Abstract
Aim
Data on associations of invasively determined hemodynamic parameters with procedural success and outcomes in patients suffering from mitral regurgitation (MR) undergoing transcatheter edge-to-edge repair of the mitral valve (M-TEER) is limited.
Methods and results
We enrolled 239 patients with symptomatic MR of grade 2 + , who received M-TEER. All patients underwent extensive pre-interventional invasive hemodynamic measurements via right heart catheterization (mean pulmonary arterial pressure (mPAP), systolic- (PAPsys) and diastolic pulmonary arterial pressure (PAPdia), pulmonary arterial wedge pressure (PAWP), a-wave, v-wave, pulmonary vascular resistance (PVR), transpulmonary pressure gradient (TPG), cardiac index (CI), stroke volume index (SVI)). mPAP and PAWP at baseline were neither associated with procedural success, immediate reduction of MR, nor residual MR after 6 months of follow-up. The composite outcome (All-cause mortality (ACM) and/or heart failure induced rehospitalization (HFH)) and HFH differed significantly after M-TEER when stratified according to mPAP, PAWP, PAPdia, a-wave and v-wave. ACM was not associated with the afore mentioned parameters. Neither PVR, TPG, CI nor SVI were associated with the composite outcome and HFH, respectively. In multivariable analyses, PAWP was independently associated with the composite outcome and HFH. PVR and SVI were not associated with outcomes.
Conclusion
PAWP at baseline was significantly and independently associated with HFH and might serve as a valuable parameter for identifying patients at high risk for HFH after M-TEER. ACM and procedural success were not affected by pulmonary arterial pressure before M-TEER. We suggest that the post-capillary component of PH serves as the driving force behind the risk of HFH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transcatheter edge-to-edge repair of the mitral valve (M-TEER) has emerged as a safe and less invasive therapeutic alternative in patients with severe mitral regurgitation and at high-risk for surgical mitral valve repair [1,2,3,4]. M-TEER is an effective intervention for both primary and secondary mitral valve regurgitation (MR) [1, 4].
Pulmonary hypertension (PH), atrial fibrillation and left ventricular dysfunction are strong predictors of perioperative risk and presence of these co-morbidities worsen prognosis [5].
MR is known to cause PH by chronically increasing the mean left atrial pressure and thereby increasing the filling pressures in the pulmonary circulation. Chronic pulmonary venous congestion leads to fibrotic remodeling of the vessels via vasoconstriction and vascular remodeling, resulting in a further increase in resistance and pressure. Subsequent right ventricular dilation and dysfunction leads to tricuspid valve regurgitation. The resulting postcapillary PH is the most common form of PH [6].
Post-capillary PH, which can be either isolated (IpcPH) or combined with a significant pre-capillary component (CpcPH), is defined by a mPAP > 20 mmHg and a PAWP > 15 mmHg. Pulmonary vascular resistance (PVR) is used to distinguish between IpcPH (PVR ≤ 2 Wood units (WU)) and CpcPH (PVR > 2 WU). Pre-capillary PH is defined by mPAP > 20 mmHg, PAWP ≤ 15 mmHg and PVR > 2 WU [6].
Higher pulmonary arterial pressure (PAP) at baseline is associated with higher long-term mortality when compared to lower PAP in patients undergoing M-TEER [7,8,9,10]. However, most studies are based on systolic pulmonary artery pressure (sPAP) obtained by echocardiography [8,9,10]. Data on invasive hemodynamic measurements in patients who suffered from MR and underwent M-TEER is limited, especially regarding the differentiation of pulmonary hypertension into pre-capillary PH, IpcPH and CpcPH, respectively. Understanding the influence of PH on the outcomes of M-TEER procedures is crucial for optimizing patient selection, procedural planning, and post-procedural care.
Here, we aimed to evaluate associations of invasively determined PAP and its components (mean pulmonary arterial pressure (mPAP), systolic pulmonary arterial pressure (PAPsys), diastolic pulmonary arterial pressure (PAPdia), pulmonary arterial wedge pressure (PAWP), a-wave, v-wave, pulmonary vascular resistance (PVR), transpulmonary pressure gradient (TPG), cardiac index (CI) and stroke volume index (SVI)) with procedural success and clinical outcomes in patients undergoing M-TEER.
Methods
Patient cohort
This is a retrospective monocenter study. We consecutively enrolled 239 patients with symptomatic, higher grade mitral valve regurgitation (MR) that were admitted to the Department of Cardiology and Angiology of the University Hospital of Tübingen, Germany, for M-TEER between January 2010 and February 2016 [11]. All echocardiographic parameters in this study were originally assessed in the echocardiographic laboratory of the University Hospital of Tübingen [12,13,14]. Patients suffered from ischemic or nonischemic heart failure with a left ventricular ejection fraction (LVEF, %) from 15 to 60%. Patients had grade 2 + to grade 4 [1, 8, 15] primary and/or secondary MR and remained symptomatic (New York Heart Association [NYHA] functional class II, III, or IV) despite treatment with stable maximal doses of guideline-directed medical therapy and cardiac resynchronization therapy (if appropriate). All patients underwent right heart catheterization prior to M-TEER. Patients were assessed by a heart team that consisted of a heart-failure specialist, an interventional cardiologist, a cardiothoracic surgeon with expertise in mitral-valve disease and an anesthesiologist with experience in heart failure and cardiac surgery. [16] All patients were treated with the MitraClip® device (Abbott, North Chicago, Illinois, USA). mPAP, PAPsys, PAPdia, PAWP, a-wave, v-wave, PVR, TPG, CI and SVI [17] were determined via right heart catheterization prior to M-TEER [18]. PAWP was measured including v-wave and assessed end-expiratory. We sub-categorized pulmonary hypertension according to the “ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension” as mentioned previously. When PVR (cut-off > 2 WU for pre-capillary PH and CpcPH) [6] was not available, we applied the diastolic pressure gradient (DPG) as well as the transpulmonary pressure gradient (TPG) to differentiate between isolated post-capillary PH (DPG < 7 mmHg, TPG ≤ 12 mmHg) and combined post- and pre-capillary PH (DPG ≥ 7 mmHg, TPG > 12 mmHg) [19, 20]. Most patients gave written informed consent, and for those where it could not be obtained due to logistic issues, the institutional ethics committee approved retrospective data analysis. The study was approved by the ethics committee of the University of Tübingen (270/2011BO1, 237/2018BO2 and 187/2023BO2 respectively). The study complies with the declaration of Helsinki and the good clinical practice guidelines.
Right heart catheterization
Right heart catheterization was performed via femoral access. A sheath was placed into the femoral vein using Seldinger technique. Then, a Swan-Ganz catheter was passed into the right atrium, the right ventricle and the pulmonary artery using standard manipulations under fluoroscopic control. PAP was recorded, and the catheter was advanced until it plugged a branch of one of the pulmonary arteries and the waveform changed to a PAWP. The catheter was then withdrawn and pressures in the pulmonary arteries, the right ventricle and the right atrium were measured sequentially in resting expiratory position.
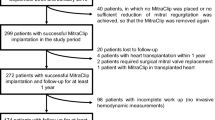
Survival outcomes and prognostic associations
All patients were followed up for 360 days for a primary composite clinical outcome consisting of all-cause mortality (ACM) and/or HFH. Secondary outcomes consisted of the single events ACM or HFH. 25 patients (10.5%) were lost to clinical follow-up. Follow-up echocardiography was performed in 205 patients (85.8%). Only patients with clinical follow-up were included into outcome analyses. We additionally analyzed a best-case (all patients lost to follow-up survived without events) and a worst-case scenario (all patients lost to follow-up suffered from hospitalization due to heart failure and/or deceased). Observed statistical significances between investigated groups did not change substantially when reanalyzed using these approaches.
Statistical analyses
All statistical analyses were performed with SPSS version 27.0 (IBM, USA) and GraphPad Prism software (GraphPad Software, Inc. USA) as previously described [21]. Non-normally distributed data are presented as median with interquartile range (IQR) or count and percentage as appropriate. Kruskal–Wallis-tests (H-tests) were applied as appropriate to analyze differences between more than two groups. Cox proportional hazard (PH) regression analyses with forward variable selection were applied to investigate associations between survival outcomes and hemodynamic parameters, using clinical factors as covariables. The time-dependent covariate method was used to check the proportional hazard assumption of the model. Survival functions were estimated by Kaplan–Meier curves. The log-rank test was applied to compare survival functions. All statistical tests were two-tailed and statistical significance level was defined as p < 0.05.
Results
Baseline characteristics
The study flow chart is presented in Fig. 1. Baseline characteristics of the complete clinical cohort stratified according to mPAP quartiles are presented in Table 1. We enrolled 239 patients affected by primary, secondary or combined MR. Of note, in one patient, only PAWP was available. Therefore, Table 1 shows 238 patients. The median age was 78 years, 37.8% were women, 55.5% had degenerative MR, and 85.7% had 3 + MR. Patients with higher mPAP were younger and suffered more often from mild aortic stenosis as well as cardiomyopathies and were more likely to have cardiac resynchronization therapy (CRT). Creatinine levels were higher; however, renal replacement therapy was evenly distributed. Prevalence of concomitant TR, which is related to mPAP and PVR, did not differ significantly between patient groups.
Procedural success
The MitraClip® procedure was completed in all patients. After M-TEER, MR was reduced to mild or less in 200 patients (83.7%), to moderate in 33 patients (13.8%) while there was no relevant reduction of MR in 6 patients (2.5%). After 6 months of follow-up, 134 patients had MR of mild or less severity (65.4%), 61 patients had moderate MR (29.8%) whereas 10 patients hat severe MR (4.9%). MR grade IV at baseline was associated with higher mPAP (3rd and 4th quartile) before M-TEER. Immediate reduction of MR and success of the procedure (MR < grade 2) were not associated with hemodynamic parameters before M-TEER (Table 2, Fig. 2).
Good procedural result (MR < grade 2) immediately after M-TEER and at 6-months follow-up stratified according to mPAP and PAWP at baseline. A and C: MR < grade 2 (%) immediately after M-TEER. B and D: MR < grade 2 (%) after 6 months of follow-up. mPAP Q1 < 24, mPAP Q2 ≥ 24 < 30, mPAP Q3 ≥ 30 < 37, mPAP Q4 ≥ 37 mmHg. PAWP Q1 < 12, PAWP Q2 ≥ 12 < 18, PAWP Q3 ≥ 18 < 25, PAWP Q4 ≥ 25 mmHg. Abbreviations: mPAP, mean pulmonary arterial pressure; MR, mitral valve regurgitation; M-TEER, transcatheter edge-to-edge repair of the mitral valve; PAWP, pulmonary arterial wedge pressure; Q, quartile.
Outcomes
All-cause mortality did not differ significantly after the MitraClip® procedure stratified according to hemodynamic parameters before M-TEER. The composite outcome and HFH were, however, significantly associated with mPAP, PAWP, PAPdia, a-wave and v-wave, respectively. Of note, neither PVR, TPG, CI nor SVI were associated with the composite outcome, ACM and HFH, respectively (Table 3 and Figs. 3 and 4). Range of hemodynamic parameters in quartiles 1–4 is presented in Table 3. While the incidence of HFH was higher in the 3rd and 4th mPAP quartile at baseline when compared to the 1st and 2nd quartile, PAWP showed a linear trend towards higher pressure being associated with HFH. In multivariable analyses, PAWP at baseline remained independently associated with the composite outcome and HFH after adjustment for covariates (Table 4).
Kaplan–Meier estimates showing composite outcome (A, B) and ACM (C, D) stratified according to mPAP and PAWP at baseline. mPAP Q1 < 24, mPAP Q2 ≥ 24 < 30, mPAP Q3 ≥ 30 < 37, mPAP Q4 ≥ 37 mmHg. PAWP Q1 < 12, PAWP Q2 ≥ 12 < 18, PAWP Q3 ≥ 18 < 25, PAWP Q4 ≥ 25 mmHg. Abbreviations: ACM, all-cause mortality; mPAP, mean pulmonary arterial pressure; PAWP, pulmonary arterial wedge pressure; Q, quartiles.
Kaplan–Meier estimates showing HFH stratified according to mPAP (A), PAWP (B), PVR (C) and SVI (D), respectively, at baseline. mPAP Q1 < 24, mPAP Q2 ≥ 24 < 30, mPAP Q3 ≥ 30 < 37, mPAP Q4 ≥ 37 mmHg. PAWP Q1 < 12, PAWP Q2 ≥ 12 < 18, PAWP Q3 ≥ 18 < 25, PAWP Q4 ≥ 25 mmHg. PVR Q1 < 1.8, PVR Q2 ≥ 1.8 < 2.7, PVR Q3 ≥ 2.7 < 4.3, PVR Q4 ≥ 4.3 WU. SVI Q1 < 23.7, SVI Q2 ≥ 23.7 < 31.3, SVI Q3 ≥ 31.3 < 41.8, SVI Q4 ≥ 41.8 ml/m2. Abbreviations: HFH, heart failure induced rehospitalization; mPAP, mean pulmonary arterial pressure; PAWP, pulmonary arterial wedge pressure; PVR, pulmonary vascular resistance; Q, quartiles; SVI, stroke volume index
Classification of PH
205 patients suffered from pulmonary hypertension (85.8%). Out of these patients, 59 (28.8%) suffered from pre-capillary PH, 53 (25.9%) from IpcPH and 91 (44.4%) from CpcPH. Within these subgroups, 2 patients without PH (6.7%), 8 patients with pre-capillary PH (15.7%), 13 patients with IpcPH (26.5%) and 26 patients with combined CpcPH (31.0%) were hospitalized due to heart failure. Of note, neither PVR nor TPG were associated with outcomes whereas parameters suggestive of left heart disease such as v-wave and PAWP were. Hence, we suggest that the post-capillary component of pulmonary hypertension serves as the driving force behind the risk of recurrent hospitalization due to heart failure.
A limitation of the current study is incomplete data on PVR. Hence, we provide data on patients with PVR available in the supplementary material.
Discussion
The current study revealed that (1) pulmonary arterial pressure before M-TEER was neither associated with procedural success nor reduction of mitral regurgitation after M-TEER. (2) Pulmonary arterial wedge pressure at baseline was significantly and independently associated with the composite outcome and heart failure induced rehospitalization after M-TEER. (3) Pulmonary arterial pressure was not associated with all-cause mortality.
Previous studies have shown that higher pulmonary arterial pressure is associated with a worse prognosis in patients undergoing M-TEER when compared to those without significant pulmonary hypertension. Tigges et al. [9] evaluated the efficacy of MitraClip® therapy in patients without, with mild and severe pulmonary hypertension, respectively, based on echocardiographically determined systolic pulmonary arterial pressure levels. Similar to our current findings, they showed that interventional success and reduction of MR were achieved in all groups. Our study demonstrated comparable findings based on invasively measured pulmonary arterial pressure. Neither mPAP nor PAWP at baseline were associated with procedural success or with the reduction of MR immediately after M-TEER or at 6 months of follow-up, suggesting M-TEER to be an effective option even for patients with severe PH.
It is well known, that PH is associated to HFH and ACM. In our current study, PH was associated to HFH but not to ACM, which seems to be contradictory. However, we believe, that there are good reasons that may explain our findings. First and foremost, a longer than 360-days follow-up period may have yielded to differences in ACM. This hypothesis is in our opinion supported by other studies in this field. Matsumoto et al. albeit offering a smaller sample size than the current investigation, showed a significant difference in ACM stratified according to PH. However, the Kaplan–Meier estimates in this study showed no difference after 360 days of follow-up but a significant difference after 720 days of follow-up [8]. In a sub-study of the COAPT trial, follow-up for ACM was 24 months. Differences in ACM stratified according to PAPsys were most pronounced after 24 months of follow-up even tough trends were evident after 12 months of follow-up. Interestingly, hospitalization for heart failure within 1-year prior to study inclusion did not differ between patients with PAPsys > 50 mmHg vs PAPsys < 50 mmHg at study inclusion [10]. Tehrani et al. could show an association of an immediate increase of mPAP after M-TEER with HFH but not ACM in a 12 months follow-up. Again, the sample size was small [22]. On the other hand, Tigges et al. found an effect of PAPsys on ACM but not rehospitalization [9]. In a large retrospective analysis by Al-Bawardy and colleagues, associations of elevated pulmonary arterial pressure with both HFH and ACM were clearly demonstrated. There are differences and similarities in these patients when compared to our cohort. In the study by Al-Bawardy, patients tended to be of older age and suffered more frequently from primary MR, respectively. Interestingly, in our cohort, significantly more patients with higher mPAP had undergone cardiac resynchronization therapy (CRT) prior to study inclusion when compared to those with lower mPAP, which may have influenced outcomes. To the best of our knowledge, information on CRT is not available in the study by Al-Bawardy et al.. Of note, over 4000 patients were included into this analysis increasing the statistical power significantly [7].
Several studies show that PH in left heart disease is associated to ACM with patients hospitalized due to HF having mortality rates significantly higher than patients never hospitalized [23, 24]. However, a considerable amount of these studies is dated with newer therapeutic strategies addressing heart failure (e.g. CRT, state of the art medication) not yet available and/or offer follow-up exceeding 12 months by far [25,26,27]. Cappola et al. e.g. state that “among patients with myocarditis, mPA is particularly good at predicting death at 1 year, whereas its prognostic value is much less among other cardiomyopathies” [26]. If we compare the current study to landmark trials in heart failure like the DAPA-HF Trial [28], we see that effects on HFH especially at 360 days of follow-up are much more pronounced than effects on ACM. Also, here, follow-up was 24 months. In a large international cohort of patients hospitalized for HF, prior HF hospitalization was associated with increased mortality in unadjusted and partially adjusted analyses but was not independently associated with 180-day mortality after adjustment for patient characteristics. In this study, 180-days ACM was 11.9% in patients without prior HFH vs. 15.5% in those with prior HFH, respectively [29]. Hence, we suggest that the combination of a limited follow-up period, a moderate sample size, and state of the art therapy are key factors, why PH and HFH are not associated to ACM in the current collective.
We could show that PAWP at baseline remained independently associated with the composite outcome and recurrent HFH after adjustment for covariates. In our analysis, PAWP at baseline was the strongest predictor of HFH, which we consider novel and a strength of our current investigation.
Most previous studies defined pulmonary hypertension based on systolic PAP assessed in transthoracic echocardiography giving an incomplete evaluation of the hemodynamic situation. Our retrospective study tried to overcome these limitations by only including patients with right heart catheterization prior to M-TEER. Thus, we provide more subtle information on pulmonary hypertension than can be given by echocardiographic measurements which may be biased by image quality or presence and severity of tricuspid regurgitation. Furthermore, we can evaluate the effect of postcapillary pulmonary hypertension on prognosis, which is hardly possible in echocardiographic measurements.
In conclusion, pulmonary arterial wedge pressure at baseline might serve as a valuable parameter for identifying patients at high risk for HFH even after successful M-TEER. Hence, patients with high pulmonary arterial wedge pressure before M-TEER might benefit from intensified monitoring and a more stringent medical therapy after intervention to avoid recurrent hospitalization.
Limitations
The current study has several limitations. First, this is a retrospective study. Hence, the design is susceptible for bias and misinterpretation. Second, the number of included patients is moderate and the study was conducted at a single center. Third, the study collective was rather heterogenous consisting of patients with ischemic and non-ischemic cardiomyopathy as well as primary and secondary MR or a combination of both. This, however, also reflects a “real-world” setting. Fourth, our study does not include a prospective validation cohort. Fifth, a considerable number of patients was lost to follow-up. Finally, a major limitation of the current study is incomplete data on PVR. However, results did not change substantially if only patients with PVR available were analyzed.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM et al (2018) Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med 379(24):2307–2318. https://doi.org/10.1056/NEJMoa1806640
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F et al (2021) 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143(5):e72–e227. https://doi.org/10.1161/CIR.0000000000000923
Geisler T, Jorbenadze R, Popov AF, Mueller KL, Rath D, Droppa M et al (2019) Thrombogenicity and Antithrombotic Strategies in Structural Heart Interventions and Nonaortic Cardiac Device Therapy-Current Evidence and Practice. Thromb Haemost 119(10):1590–1605. https://doi.org/10.1055/s-0039-1694751
Kar S, Feldman T, Qasim A, Trento A, Kapadia S, Pedersen W et al (2019) Five-year outcomes of transcatheter reduction of significant mitral regurgitation in high-surgical-risk patients. Heart 105(21):1622–1628. https://doi.org/10.1136/heartjnl-2017-312605
Lombard FW, Liang Y (2019) Risk Factors for Mitral Valve Surgery: Atrial Fibrillation and Pulmonary Hypertension. Semin Cardiothorac Vasc Anesth 23(1):57–69. https://doi.org/10.1177/1089253218821694
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M et al (2022) 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 43(38):3618–3731. https://doi.org/10.1093/eurheartj/ehac237
Al-Bawardy R, Vemulapalli S, Thourani VH, Mack M, Dai D, Stebbins A et al (2020) Association of Pulmonary Hypertension With Clinical Outcomes of Transcatheter Mitral Valve Repair. JAMA Cardiol 5(1):47–56. https://doi.org/10.1001/jamacardio.2019.4428
Matsumoto T, Nakamura M, Yeow WL, Hussaini A, Ram V, Makar M et al (2014) Impact of pulmonary hypertension on outcomes in patients with functional mitral regurgitation undergoing percutaneous edge-to-edge repair. Am J Cardiol 114(11):1735–1739. https://doi.org/10.1016/j.amjcard.2014.08.044
Tigges E, Blankenberg S, von Bardeleben RS, Zurn C, Bekeredjian R, Ouarrak T et al (2018) Implication of pulmonary hypertension in patients undergoing MitraClip therapy: results from the German transcatheter mitral valve interventions (TRAMI) registry. Eur J Heart Fail 20(3):585–594. https://doi.org/10.1002/ejhf.864
Ben-Yehuda O, Shahim B, Chen S, Liu M, Redfors B, Hahn RT et al (2020) Pulmonary Hypertension in Transcatheter Mitral Valve Repair for Secondary Mitral Regurgitation: The COAPT Trial. J Am Coll Cardiol 76(22):2595–2606. https://doi.org/10.1016/j.jacc.2020.09.609
Zuern CS, Krumm P, Wurster T, Kramer U, Schreieck J, Henning A et al (2013) Reverse left ventricular remodeling after percutaneous mitral valve repair: strain analysis by speckle tracking echocardiography and cardiac magnetic resonance imaging. Int J Cardiol 168(5):4983–4985. https://doi.org/10.1016/j.ijcard.2013.07.132
Patzelt J, Zhang W, Sauter R, Mezger M, Nording H, Ulrich M et al (2019) Elevated Mitral Valve Pressure Gradient Is Predictive of Long-Term Outcome After Percutaneous Edge-to-Edge Mitral Valve Repair in Patients With Degenerative Mitral Regurgitation ( MR ), But Not in Functional MR. J Am Heart Assoc 8(13):e011366. https://doi.org/10.1161/JAHA.118.011366
Zuern CS, Floss N, Mueller II, Eick C, Duckheim M, Patzelt J et al (2018) Galectin-3 is associated with left ventricular reverse remodeling and outcome after percutaneous mitral valve repair. Int J Cardiol 263:104–110. https://doi.org/10.1016/j.ijcard.2018.04.025
Grayburn PA, Thomas JD (2021) Basic Principles of the Echocardiographic Evaluation of Mitral Regurgitation. JACC Cardiovasc Imaging 14(4):843–853. https://doi.org/10.1016/j.jcmg.2020.06.049
Mandurino-Mirizzi A, Crimi G, Raineri C, Magrini G, Gazzoli F, Frassica R et al (2021) Haemodynamic impact of MitraClip in patients with functional mitral regurgitation and pulmonary hypertension. Eur J Clin Invest 51(12):e13676. https://doi.org/10.1111/eci.13676
Mizera L, Rath D, Schreieck J, Seizer P, Gawaz MP, Duckheim M et al (2023) Deceleration capacity of heart rate predicts 1-year mortality in patients undergoing transcatheter edge-to-edge mitral valve repair. Clin Cardiol 46(5):529–534. https://doi.org/10.1002/clc.24007
Hoeper MM, Bogaard HJ, Condliffe R, Frantz R, Khanna D, Kurzyna M et al (2013) Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 62(25 Suppl):D42-50. https://doi.org/10.1016/j.jacc.2013.10.032
Patzelt J, Ulrich M, Becker A, Muller KAL, Jorbenadze R, Droppa M et al (2018) Previous TAVR in patients undergoing percutaneous edge-to-edge mitral valve repair (PMVR) affects improvement of MR. PLoS ONE 13(10):e0205930. https://doi.org/10.1371/journal.pone.0205930
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A et al (2016) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37(1):67–119. https://doi.org/10.1093/eurheartj/ehv317
Galie N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA et al (2009) Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J 30(20):2493–2537. https://doi.org/10.1093/eurheartj/ehp297
Bo H, Heinzmann D, Grasshoff C, Rosenberger P, Schlensak C, Gawaz M et al (2019) ECG changes after percutaneous edge-to-edge mitral valve repair. Clin Cardiol 42(11):1094–1099. https://doi.org/10.1002/clc.23258
Tehrani DM, Wang J, Lai P, Desai PS, Nguyen HL, Bang L et al (2021) Change in Invasively Measured Mean Pulmonary Artery Pressure After Transcatheter Mitral Valve Repair Is Associated With Heart Failure Readmission. Cardiol Res 12(5):302–308. https://doi.org/10.14740/cr1284
Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB et al (2007) Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 116(13):1482–1487. https://doi.org/10.1161/CIRCULATIONAHA.107.696906
Setoguchi S, Stevenson LW, Schneeweiss S (2007) Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J 154(2):260–266. https://doi.org/10.1016/j.ahj.2007.01.041
Abramson SV, Burke JF, Kelly JJ Jr, Kitchen JG 3rd, Dougherty MJ, Yih DF et al (1992) Pulmonary hypertension predicts mortality and morbidity in patients with dilated cardiomyopathy. Ann Intern Med 116(11):888–895. https://doi.org/10.7326/0003-4819-116-11-888
Cappola TP, Felker GM, Kao WH, Hare JM, Baughman KL, Kasper EK (2002) Pulmonary hypertension and risk of death in cardiomyopathy: patients with myocarditis are at higher risk. Circulation 105(14):1663–1668. https://doi.org/10.1161/01.cir.0000013771.30198.82
Damy T, Goode KM, Kallvikbacka-Bennett A, Lewinter C, Hobkirk J, Nikitin NP et al (2010) Determinants and prognostic value of pulmonary arterial pressure in patients with chronic heart failure. Eur Heart J 31(18):2280–2290. https://doi.org/10.1093/eurheartj/ehq245
McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA et al (2019) Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med 381(21):1995–2008. https://doi.org/10.1056/NEJMoa1911303
Blumer V, Mentz RJ, Sun JL, Butler J, Metra M, Voors AA et al (2021) Prognostic Role of Prior Heart Failure Hospitalization Among Patients Hospitalized for Worsening Chronic Heart Failure. Circ Heart Fail 14(4):e007871. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007871
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
PJ, DR, TG, MG and JS contributed to the study design. PJ, FS, ME, IT, JH, SS, PS, HL and AM contributed to data collection. PJ and DR analyzed and interpreted the data. PJ and DR wrote the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Additional information
Jürgen Schreieck and Dominik Rath these authors share last authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jaeger, P., Toskas, I., Henes, JK. et al. Impact of pulmonary hypertension on outcomes after TEER in patients suffering from mitral regurgitation. Clin Res Cardiol (2024). https://doi.org/10.1007/s00392-024-02442-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-024-02442-1