Abstract
Purpose
To evaluate the role of miR-124a in the regulation of genes involved in insulin exocytosis and its effects on the kinetics of insulin secretion in pancreatic islets from pregnant rats submitted to a low-protein diet.
Methods
Adult control non-pregnant (CNP) and control pregnant (CP) rats were fed a normal protein diet (17%), whereas low-protein non-pregnant (LPNP) and low-protein pregnant (LPP) rats were fed a low-protein diet (6%) from days 1 to 15 of pregnancy. Kinetics of the glucose-induced insulin release and measurement of [Ca2+]i in pancreatic islets were assessed by standard protocols. The miR-124a expression and gene transcriptions from pancreatic islets were determined by real-time polymerase chain reaction.
Results
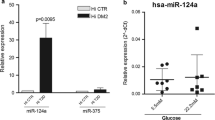
In islets from LPP rats, the first phase of insulin release was abrogated. The AUC [Ca2+]i from the LPP group was lower compared with the other groups. miR-124a expression was reduced by a low-protein diet. SNAP-25 mRNA, protein expression, and Rab3A protein content were lower in the LPP rats than in CP rats. Syntaxin 1A and Kir6.2 mRNA levels were decreased in islets from low-protein rats compared with control rats, whereas their protein content was reduced in islets from pregnant rats.
Conclusions
Loss of biphasic insulin secretion in islets from LPP rats appears to have resulted from reduced [Ca2+]i due, at least in part, to Kir6.2 underexpression and from the changes in exocytotic elements that are influenced either directly or indirectly by miR-124a.








Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- AUC:
-
Area under curve
- cAMP:
-
Adenosine 3′,5′-cyclic monophosphate
- [Ca2+]i :
-
Cytosolic calcium
- CNP:
-
Control non-pregnant
- CP:
-
Control pregnant
- FOXA-2:
-
Forkhead box A2
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GH:
-
Human growth hormone
- GLUT-2:
-
Glucose transporter-2
- KATP :
-
ATP-sensitive K+ channel
- Kir6.2:
-
Inward rectifier potassium channel member 6.2
- K itt :
-
Rate constant for serum glucose disappearance during insulin-tolerance test
- LPNP:
-
Low-protein non-pregnant
- LPP:
-
Low-protein pregnant
- LSD:
-
Least significant difference
- miR:
-
MicroRNA
- PKA:
-
Protein kinase A
- Rab3A:
-
Rabphilin 3A
- Rab27A:
-
Rabphilin 27A
- RNA:
-
Ribonucleic acid
- SDS:
-
Sodium dodecyl sulfate
- SEM:
-
Standard error of the mean
- SNAP-25:
-
Synaptosome-associated protein 25 kDa
- SUR1:
-
Sulfonylurea receptor subunits
- U6 snRNA:
-
Small nuclear ribonucleic acid U6
- VAMP-2:
-
Vesicle-associated membrane protein 2
References
Parsons JA, Brelje TC, Sorenson RL (1992) Adaptation of islets of Langerhans to pregnancy: increased islet cell proliferation and insulin secretion correlates with the onset of placental lactogen secretion. Endocrinology 130:1459–1466
Weinhaus AJ, Stout LE, Sorenson RL (1996) Glucokinase, hexokinase, glucose transporter 2, and glucose metabolism in islets during pregnancy and prolactin-treated islets in vitro: mechanisms for long term up-regulation of islets. Endocrinology 137:1640–1649
Weinhaus AJ, Bhagroo NV, Brelje TC, Sorenson RL (1998) Role of cAMP in upregulation of insulin secretion during the adaptation of islets of Langerhans to pregnancy. Diabetes 47:1426–1435
Cunha DA, Amaral ME, Carvalho CP, Collares-Buzato CB, Carneiro EM, Boschero AC (2006) Increased expression of SNARE proteins and synaptotagmin IV in islets from pregnant rats and in vitro prolactin-treated neonatal islets. Biol Res 39:555–566
Amaral AG, Rafacho A, Machado de Oliveira CA, Batista TM, Ribeiro RA, Latorraca MQ, Bposchero AC, Carneiro EM (2010) Leucine supplementation augments insulin secretion in pancreatic islets of malnourished mice. Pancreas 39:847–855
Souza DF, Ignacio-Souza LM, Reis SR, Reis MA, Stoppiglia LF, Carneiro EM, Boschero AC, Arantes VC, Latorraca MQ (2012) A low-protein diet during pregnancy alters glucose metabolism and insulin secretion. Cell Biochem Funct 30:114–121
Soriano S, Gonzalez A, Marroqui L, Tuduri E, Vieira E, Amaral AG, Batista TM, Rafacho A, Boschero AC, Nadal A, Carneiro EM, Quesada I (2010) Reduced insulin secretion in protein malnourished mice is associated with multiple changes in the beta-cell stimulus-secretion coupling. Endocrinology 151:3543–3554
Batista TM, Ribeiro RA, Silva PM, Camargo RL, Lollo PC, Boschero AC, Carneiro EM (2013) Taurine supplementation improves liver glucose control in normal protein and malnourished mice fed a high-fat diet. Mol Nutr Food Res 57:423–434
Milanski M, Arantes VC, Ferreira F, de Barros Reis MA Carneiro EM, Boschero AC, Collares-Buzato CB, Latorraca MQ (2005) Low-protein diets reduce PKAalpha expression in islets from pregnant rats. J Nutr 135:1873–1878
Sempere LF, Freemantle S, Pitha-Rowe I, Moss E, Dmitrovsky E, Ambros V (2004) Expression profiling of mammalian microRNAs uncovers a subset of brain-expressed microRNAs with possible roles in murine and human neuronal differentiation. Genome Biol 5:R13
Guo H, Ingolia NT, Weissman JS, Bartel DP (2010) Mammalian microRNAs predominantly act to decrease target mRNA levels. Nature 466:835–840
Lovis P, Gattesco S, Regazzi R (2008) Regulation of the expression of components of the exocytotic machinery of insulin-secreting cells by microRNAs. Biol Chem 389:305–312
Baroukh N, Ravier MA, Loder MK, Hill EV, Bounacer A, Scharfmann R, Rutter GA, van Obberghen E (2007) MicroRNA-124a regulates Foxa2 expression and intracellular signaling in pancreatic beta-cell lines. J Biol Chem 282:19575–19588
Scott AM, Atwater I, Rojas E (1981) A method for the simultaneous measurement of insulin release and B cell membrane potential in single mouse islets of Langerhans. Diabetologia 21:470–475
Bordin S, Boschero AC, Carneiro EM, Atwater I (1995) Ionic mechanisms involved in the regulation of insulin secretion by muscarinic agonists. J Membr Biol 148:177–184
Kelley GG, Zawalich KC, Zawalich WS (1995) Synergistic interaction of glucose and neurohumoral agonists to stimulate islet phosphoinositide hydrolysis. Am J Physiol 269:E575–E582
Amaral ME, Ueno M, Carvalheira JB, Carneiro EM Velloso LA, Saad MJ, Boschero AC (2003) Prolactin-signal transduction in neonatal rat pancreatic islets and interaction with the insulin-signaling pathway. Hormon Metab Res 35:282–289
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254
Gutierrez JM, Alvarez J, Díaz F, Fernández S, Menéndez-Patterson A (1991) Influence of nitrogen balance and intestinal glucose absorption on growth of rats recovery from early undernutrition. Nutr Res 11:835–840
Fernández A, Ordás I, Gutiérrez JM, Ganzález C, Fernández S, Patterson AM (1993) The rehabilitation of malnourished rat, at the end of the lactation period, with two different sources of dietary lipids: soybean and olive oils. Nutrition. 12:79–88 (Life Science Advances)
Cerasi E, Luft R (1967) The plasma insulin response to glucose infusion in healthy subjects and in diabetes mellitus. Acta Endocrinol 55:278–304
Henquin JC (2009) Regulation of insulin secretion: a matter of phase control and amplitude modulation. Diabetologia 52:739–751
Rajan AS, Hill RS, Boyd AE 3rd (1989) Effect of rise in cAMP levels on Ca2 + influx through voltage-dependent Ca2+ channels in HIT cells. Second-messenger synarchy in beta-cells. Diabetes 38:874–880
Nadal A, Rovira JM, Laribi O, Leon-Quinto T, Andreu E, Ripoll C, Soria B (1998) Rapid insulinotropic effect of 17beta-estradiol via a plasma membrane receptor. FASEB J 12:1341–1348
Rafacho A, Marroquí L, Taboga SR, Abrantes JL, Silveira LR, Boschero AC, Carneiro EM, Bosqueiro JR, Nadal A, Quesada I (2010) Glucocorticoids in vivo induce both insulin hypersecretion and enhanced glucose sensitivity of stimulus-secretion coupling in isolated rat islets. Endocrinology 151:85–95
Zhang Q, Köhler M, Yang SN, Zhang F, Larsson O, Berggren PO (2004) Growth hormone promotes Ca(2+)-induced Ca2+ release in insulin-secreting cells by ryanodine receptor tyrosine phosphorylation. Mol Endocrinol 18:1658–1669
Straub SG, Sharp GW, Meglasson MD, de Souza CJ (2001) Progesterone inhibits insulin secretion by a membrane delimited, non-genomic action. Biosci Rep 21:653–666
Slingerland AS, Hattersley AT (2005) Mutations in the Kir6.2 subunit of the KATP channel and permanent neonatal diabetes: new insights and new treatment. Ann Med 37:186–195
Izumi T, Gomi H, Kasai K, Mizutani S, Torii S (2003) The roles of Rab27 and its effectors in the regulated secretory pathways. Cell Struct Funct. 28:465–474.
Cheviet S, Coppola T, Haynes LP, Burgoyne RD, Regazzi R (2004) The Rab-binding protein Noc2 is associated with insulin-containing secretory granules and is essential for pancreatic beta-cell exocytosis. Mol Endocrinol 18:117–126
Kasai K, Ohara-Iamizumi M, Takahashi N, Mizutani S, Zhao S, Kikuta T, Kasai H, Nagamatsu S, Gomi H, Izumi T (2005) Rab27A a mediates the tight docking of insulin granules onto the plasma membrane during glucose stimulation. J Clin Investig 115:388–396
Donelan MJ, Morfini G, Julyan R, Sommers S, Hays L, Kajio H, Briaud I, Easom RA, Molkentin JD, Brady ST, Rhodes CJ (2002) Ca2+-dependent dephosphorylation of kinesin heavy chain on beta-granules in pancreatic beta-cells. Implications for regulated beta-granule transport and insulin exocytosis. J Biol Chem 277:24232–24242
Yaekura K, Julyan R, Wicksteed BL, Hays LB, Alarcon C, Sommers S, Poitout V, Baskin DG, Wang Y, Philipson LH, Rhodes CJ (2003) Insulin secretory deficiency and glucose intolerance in Rab3A null mice. J Biol Chem 278:9715–9721
Sudhof TC (1995) The synaptic vesicle cycle: a cascade of protein-protein interactions. Nature 375:645–653
Huang X, Wheeler MB, Kang YH, Sheu L, Lukacs GL, Trimble WS, Gaisano HY (1998) Truncated SNAP-25 (1–197), like botulinum neurotoxin A, can inhibit insulin secretion from HIT-T15 insulinoma cells. Mol Endocrinol 12:1060–1070
Acknowledgements
The authors are grateful to Celso Roberto Afonso for his excellent technical assistance. This work was supported by the Brazilian foundation CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, PROCAD, Grant No. 23038.023925/2008-62) and PRONEX/FAPEMAT (Programa de Apoio a Núcloes de Excelência/ Fundação de Amparo à Pesquisa do Estado de Mato Grosso, Grant No. 825637/2009). This work is part of a dissertation presented by Kariny Cassia de Siqueira as a partial requirement for a Master’s degree in Biosciences at the College of Nutrition, UFMT.
Author contributions
KCS, FML, FSL, MST, CFC, and SRLR carried out the islets isolation and performed real-time PCR and western blotting. RLC, TMB, and EMC help measuring [Ca2+]i. ECV and TRN assisted in cell culture and transfection. KCS, LMIS, and MQL contributed equally to this paper in various aspects of this study. KCS drafted the manuscript along with the other authors. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
de Siqueira, K.C., de Lima, F.M., Lima, F.S. et al. miR-124a expression contributes to the monophasic pattern of insulin secretion in islets from pregnant rats submitted to a low-protein diet. Eur J Nutr 57, 1471–1483 (2018). https://doi.org/10.1007/s00394-017-1425-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1425-z