Dupont C, Frelut ML, Ghisolfi J, Girardet JP, Goulet O, Hankard R, Rieu D, Simeoni U, Turck D, Comité de nutrition de la Société française de pédiatrie, (2012) Vitamin D: still a topical matter in children and adolescents. A position paper by the Committee on Nutrition of the French Society of Paediatrics. Arch Pediatr 19:316–328. https://doi.org/10.1016/j.arcped.2011.12.015
Traber MG (2014) Vitamin E inadequacy in humans: causes and consequences. Adv Nutr 5:503–514. https://doi.org/10.3945/an.114.006254
Acknowledgements
The authors thank all the families having participated in the survey, and all the SOFRES and CREDOC team members who contributed in collecting and analysing the data. The Nutri-Bébé survey has been funded by the “Secteur Français des Aliments de l’Enfance” (SFAE), 9 boulevard Malesherbes, Paris-75008 France.
Author information
Authors and Affiliations
Contributions
JPC was involved in the study design, data collection, analysis, and interpretation of data, wrote the manuscript, and had responsibility for the final content of the manuscript. GT conceived the study, participated in its design and coordination, collected the data, performed the statistical analysis, and revised the manuscript. CF contributed in writing the manuscript. MB designed, coordinated and supervised the survey. DT and FF reviewed, and provided comments on drafts of the manuscript. All authors read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
JPC received an honorarium as scientific consultant from the CREDOC. GT is employed by the CREDOC that received funding from the SFAE to carry out the present study. CF is employed by the SFAE. DT and FF declare that they have no competing interest.
Ethical approval
Ethical approval was not required according to French law, since the current research was conducted by an official polling institute, TNS Sofres, in full agreement with the guidelines laid down in the Declaration of Helsinki and the French data protection act and did not involve invasive procedures or therapeutic intervention other than usual vitamin supplementation. The study was registered on ClinicalTrials.gov (NCT03327415).
Rights and permissions
About this article
Cite this article
Chouraqui, JP., Tavoularis, G., Turck, D. et al. Mineral and vitamin intake of infants and young children: the Nutri-Bébé 2013 survey. Eur J Nutr 59, 2463–2480 (2020). https://doi.org/10.1007/s00394-019-02093-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-02093-3