Abstract
Purpose
Liquids have higher ingestion and gastric-emptying rates, resulting in rapid glycemic response. They are also less satiating than solid foods. This study examined if the addition of plant proteins alter postprandial glucose, insulin, triglycerides, glucose-dependent insulinotropic peptide (GIP), glycogen-like peptide-1 (GLP-1) and appetitive responses to a sugar-sweetened beverage.
Methods
This was a randomized, crossover acute feeding study consisting of four treatments: chocolate beverage alone (50 g carbohydrate), or added with 24 g oat, pea or rice proteins. Twenty Chinese males (mean ± SD age 26 ± 5 years; body mass index 21.5 ± 1.7 kg/m2) ingested the test drink after an overnight fast. Venous blood samples and subjective appetite ratings were collected before test beverage and at fixed intervals for 180 min. Blood biochemical data and appetite ratings were compared using repeated-measures ANOVA.
Results
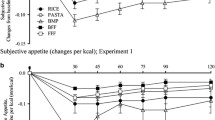
Significant interaction effects were found in postprandial glucose excursions (time × protein effects, p = 0.003). Glucose iAUC was lower in pea and rice proteins, although not significantly (p > 0.385). Insulin iAUC was significantly higher in the oat (p = 0.035) and pea (p = 0.036) protein beverages. GIP and GLP-1 release in a sub-sample (n = 10) followed a comparable order as insulin release (p = 0.397 and 0.454, respectively). Significant interaction effects were found in fullness ratings (p = 0.024), and a trend of greater suppression of hunger and desire-to-eat was also documented (p = 0.088 and 0.080, respectively).
Conclusions
Plant proteins altered the glycemic and appetitive responses of Asian males to a sugar-sweetened beverage. Food-based interventions are useful in promoting glycemic control. This trial was registered with ClinicalTrials.gov as NCT02933424.


Similar content being viewed by others
References
American Diabetes Association (2017) 2. Classification and diagnosis of diabetes. Diabetes Care 40(Supplement 1):S11–S24
Temelkova-Kurktschiev TS, Koehler C, Henkel E, Leonhardt W, Fuecker K, Hanefeld M (2000) Postchallenge plasma glucose and glycemic spikes are more strongly associated with atherosclerosis than fasting glucose or HbA1c level. Diabetes Care 23(12):1830–1834
Cavalot F, Petrelli A, Traversa M, Bonomo K, Fiora E, Conti M, Anfossi G, Costa G, Trovati M (2006) Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga Diabetes Study. J Clin Endocrinol Metab 91(3):813–819
Dickinson S, Colagiuri S, Faramus E, Petocz P, Brand-Miller J (2002) Postprandial hyperglycemia and insulin sensitivity differ among lean young adults of different ethnicities. J Nutr 132(9):2574–2579
Ma RC, Chan JC (2013) Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann NY Acad Sci 1281(1):64–91
Behall KM, Scholfield DJ, Canary J (1988) Effect of starch structure on glucose and insulin responses in adults. Am J Clin Nutr 47(3):428–432
Brennan CS (2005) Dietary fibre, glycaemic response, and diabetes. Mol Nutr Food Res 49(6):560–570
Tan S-Y, Peh EW-Y, Marangoni AG, Henry CJ (2017) Effects of liquid oil vs. oleogel co-ingested with a carbohydrate-rich meal on human blood triglycerides, glucose, insulin and appetite. Food Funct 8:241–249
American Diabetes Association (2017) 4. Lifestyle management. Diabetes Care 40(Supplement 1):S33–S43
Karhunen L, Juvonen K, Huotari A, Purhonen A, Herzig K (2008) Effect of protein, fat, carbohydrate and fibre on gastrointestinal peptide release in humans. Regul Pept 149(1):70–78
Sun L, Wei Jie Tan K, Jeyakumar Henry C (2015) Co-ingestion of essence of chicken to moderate glycaemic response of bread. Int J Food Sci Nutr 66(8):931–935
van Loon LJ, Saris WH, Verhagen H, Wagenmakers AJ (2000) Plasma insulin responses after ingestion of different amino acid or protein mixtures with carbohydrate. Am J Clin Nutr 72(1):96–105
Hu FB, Malik VS (2010) Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav 100(1):47–54
Camilleri M, Malagelada JR, Brown ML, Becker G, Zinsmeister AR (1985) Relation between antral motility and gastric emptying of solids and liquids in humans. Am J Physiol 249(5):G580–G585
Cassady BA, Considine RV, Mattes RD (2012) Beverage consumption, appetite, and energy intake: what did you expect? Am J Clin Nutr 95(3):587–593
Dhillon J, Running CA, Tucker RM, Mattes RD (2016) Effects of food form on appetite and energy balance. Food Qual Prefer 48:368–375
Duffey KJ, Popkin BM (2007) Shifts in patterns and consumption of beverages between 1965 and 2002. Obesity 15(11):2739–2747
Barquera S, Hernandez-Barrera L, Tolentino ML, Espinosa J, Ng SW, Rivera JA, Popkin BM (2008) Energy intake from beverages is increasing among Mexican adolescents and adults. J Nutr 138(12):2454–2461
Bell A, Kremer P, Magarey AM, Swinburn B (2005) Contribution of ‘noncore’foods and beverages to the energy intake and weight status of Australian children. Eur J Clin Nutr 59(5):639–645
Ma J, Stevens JE, Cukier K, Maddox AF, Wishart JM, Jones KL, Clifton PM, Horowitz M, Rayner CK (2009) Effects of a protein preload on gastric emptying, glycemia, and gut hormones after a carbohydrate meal in diet-controlled type 2 diabetes. Diabetes Care 32(9):1600–1602
Nuttall FQ, Mooradian AD, Gannon MC, Billington C, Krezowski P (1984) Effect of protein ingestion on the glucose and insulin response to a standardized oral glucose load. Diabetes Care 7(5):465–470
Calbet JA, Holst JJ (2004) Gastric emptying, gastric secretion and enterogastrone response after administration of milk proteins or their peptide hydrolysates in humans. Eur J Nutr 43(3):127–139
Dhillon J, Craig BA, Leidy HJ, Amankwaah AF, Anguah KO-B, Jacobs A, Jones BL, Jones JB, Keeler CL, Keller CE (2016) The effects of increased protein intake on fullness: a meta-analysis and its limitations. J Acad Nutr Diet 116(6):968–983
Veldhorst MA, Nieuwenhuizen AG, Hochstenbach-Waelen A, van Vught AJ, Westerterp KR, Engelen MP, Brummer RJ, Deutz NE, Westerterp-Plantenga MS (2009) Dose-dependent satiating effect of whey relative to casein or soy. Physiol Behav 96(4–5):675–682
Nilsson M, Stenberg M, Frid AH, Holst JJ, Björck IM (2004) Glycemia and insulinemia in healthy subjects after lactose-equivalent meals of milk and other food proteins: the role of plasma amino acids and incretins. Am J Clin Nutr 80(5):1246–1253
Gilbert JA, Bendsen NT, Tremblay A, Astrup A (2011) Effect of protein from different sources on body composition. Nutr Metab Cardiovasc Dis 21:B16–B31
Newgard CB, An J, Bain JR, Muehlbauer MJ, Stevens RD, Lien LF, Haqq AM, Shah SH, Arlotto M, Slentz CA (2009) A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab 9(4):311–326
Hall W, Millward D, Long S, Morgan L (2003) Casein and whey exert different effects on plasma amino acid profiles, gastrointestinal hormone secretion and appetite. Br J Nutr 89(02):239–248
Floyd JC Jr, Fajans SS, Conn JW, Knopf RF, Rull J (1966) Stimulation of insulin secretion by amino acids. J Clin Invest 45(9):1487–1502
Nestle M (1999) Animal v. plant foods in human diets and health: is the historical record unequivocal? Proc Nutr Soc 58(02):211–218
World Health Organization (2003) Diet, nutrition and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. WHO Tech Rep Series, Geneva
Quek R, Bi X, Henry CJ (2016) Impact of protein-rich meals on glycaemic response of rice. Br J Nutr 115(07):1194–1201
Shewry PR, Halford NG (2002) Cereal seed storage proteins: structures, properties and role in grain utilization. J Exp Bot 53(370):947–958
Spiller GA, Jensen CD, Pattison T, Chuck CS, Whittam JH, Scala J (1987) Effect of protein dose on serum glucose and insulin response to sugars. Am J Clin Nutr 46(3):474–480
Flint A, Raben A, Blundell JE, Astrup A (2000) Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes 24(1):38–48
Wolever TM (2006) Determining the GI of foods—methodological considerations. In: Wolever TM (ed) The glycaemic index: a physiological classification of dietary carbohydrate. CABI, Wallingford, pp 12–42
Veldhorst MA, Nieuwenhuizen AG, Hochstenbach-Waelen A, Westerterp KR, Engelen MP, Brummer R-JM, Deutz NE, Westerterp-Plantenga MS (2009) Effects of high and normal soyprotein breakfasts on satiety and subsequent energy intake, including amino acid and ‘satiety’hormone responses. Eur J Nutr 48(2):92–100
Calbet JA, MacLean DA (2002) Plasma glucagon and insulin responses depend on the rate of appearance of amino acids after ingestion of different protein solutions in humans. J Nutr 132(8):2174–2182
Claessens M, Calame W, Siemensma AD, Saris WH, van Baak MA (2007) The thermogenic and metabolic effects of protein hydrolysate with or without a carbohydrate load in healthy male subjects. Metabolism 56(8):1051–1059
Ishikawa Y, Hira T, Inoue D, Harada Y, Hashimoto H, Fujii M, Kadowaki M, Hara H (2015) Rice protein hydrolysates stimulate GLP-1 secretion, reduce GLP-1 degradation, and lower the glycemic response in rats. Food Funct 6(8):2525–2534
Fajans S, Floyd Jr J, Knopf R, Conn J (2013) Effect of amino acids and proteins on insulin secretion in man. In: Schering symposium on endocrinology, Berlin, May 26 to 27, 1967: advances in the biosciences, Elsevier, p 231
Gilani GS, Cockell KA, Sepehr E (2005) Effects of antinutritional factors on protein digestibility and amino acid availability in foods. J AOAC Int 88(3):967–987
Holt GM, Owen LJ, Till S, Cheng Y, Grant VA, Harden CJ, Corfe BM (2016) Systematic literature review shows that appetite rating does not predict energy intake. Crit Rev Food Sci Nutr in press. doi:10.1080/10408398.2016.1246414
Borzoei S, Neovius M, Barkeling B, Teixeira-Pinto A, Rössner S (2006) A comparison of effects of fish and beef protein on satiety in normal weight men. Eur J Clin Nutr 60(7):897–902
Pal S, Ellis V (2010) The acute effects of four protein meals on insulin, glucose, appetite and energy intake in lean men. Br J Nutr 104(08):1241–1248
Anderson GH, Tecimer SN, Shah D, Zafar TA (2004) Protein source, quantity, and time of consumption determine the effect of proteins on short-term food intake in young men. J Nutr 134(11):3011–3015
Williamson DA, Geiselman PJ, Lovejoy J, Greenway F, Volaufova J, Martin CK, Arnett C, Ortego L (2006) Effects of consuming mycoprotein, tofu or chicken upon subsequent eating behaviour, hunger and safety. Appetite 46(1):41–48
Bowen J, Noakes M, Clifton PM (2006) Appetite regulatory hormone responses to various dietary proteins differ by body mass index status despite similar reductions in ad libitum energy intake. J Clin Endocrinol Metab 91(8):2913–2919
Tan S-Y, Batterham MJ, Tapsell LC (2010) Energy expenditure does not differ, but protein oxidation rates appear lower in meals containing predominantly meat versus soy sources of protein. Obes Facts 3:101–104
Diepvens K, Häberer D, Westerterp-Plantenga M (2008) Different proteins and biopeptides differently affect satiety and anorexigenic/orexigenic hormones in healthy humans. Int J Obes 32(3):510–518
Chungchunlam SM, Henare SJ, Ganesh S, Moughan PJ (2017) Effects of whey protein and its two major protein components on satiety and food intake in normal-weight women. Physiol Behav 175(1):113–118
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ (2008) Translating the A1C assay into estimated average glucose values. Diabetes Care 31(8):1473–1478
Acknowledgements
We would like to thank our clinical trial nurse, Ms. Susanna Lim, for her phlebotomy assistance in this study. This study was partially funded by Wilmar International Limited. We would like to thank Wilmar for the rice protein, Tate & Lyle for the oat protein, and Roquette Freres for the pea protein concentrate used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tan, SY., Siow, P.C., Peh, E. et al. Influence of rice, pea and oat proteins in attenuating glycemic response of sugar-sweetened beverages. Eur J Nutr 57, 2795–2803 (2018). https://doi.org/10.1007/s00394-017-1547-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1547-3