Abstract
Background
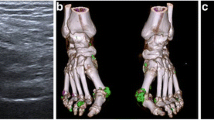
There are few data demonstrating the association between urate burden assessed by ultrasound (US) and gout flares. The aim of this study was to determine the association of urate deposition shown by US and frequent gout attacks.
Materials and methods
Patients with gout were divided into two groups according to the frequency of gout attacks in the previous 12 months: frequent (>2 attacks) and infrequent (0–2 attacks). Urate deposition in the hands, knees, and feet was assessed by US.
Results
Overall, 106 patients were enrolled in this study, of whom 32 (30.1%) had had frequent gout attacks (>2 attacks) in the previous 12 months (the average number of gout attacks was 4.7, range 3–12). Those with frequent gout attacks had significantly longer gout duration, a higher serum urate level, and more urate deposition shown by US than those with infrequent gout attacks (P < 0.05). In both univariate and logistic regression analyses, frequent gout attacks were correlated with gout duration, serum urate level, and urate deposition as shown by US (P < 0.05).
Conclusion
These findings indicate that urate deposition shown by US is independently associated with frequent gout attacks. Special attention should be given to the prevention of flares in patients with an initially high urate burden as assessed by US.
Zusammenfassung
Hintergrund
Es gibt nur wenige Daten zum Zusammenhang zwischen der sonographisch ermittelten Harnsäurebelastung und Gichtanfällen. Ziel der vorliegenden Studie war es, den Zusammenhang zwischen Ablagerungen von Harnsäurekristallen, die im Ultraschall (US) darstellbar sind, und häufigen Gichtanfällen zu untersuchen.
Material und Methoden
Patienten mit Gicht wurden je nach Häufigkeit ihrer Gichtanfälle in den letzten 12 Monaten in 2 Gruppen unterteilt: häufig (>2 Anfälle) und selten (0–2 Anfälle). Die Ablagerungen von Harnsäurekristallen in den Händen, Knien und Füßen wurden mittels US untersucht.
Ergebnisse
Es wurden 106 Patienten in die Studie aufgenommen, von denen 32 (30,1%) in den letzten 12 Monaten häufige Gichtanfälle (>2 Anfälle) gehabt hatten (die Durchschnittszahl der Gichtanfälle betrug 4,7; Spannbreite: 3–12). Bei den Patienten mit häufigen Gichtanfällen dauerten die Anfälle deutlich länger, bestand ein höherer Harnsäurespiegel und waren mehr Ablagerungen von Harnsäurekristallen im US nachweisbar als bei Patienten mit seltenen Gichtanfällen (p < 0,05). Sowohl in der univariaten als auch in der logistischen Regressionsanalyse waren häufige Gichtanfälle mit der Dauer der Gicht, dem Serumharnsäurespiegel und im US sichtbaren Ablagerungen von Harnsäurekristallen korreliert (p < 0,05).
Schlussfolgerung
Diese Ergebnisse zeigen, dass im US nachweisbare Ablagerungen von Harnsäurekristallen in unabhängiger Weise mit häufigen Gichtanfällen assoziiert sind. Besondere Aufmerksamkeit sollte der Prävention von Krankheitsausbrüchen bei Patienten mit initial hoher im US nachweisbarer Harnsäurebelastung gewidmet werden.


Similar content being viewed by others
References
Dalbeth N, Merriman TR, Stamp LK (2016) Gout. Lancet 388:2039–2052
Martinon F, Petrilli V, Mayor A et al (2006) Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature 440:237–241
Singh JA, Reddy SG, Kundukulam J (2011) Risk factors for gout and prevention: a systematic review of the literature. Curr Opin Rheumatol 23:192–202
Rothenbacher D, Primatesta P, Ferreira A et al (2011) Frequency and risk factors of gout flares in a large population-based cohort of incident gout. Rheumatology (Oxford) 50:973–981
Zhang Y, Chen C, Choi H et al (2012) Purine-rich foods intake and recurrent gout attacks. Ann Rheum Dis 71:1448–1453
Neogi T, Chen C, Niu J et al (2014) Alcohol quantity and type on risk of recurrent gout attacks: an internet-based case-crossover study. Am J Med 127:311–318
Abhishek A, Valdes AM, Zhang W et al (2016) Association of serum uric acid and disease duration with frequent gout attacks: a case-control study. Arthritis Care Res (Hoboken) 68:1573–1577
Richette P, Doherty M, Pascual E et al (2017) 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis 76:29–42
Kiltz U, Smolen J, Bardin T et al (2016) Treat-to-target (T2T) recommendations for gout. Ann Rheum Dis 76:632–638
Pascart T, Grandjean A, Capon B et al (2018) Monosodium urate burden assessed with dual-energy computed tomography predicts the risk of flares in gout: a 12-month observational study. MSU burden and risk of gout flare. Arthritis Res Ther 20:210
Dalbeth N, Nicolaou S, Baumgartner S et al (2018) Presence of monosodium urate crystal deposition by dual-energy CT in patients with gout treated with allopurinol. Ann Rheum Dis 77:364–370
Neogi T, Jansen TL, Dalbeth N et al (2015) Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheumatol 67(10):2557–2568
Grainger RHA, Taylor WJ (2005) Preliminary identification of potential items for a definition of ‘Gout Flare’ using Delphi methodology. Arthritis Rheum 52(Suppl 9):105
Proudman C, Lester SE, Gonzalez-Chica DA et al (2019) Gout, flares, and allopurinol use: a population-based study. Arthritis Res Ther 21:132
Shiozawa A, Szabo SM, Bolzani A et al (2017) Serum uric acid and the risk of incident and recurrent gout: a systematic review. J Rheumatol 44:388–396
Shiozawa A, Buysman EK, Korrer S (2017) Serum uric acid levels and the risk of flares among gout patients in a US managed care setting. Curr Med Res Opin 33:117–124
Stamp L, Morillon MB, Taylor WJ et al (2018) Serum urate as surrogate endpoint for flares in people with gout: a systematic review and meta-regression analysis. Semin Arthritis Rheum 48:293–301
Stamp LK, Morillon MB, Taylor WJ et al (2018) Variability in the reporting of serum urate and flares in gout clinical trials: need for minimum reporting requirements. J Rheumatol 45:419–424
Nuki G, Doherty M, Richette P (2017) Current management of gout: practical messages from 2016 EULAR guidelines. Pol Arch Intern Med 127:267–277
Eminaga F, La-Crette J, Jones A et al (2016) Does the initiation of urate-lowering treatment during an acute gout attack prolong the current episode and precipitate recurrent attacks: a systematic literature review. Rheumatol Int 36:1747–1752
Gutierrez M, Schmidt WA, Thiele RG et al (2015) International consensus for ultrasound lesions in gout: results of Delphi process and web-reliability exercise. Rheumatology (Oxford) 54:1797–1805
Elfishawi MM, Zleik N, Kvrgic Z et al (2020) Changes in the presentation of incident gout and the risk of subsequent flares: a population-based study over 20 years. J Rheumatol 47:613–618
Mak A, Ho RC, Tan JY et al (2009) Atherogenic serum lipid profile is an independent predictor for gouty flares in patients with gouty arthropathy. Rheumatology (Oxford) 48:262–265
Funding
This study was partly supported by the grants from the National Science Foundation of Zhejiang (LY19H100002) and 2019 Jiaxing Key Supporting Discipline of Medicine Rheumatology and Autoimmunology (2019-ZC-03).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Z. Zou, M. Yang, Y. Wang, and B. Zhang declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee (First Affiliated Hospital of Jiaxing University Ethics Committee) and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Zou, Z., Yang, M., Wang, Y. et al. Association of urate deposition shown by ultrasound and frequent gout attacks. Z Rheumatol 80, 565–569 (2021). https://doi.org/10.1007/s00393-020-00913-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-020-00913-0