Abstract
Background
Ferritin is commonly used to evaluate iron stores and guide therapeutic decisions regarding intravenous iron supplementation. However, in the context of AHF, inflammation-driven upregulation of ferritin might disrupt its correlation with iron stores, restricting iron bioavailability and potentially amplifying the inflammatory response.
Aim
This study aims to assess the clinical and prognostic associations of ferritin levels in an AHF cohort and to determine whether the prognostic value of ferritin is influenced by the presence of infection, inflammatory activation, and other markers of iron deficiency.
Methods
The association between ferritin and clinical outcomes (180 days) in AHF was evaluated in a cohort of 526 patients from the EDIFICA registry.
Results
The median ferritin plasma concentration at admission was 180 pg/mL. Patients with higher ferritin levels at admission were predominantly men, exhibiting a high prevalence of chronic kidney disease and alcohol consumption, and presenting with lower blood pressure and a higher incidence of clinical infection. Higher ferritin levels were associated with increased risk of the composite of heart failure hospitalization or cardiovascular death (Tertile 2: HR 1.75; 95% CI 1.10–2.79; p = 0.017; Tertile 3: HR 1.79; 95% CI 1.08–2.97; p = 0.025), independently of classical HF prognostic factors, inflammatory and iron-related markers. No significant associations were found between admission serum iron or transferrin saturation tertiles, iron status categories, or guideline-defined iron deficiency (ID) criteria and the primary composite outcome. However, at discharge, patients who met the criteria for defective iron utilization, low iron storage, or guideline-defined ID had a lower risk of the composite endpoint compared to those with normal iron utilization or who did not meet the guideline-defined ID criteria, respectively.
Conclusions
Elevated ferritin levels are independently associated with poor prognosis in AHF. Low ferritin levels are associated with a favorable outcome and do not carry significant value in identifying ID in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute heart failure (AHF) stands as a leading cause of unplanned hospitalization and portends a poor prognosis [1]. Inflammatory activation is frequently observed in AHF patients, either due to infectious triggers leading to HF decompensation (e.g., respiratory infection) or as a result of exacerbation of HF alongside comorbid conditions (e.g., worsening of renal function) [2, 3].
Ferritin is a central regulator of intracellular iron levels and its plasma concentrations are widely used for assessing the body iron stores, particularly for establishing the diagnosis of iron deficiency (ID) and making treatment decisions regarding the administration of IV iron therapy [1, 4, 5]. However, in inflammatory conditions, ferritin levels are highly upregulated independently of iron status [6]. Consequently, within the context of AHF, high-ferritin levels might primarily indicate the presence of inflammatory activation rather than excluding ID. Despite this theoretical background, there is insufficient evidence on the relationship between ferritin, markers of ID and clinical outcomes in AHF.
Aims
To evaluate the clinical and prognostic associations of ferritin levels (both at hospital admission and discharge) in an AHF cohort. Assess whether the prognostic value of ferritin is influenced by the presence of infection, inflammatory activation, and biomarkers of iron deficiency. Lastly, we aim to discuss the potential implications of the use of ferritin for the criteria of ID and iron replacement therapy in AHF.
Methods
The EDIFICA registry (“Estratificação de Doentes com InsuFIciência Cardíaca Aguda”) is a single-center, prospective cohort study, conducted during a 21-month period at the Internal Medicine Department of Centro Hospitalar Universitário São João, Porto, Portugal [2, 7]. Patients admitted with the primary diagnosis of AHF were eligible for registry inclusion. Patients with acute coronary syndromes and those whose symptoms were explained by conditions other than HF were excluded from this registry. All patients underwent detailed clinical history, physical examination, and venous blood sample analysis at admission and discharge. An echocardiogram was performed within 72 h after admission. The investigation conformed with the principles outlined in the Declaration of Helsinki and was approved by the local ethics committee. Admission (N = 526) and discharge (N = 396) ferritin levels were evaluated using an immunoturbidimetric assay (OSR61203; Beckman Coulter).
Categorical variables are described as frequencies (proportions), and continuous variables are expressed as means ± standard deviation or median (25th and 75th percentiles), depending on their distributions. Comparisons of demographic, clinical, and biological parameters among tertiles of ferritin levels, iron status [8] and guideline-defined iron deficiency criteria [1] were analyzed using analysis of variance (ANOVA) for continuous normally distributed variables, the analogous non-parametric Kruskal–Wallis test for continuous non-normally distributed variables, and Chi-squared test (χ2) for categorical variables. The primary endpoint was a composite of heart failure hospitalization (HFH) or cardiovascular death (CVD). Cox proportional hazards regression models were used to assess the association between ferritin levels and the clinical endpoints, adjusting for sex, age, atrial fibrillation, NYHA class at admission, eGFR (CKD-EPI formula), clinical infection and circulating levels of B-type natriuretic peptide (BNP, log2), transferrin saturation (TSAT, log2), hemoglobin, albumin, total cholesterol, and C-reactive protein (CRP, log2). All statistical analyses were performed with Stata® (StataCorp. 2021. Stata Statistical Software: Release 18.0. College Station, TX: StataCorp LLC). A 2-sided value of p<0.05 was considered statistically significant.
Results
The median age was 78 (IQR 71–84) years, and 227 (43%) patients were men. Median ejection fraction was 41%, 228 (43%) patients had an ejection fraction ≤ 40% and 40% of the patients had HF of ischemic etiology. Median ferritin plasma concentration was 180 pg/mL (percentile25-75 74–312 pg/mL) at admission and 197 pg/mL (percentile25-75 108–346 pg/mL) at discharge.
Table 1 presents patient characteristics, demographic data, and analytical parameters by tertiles of ferritin levels at admission. Patients in the highest tertile of ferritin at admission (Tertile 3: 421 [312–611] pg/mL) were predominantly men, with a high prevalence of chronic kidney disease and alcohol consumption and presenting with lower blood pressure and a high incidence of clinical infection. On the other hand, patients with lower ferritin levels (Tertile 1: 57 [36–74] pg/mL) used beta-blockers and loop diuretics less frequently and had higher rate of atrial fibrillation. No differences were observed between ferritin tertiles regarding age, HF disease-modifying treatment (e.g., ACEi, ARB or MRAs), circulating BNP and troponin or classical cardiovascular risk factors such as anemia, diabetes and hypertension. Increased ferritin correlated with higher mean corpuscular volume, TSAT, urea, C-reactive protein, and lower red blood cell distribution width and transferrin concentration. These associations remained consistent when discharge ferritin tertiles were analyzed (Table S1).
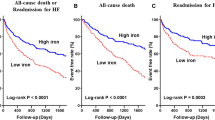
Table 2 shows the association between admission ferritin levels and clinical outcomes. Higher ferritin levels (Tertiles 2 and 3) were independently associated with increased risk of the composite of HFH or cardiovascular death (Tertile 2: HR 1.75; 95% CI 1.10–2.79; p = 0.017; Tertile 3: HR 1.79; 95% CI 1.08–2.97; p = 0.025) (Fig. 1). This association remained consistent across all subgroups, including among patients presenting with clinical infection (Table 3). Similar, though less strong, associations were observed when analyzing discharge ferritin tertiles (Table S2 and Fig. S1) or applying guideline-defined ID criteria ferritin cutoffs (Table S3 and Fig. S2). Patient characteristics based on admission and discharge iron status and guideline-defined ID criteria ferritin cutoffs are additionally displayed in the supplemental data (Tables S4 and S5).
Admission ferritin levels and acute heart failure outcomes. A Kaplan–Meier analysis for 180-day composite endpoint of HF hospitalization or cardiovascular death, stratified by tertiles of admission ferritin. B Spline curve for the composite endpoint of HF hospitalization and cardiovascular death across the range of admission ferritin values (log2). The hazard ratio is depicted by a green line, accompanied by overlaid 95% confidence intervals (green shadow) alongside an admission ferritin histogram (red bars)
No significant associations were found between admission serum iron or TSAT tertiles, iron status categories, or guideline-defined iron deficiency criteria and the primary composite outcome (Table 4). Contrastingly, at discharge, intermediate tertiles of serum iron (Tertile 2: 53 [42–68] μg/mL) and TSAT (Tertile 2: 15.5 [11.8–20.2] %) demonstrated a decreased risk of the primary composite endpoint when compared to those in the highest tertile (Tertile 3), which encompasses the ‘normal range’ (Table S6). Accordingly, patients who met the criteria at discharge for defective iron utilization and low iron storage, or the guideline-defined ID criteria, had a lower risk of the primary composite endpoint compared to those with normal iron utilization and those who did not meet the guideline-defined ID criteria, respectively (Table S6).
Comparison of multiple established iron deficiency-related cutoffs revealed increased circulating levels of ferritin, transferrin saturation, and serum iron at discharge, alongside a decreased prevalence of anemia, compared with admission (Table S7).
Conclusion
In this study, we show that higher ferritin levels are associated with worse clinical outcomes, independently of key HF prognostic factors, iron-related factors and inflammatory markers, suggesting potential ferritin-dependent mechanisms of HF decompensation [9, 10]. Importantly, our data also indicate that in the inflammatory context of AHF, measuring ferritin, serum iron, or transferrin saturation may not reliably assess iron status, challenging the validity of current guideline-defined criteria for identifying ID in this clinical setting.
Inflammation plays a central role in the pathogenesis and prognosis of AHF, as evidenced by the high prognostic value of inflammatory markers [2]. Ferritin expression is markedly upregulated by inflammatory signaling and is associated with adverse outcomes across a broad range of cardiovascular, infectious, immunological, and malignant disorders [6, 11, 12]. Interestingly, in inflammatory states, particularly during infection, ferritin upregulation has been perceived as protective, as it restricts iron availability to pathogens and attenuates iron-mediated oxidative stress [6]. However, experimental data suggests a potential dual role of ferritin, as it can also apparently function as a cytokine, increasing inflammatory transcriptional activity [13]. Furthermore, within the context of AHF, the impairment of iron bioavailability can negatively impact on myocardial bioenergetics and function [14].
Importantly, categorization by iron status and guideline-defined ID criteria at discharge identified patients at lower, instead of higher, risk of clinical events. These results suggest that AFFIRM-AHF [15] and IRONMAN [16] trials, by selecting a low-ferritin AHF population, may have targeted a low-inflammation population including patients potentially lacking ID. Simultaneously, these trials may have excluded patients with ID and high inflammatory activity, who could have potentially benefited from the treatment outside the hyperinflammatory phase. While it is seems reasonable to exclude patients with a confirmed or suspected active infection from IV iron therapy [17, 18], it is important to acknowledge that AHF itself represents an inflammatory condition and high-ferritin patients may still benefit from IV supplementation. Supporting this hypothesis, a secondary analysis from the IRONMAN trial recently revealed that patients with higher ferritin (i.e., > 100 ng/mL) had worse outcome but showed a greater response to IV iron therapy [19].
Transferrin saturation or serum iron concentration were recently shown to outperform guideline-defined criteria in predicting HF-related mortality and may serve as viable alternatives [12, 19, 20]. However, caution should be exercised when applying cutoffs derived from chronic HF cohorts to the inflammatory setting of AHF, as our analysis suggest pre-discharge levels below these cutoffs (e.g. TSAT < 20%) may offer some protection. In addition, the negative correlation between inflammation and transferrin may complicates the use classical ID criteria in high-ferritin states, such as AHF [21]. In this regard, soluble transferrin receptor, which has been shown to accurately reflect iron stores and independently predict HF outcomes [22, 23], could potentially improve the assessment of iron status in AHF, but further studies are needed to confirm its utility in this setting.
In conclusion, in patients with AHF, elevated ferritin levels are associated with poor prognosis, independently of classical HF prognosticators and inflammatory markers. Low ferritin levels are associated with a favorable outcome and may not hold significant value in identifying ID in this population.
References
Members AF et al (2022) 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail 24:4–131
Vasques-Nóvoa F et al (2022) Interleukin-6, infection and cardiovascular outcomes in acute heart failure: findings from the EDIFICA registry. Cytokine 160:156053
Arrigo M et al (2020) Acute heart failure. Nat Rev Dis Primers 6:1–15
Lindberg F et al (2023) Iron deficiency in heart failure: screening, prevalence, incidence and outcome data from the Swedish Heart Failure Registry and the Stockholm Creatinine Measurements collaborative project. Eur J Heart Fail 25:1270–1280
Marques P et al (2023) Erythropoietic response after intravenous iron in patients with heart failure and reduced ejection fraction with and without background treatment with sodium-glucose cotransporter 2 inhibitors. Eur J Heart Fail. https://doi.org/10.1002/ejhf.2992
Kernan KF, Carcillo JA (2017) Hyperferritinemia and inflammation. Int Immunol 29:401–409
Pintalhao M et al (2017) Relaxin serum levels in acute heart failure are associated with pulmonary hypertension and right heart overload. Eur J Heart Fail 19:218–225
Grote Beverborg N et al (2019) Differences in clinical profile and outcomes of low iron storage vs defective iron utilization in patients with heart failure: results from the DEFINE-HF and BIOSTAT-CHF studies. JAMA Cardiol 4:696–701
Klip IJT et al (2017) Serum ferritin and risk for new-onset heart failure and cardiovascular events in the community. Eur J Heart Fail 19:348–356
Silvestre OM et al (2017) Ferritin levels and risk of heart failure - the atherosclerosis risk in communities study. Eur J Heart Fail 19:340–347
Cleland JGF et al (2016) Prevalence and outcomes of anemia and hematinic deficiencies in patients with chronic heart failure. JAMA Cardiol 1:539
Masini G et al (2022) Criteria for iron deficiency in patients with heart failure. J Am Coll Cardiol 79:341–351
Ruddell RG et al (2009) Ferritin functions as a proinflammatory cytokine via iron-independent protein kinase C zeta/nuclear factor kappaB-regulated signaling in rat hepatic stellate cells. Hepatology 49:887–900
Zhang H, Zhabyeyev P, Wang S, Oudit GY (2019) Role of iron metabolism in heart failure: from iron deficiency to iron overload. Biochimica et Biophysica Acta (BBA)-Mol Basis Dis 1865:1925–1937
Ponikowski P et al (2020) Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet 396:1895–1904
Kalra PR et al (2022) Intravenous ferric derisomaltose in patients with heart failure and iron deficiency in the UK (IRONMAN): an investigator-initiated, prospective, randomised, open-label, blinded-endpoint trial. Lancet 400:2199–2209
Shah AA et al (2021) Risk of infection associated with administration of intravenous iron: a systematic review and meta-analysis. JAMA Netw Open 4:e2133935
Lan P et al (2018) High serum iron level is associated with increased mortality in patients with sepsis. Sci Rep 8:11072
Cleland JGF et al (2024) Intravenous iron for heart failure, iron deficiency definitions, and clinical response: the IRONMAN trial. Eur Heart J 45:1410–1426
Packer M et al (2024) Redefining iron deficiency in patients with chronic heart failure. Circulation 150:151–161
Graham FJ et al (2023) Influence of serum transferrin concentration on diagnostic criteria for iron deficiency in chronic heart failure. ESC Heart Fail 10:2826–2836
Sierpinski R et al (2021) High soluble transferrin receptor in patients with heart failure: a measure of iron deficiency and a strong predictor of mortality. Eur J Heart Fail 23:919–932
Kang M et al (2022) Soluble transferrin receptor can predict all-cause mortality regardless of anemia and iron storage status. Sci Rep 12:11911
Funding
Open access funding provided by FCT|FCCN (b-on). This study was funded by national funds through FCT—Portuguese Foundation for Science and Technology, under the scope of the Cardiovascular R&D Center—UnIC (UIDB/00051/2020 and UIDP/00051/2020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have nothing to disclose.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vasques-Nóvoa, F., Pimentel, M.J., Marques, P. et al. Ferritin, inflammation, and iron deficiency in acute heart failure: evidence from the EDIFICA cohort. Clin Res Cardiol (2024). https://doi.org/10.1007/s00392-024-02535-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-024-02535-x