Abstract
Objectives
Restless legs syndrome (RLS) is a neurological disease with a chronic course that is characterised by sleep disorders and sensorimotor impairment. The aim of this study was to evaluate the prevalence and severity of RLS in psoriatic arthritis (PSA) patients and those with psoriasis (P).
Patients and methods
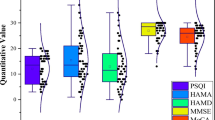
The study included 50 patients with psoriasis (28 females, 22 males), 50 PSA patients (33 females, 17 males) and 50 healthy control subjects (34 females, 16 males), and all 3 groups were matched with respect to age, gender and body mass index (BMI). Evaluations were made using the International RLS Rating Scale, Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale, Insomnia Severity Index, Fatigue Severity Scale (FSS), Beck Depression Index (BDI) and the SF-36 quality of life scores.
Results
RLS was determined at a higher rate in the PSA patients (64.0%), compared to the P group (20.0%, p < 0.001) and the control group (14.0%, p < 0.001). The number of moderate and severe RLS cases was significantly higher in the PSA group (68.7%) compared to the P group (30%, p < 0.001) and the control group (0%, p < 0.001). In regression analysis, an independent correlation was found between the RLS score and PSQI (beta [β] = 0.269, p = 0.002), FSS (β = 0.243, p = 0.003), SF-36 physical score (β = 0.242, p = 0.004) and BDI (β = 0.177, p = 0.036).
Conclusion
RLS was determined in PSA patients at a higher rate than in psoriasis patients. The presence of RLS in PSA and psoriasis patients is related to impairments in sleep and quality of life, fatigue and depression.
Zusammenfassung
Ziele
Das Restless-Legs-Syndrom (RLS) ist eine neurologische Krankheit mit einem chronischen Verlauf, die durch Schlafstörungen und sensomotorische Beeinträchtigungen gekennzeichnet ist. Ziel dieser Studie war es, die Prävalenz und Schwere des RLS bei Patienten mit Psoriasisarthritis (PSA) und Patienten mit Psoriasis (P) zu untersuchen.
Patienten und Methoden
Die Studie umfasste 50 Patienten mit Psoriasis (28 w., 22 m.), 50 PSA-Patienten (33 w., 17 m.) und 50 gesunde Kontrollpersonen (34 w., 16 m.), und alle 3 Gruppen wurden in Bezug auf Alter, Geschlecht und Body Mass Index (BMI) verglichen. Die Bewertungen erfolgten anhand der International RLS Rating Scale, des Pittsburgh Sleep Quality Index (PSQI), der Epworth Sleepiness Scale, des Insomnia Severity Index, der Fatigue Severity Scale (FSS), des Beck Depression Index (BDI) und der SF-36 Quality of Life Scores.
Ergebnisse
Die Häufigkeit eines RLS war bei den PSA-Patienten (64,0 %) größer als in der P-Gruppe (20,0 %; p < 0,001) und der Kontrollgruppe (14,0 %; p < 0,001). Die Anzahl der mittleren und schweren RLS-Fälle war in der PSA-Gruppe (68,7 %) signifikant höher als in der P-Gruppe (30 %; p < 0,001) und der Kontrollgruppe (0 %; p < 0,001). In der Regressionsanalyse wurde eine unabhängige Korrelation zwischen dem RLS-Score und PSQI (beta [β] = 0,269; p = 0,002), FSS (β = 0,243; p = 0,003), SF-36 – körperliche Funktion (β = 0,242; p = 0,004) und BDI (β = 0,177; p = 0,036) festgestellt.
Schlussfolgerung
Ein RLS wurde bei PSA-Patienten häufiger als bei Psoriasispatienten festgestellt. Das Vorhandensein eines RLS bei PSA- und Psoriasispatienten steht im Zusammenhang mit Beeinträchtigungen des Schlafs und der Lebensqualität, Müdigkeit und Depression.
Ein RLS wurde bei PSA-Patienten häufiger als bei Psoriasispatienten festgestellt. Das Vorhandensein eines RLS bei PSA- und Psoriasispatienten steht im Zusammenhang mit Beeinträchtigungen des Schlafs und der Lebensqualität, Müdigkeit und Depression.


Similar content being viewed by others
References
Parisi R, Symmons DP, Griffiths CE et al (2013) Identification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Globalepidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol 133:377–385
Albanesi C, Madonna S, Gisondi P et al (2018) The interplay between keratinocytes and immune cells in the pathogenesis of psoriasis. Front Immunol 9:1549
Pap T, Sunderkötter C (2017) Psoriasis vs. psoriatic arthritis: similarities and differences in the pathophysiology. Z Rheumatol 76:477–483
Liu JT, Yeh HM, Liu SY et al (2014) Psoriatic arthritis: epidemiology, diagnosis, and treatment. World J Orthop 5:537–543
Coates LC, Helliwell PS (2010) Disease measurement—enthesitis, skin, nails, spine and dactylitis. Best Pract Res Clin Rheumatol 24:659–670
Busse K, Liao W (2010) Which psoriasis patients develop psoriatic arthritis? Psoriasis Forum 16:17–25
Ogdie A, Gelfand JM (2015) Clinical risk factors for the development of psoriatic arthritis among patients with psoriasis: a review of available evidence. Curr Rheumatol Rep 17:64
Garcia-Borreguero D, Cano-Pumarega I (2017) New concepts in the management of restless legs syndrome. BMJ 356:j104
Manconi M, Ulfberg J, Berger K et al (2012) When gender matters: restless legs syndrome. Report of the “RLS and woman” workshop endorsed by the European RLS Study Group. Sleep Med Rev 16:297–307
Bogan RK, Cheray JA (2013) Restless legs syndrome: a review of diagnosis and management in primary care. Postgrad Med 125:99–111
Mucsi I, Molnar MZ, Ambrus C et al (2005) Restless legs syndrome, insomnia and quality of life in patients on maintenance dialysis. Nephrol Dial Transplant 20:571–577
Giannaki CD, Hadjigavriel M, Lazarou A et al (2017) Restless legs syndrome is contributing to fatigue and low quality of life levels in hemodialysis patients. World J Nephrol 6:236–242
Schell C, Schleich R, Walker F et al (2015) Restless legs syndrome in psoriasis: an unexpected comorbidity. Eur J Dermatol 25:255–260
Temel AB, Karaman NS, Bozkurt S et al (2016) Prevalence of restless legs syndrome among psoriasis patients and association with depression and sleep quality. Turk J Dermatol 10:110–115
Kucuk A, Uslu AU, Yilmaz R et al (2017) Relationship between prevalence and severity of restless legs syndrome and anemia in patients with systemic lupus erythematosus. Int J Rheum Dis 20:469–473
Gupta MA, Simpson FC, Gupta AK (2016) Psoriasis and sleep disorders: a systematic review. Sleep Med Rev 29:63–75
Gezer O, Batmaz I, Sariyildiz MA et al (2017) Sleep quality in patients with psoriatic arthritis. Int J Rheum Dis 20:1212–1218
Duffin KC, Wong B, Krueger G (2009) Sleep disturbance and medical comorbidities in patients with psoriasis, psoriatic arthritis, and controls. J Am Acad Dermatol 1:AB9
Taylor W, Gladman D, Helliwell P et al (2006) Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 54:2665–2673
Allen RP, Picchietti D, Hening WA et al (2003) Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the national institutes of health. Sleep Med 4:101–119
Walters AS, LeBrocq C, Dhar A et al (2003) Validation of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med 4:121–132
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Beck AT, Ward CH, Mehdelson M et al (1961) An inventory for measuring depresssion. Arch Gen Psychiatry 4:561–571
Johns MWA (1991) New method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Buysse DJ, Reynolds CF, Monk TH et al (1991) Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep 14:331–338
Bastien CH, Vallières A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2:297–307
Valko PO, Bassetti CL, Bloch KE et al (2008) Validation of the fatigue severity scale in a Swiss cohort. Sleep 31:1601–1607
Jiménez-Jiménez FJ, Alonso-Navarro H, García-Martín E et al (2018) Genetics of restless legs syndrome: An update. Sleep Med Rev 39:108–121
Ferré S, García-Borreguero D, Allen RP et al (2018) New insights into the neurobiology of restless legs syndrome. Neuroscientist. https://doi.org/10.1177/1073858418791763
Guo S, Huang J, Jiang H et al (2017) Restless legs syndrome: from pathophysiology to clinical diagnosis and management. Front Aging Neurosci 9:171
Weinstock LB, Walters AS, Paueksakon P (2012) Restless legs syndrome—theoretical roles of inflammatory and immune mechanisms. Sleep Med Rev 16:341–354
Taylor-Gjevre RM, Gjevre JA, Nair BV (2014) Increased nocturnal periodic limb movements in rheumatoid arthritis patients meeting questionnaire diagnostic criteria for restless legs syndrome. BMC Musculoskelet Disord 18(15):378
Gjevre JA, Taylor Gjevre RM (2013) Restless legs syndrome as a comorbidity in rheumatoid arthritis. Autoimmune Dis 2013:352782
Ishaq M, Muhammad JS, Hameed K (2013) Risk of restless legs syndrome in low socioeconomic rheumatoid arthritis patients. Mod Rheumatol 23:705–708
Ediz L, Hiz O, Toprak M et al (2011) Restless legs syndrome in Behçet’s disease. J Int Med Res 39:759–765
Tekatas A, Pamuk ON (2015) Increased frequency of restless leg syndrome in patients with ankylosing spondylitis. Int J Rheum Dis 18:58–62
Feld J, Chandran V, Haroon N (2018) Axial disease in psoriatic arthritis and ankylosing spondylitis: a critical comparison. Nat Rev Rheumatol 14:363–371
Ferreira BR, Pio-Abreu JL, Reis JP et al (2017) Analysis of the prevalence of mental disorders in psoriasis: the relevance of psychiatric assessment in dermatology. Psychiatr Danub 29:401–406
Cicek D, Halisdemir N, Dertioglu SB et al (2012) Increased frequency of restless legs syndrome in atopic dermatitis. Clin Exp Dermatol 37:469–476
Winkelman JW, Redline S, Baldwin CM et al (2009) Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep 32:772–778
Wong ITY, Chandran V, Li S et al (2017) Sleep disturbance in psoriatic disease: prevalence and associated factors. J Rheumatol 44:1369–1374
Henry AL, Kyle SD, Chisholm A et al (2017) A cross-sectional survey of the nature and correlates of sleep disturbance in people with psoriasis. Br J Dermatol 177:1052–1059
Henry AL, Kyle SD, Bhandari S et al (2016) Measurement, classification and evaluation of sleep disturbance in psoriasis: a systematic review. PLoS ONE 11:e157843
Callis Duffin K, Wong B, Horn EJ et al (2009) Psoriatic arthritis is a strong predictor of sleep interference in patients with psoriasis. J Am Acad Dermatol 60:604–608
Güler S, Tekatas A, Arican O et al (2015) Restless legs syndrome and insomnia frequency in patients with psoriasıs. Ideggyogy Sz 68:331–336
Akdag Uzun Z, Kurt S, Karaer Unaldi H (2018) The relationship with restless legs syndrome, fibromyalgia, and depressive symptoms in migraine patients. Neurol Sci 39:1409–1414
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. C. Sandikci, S. Colak, R. Aydoğan Baykara, A. Öktem, E. Cüre, A. Omma and A. Kucuk declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Redaktion
U. Müller-Ladner, Bad Nauheim
U. Lange, Bad Nauheim
Rights and permissions
About this article
Cite this article
Sandikci, S.C., Colak, S., Aydoğan Baykara, R. et al. Evaluation of restless legs syndrome and sleep disorders in patients with psoriatic arthritis. Z Rheumatol 78, 987–995 (2019). https://doi.org/10.1007/s00393-018-0562-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00393-018-0562-y