Abstract
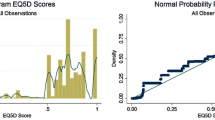
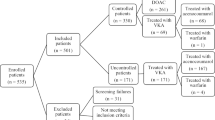
Associations of anticoagulation with primary endpoints in longitudinal studies are impacted by selection bias and time-varying covariates (e.g. comorbidities). We demonstrate how time-varying covariates and selection bias influence association estimates between anticoagulation and health-related quality of life (HRQoL) in patients with atrial fibrillation. We performed a secondary analysis of the Atrial Fibrillation Follow-up Investigation of Rhythm Management trial quality of life substudy. Dichotomized warfarin use was ascertained at the study baseline, 2 months later, and annually for up to 6 years. HRQoL was measured at every time point using a self-reported ordinal 5-point Likert-scale (lower score and lower odds ratio represents better health-related quality of life). Static and time-varying covariates were ascertained throughout the study period. Confounder-adjusted generalized mixed model and generalized estimating equation regressions were used to demonstrate traditional association estimates between anticoagulation and HRQoL. Inverse probability of treatment and censorship weights were used to ascertain the influence of time-varying confounding and selection bias. Age-stratified analysis (age ≥ 70 years) evaluated for effect modification. 656 individuals were included in the analysis, 601 on warfarin at baseline. The association of warfarin use with better HRQoL over time strengthened when accounting for time-varying confounding and selection bias (OR 0.30, 95% CI 0.14–0.55) compared to traditional analyses (OR 0.61, 95% CI 0.38–0.97), and was most pronounced in those ≥ 70 years upon stratified analysis. Anticoagulation is associated with higher HRQoL in patients with atrial fibrillation, with time-varying confounding and selection bias likely influencing longitudinal estimates in anticoagulation-HRQoL research.
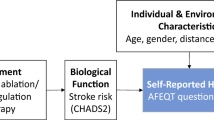
Graphical abstract



Similar content being viewed by others
Data availability
Data from the AFFIRM Quality of Life Substudy was obtained from the Biologic Specimen and Data Repository Information Coordinating Center (BioLincc) of the National Heart, Lung and Blood Institute (NHLBI) of the National Institutes of Health (NIH).
References
Katzan IL, Thompson NR, Uchino K, Lapin B (2018) The most affected health domains after ischemic stroke. Neurology 90:e1364–e1371
Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R et al (2005) Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke 36:1115–1119
Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K et al (2007) Heart disease and stroke statistics—2007 update: a report from the american heart association statistics committee and stroke statistics subcommittee. Circulation 115:e69-171
Tu HT, Campbell BC, Christensen S, Desmond PM, De Silva DA, Parsons MW et al (2015) Worse stroke outcome in atrial fibrillation is explained by more severe hypoperfusion, infarct growth, and hemorrhagic transformation. Int J Stroke 10:534–540
Freedman B, Potpara TS, Lip GY (2016) Stroke prevention in atrial fibrillation. Lancet 388:806–817
Wolf PA, Abbott RD, Kannel WB (1987) Atrial fibrillation: a major contributor to stroke in the elderly. The framingham study. Arch Intern Med 147:1561–1564
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137:263–272
Mefford MT, Zhou H, Fan D, Fang MC, Prasad PA, Go AS et al (2022) Health literacy and treatment satisfaction among patients with venous thromboembolism. J Gen Intern Med 38:1582–1592
Pappas MA, Barnes GD, Vijan S (2019) Cost-effectiveness of bridging anticoagulation among patients with nonvalvular atrial fibrillation. J Gen Intern Med 34:583–590
Shah SJ, Singer DE, Fang MC, Reynolds K, Go AS, Eckman MH (2019) Net clinical benefit of oral anticoagulation among older adults with atrial fibrillation. Circ Cardiovasc Qual Outcomes 12:e006212
Whitbeck MG, Charnigo RJ, Khairy P, Ziada K, Bailey AL, Zegarra MM et al (2013) Increased mortality among patients taking digoxin—analysis from the affirm study. Eur Heart J 34:1481–1488
Gheorghiade M, Fonarow GC, van Veldhuisen DJ, Cleland JG, Butler J, Epstein AE et al (2013) Lack of evidence of increased mortality among patients with atrial fibrillation taking digoxin: findings from post hoc propensity-matched analysis of the affirm trial. Eur Heart J 34:1489–1497
Murphy SA (2013) When “digoxin use” is not the same as “digoxin use”: lessons from the affirm trial. Eur Heart J 34:1465–1467
Abdel-Qadir H, Fang J, Lee DS, Tu JV, Amir E, Austin PC et al (2018) Importance of considering competing risks in time-to-event analyses: Application to stroke risk in a retrospective cohort study of elderly patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes 11:e004580
Robins JM, Hernan MA, Brumback B (2000) Marginal structural models and causal inference in epidemiology. Epidemiology 11:550–560
Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB et al (2002) A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 347:1825–1833
Jenkins LS, Brodsky M, Schron E, Chung M, Rocco T Jr, Lader E et al (2005) Quality of life in atrial fibrillation: the atrial fibrillation follow-up investigation of rhythm management (affirm) study. Am Heart J 149:112–120
Reeves SL, Brown DL, Baek J, Wing JJ, Morgenstern LB, Lisabeth LD (2015) Ethnic differences in poststroke quality of life in the brain attack surveillance in corpus christi (basic) project. Stroke 46:2896–2901
Reynolds MR, Ellis E, Zimetbaum P (2008) Quality of life in atrial fibrillation: measurement tools and impact of interventions. J Cardiovasc Electrophysiol 19:762–768
Campeau L (2002) The canadian cardiovascular society grading of angina pectoris revisited 30 years later. Can J Cardiol 18:371–379
Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS et al (2001) Acc/aha guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the american college of cardiology/american heart association task force on practice guidelines (committee to revise the 1995 guidelines for the evaluation and management of heart failure). J Am Coll Cardiol 38:2101–2113
VanderWeele TJ (2010) Bias formulas for sensitivity analysis for direct and indirect effects. Epidemiology 21:540–551
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (iptw) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34:3661–3679
StataCorp. Stata statistical software: Release 17. 2021
Conner SC, Lodi S, Lunetta KL, Casas JP, Lubitz SA, Ellinor PT et al (2019) Refining the association between body mass index and atrial fibrillation: G-formula and restricted mean survival times. J Am Heart Assoc 8:e013011
Weuve J, Tchetgen Tchetgen EJ, Glymour MM, Beck TL, Aggarwal NT, Wilson RS et al (2012) Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiology 23:119–128
Huber M, Vogelmann M, Leidl R (2018) Valuing health-related quality of life: systematic variation in health perception. Health Qual Life Outcomes 16:156
Ayis S, Wellwood I, Rudd AG, McKevitt C, Parkin D, Wolfe CD (2015) Variations in health-related quality of life (hrqol) and survival 1 year after stroke: five european population-based registers. BMJ Open 5:e007101
Pezawas T, Ristl R, Schukro C, Schmidinger H (2016) Health-related quality of life changes in patients undergoing repeated catheter ablation for atrial fibrillation. Clin Res Cardiol 105:1–9
Meissner A, Christ M, Maagh P, Borchard R, van Bracht M, Wickenbrock I et al (2007) Quality of life and occurrence of atrial fibrillation in long-term follow-up of common type atrial flutter ablation: ablation with irrigated 5 mm tip and conventional 8 mm tip electrodes. Clin Res Cardiol 96:794–802
Jurek AM, Greenland S, Maldonado G, Church TR (2005) Proper interpretation of non-differential misclassification effects: expectations vs observations. Int J Epidemiol 34:680–687
Acknowledgements
No additional acknowledgements.
Funding
The research reported in this publication was supported (in part or in full) by the Utah Stimulating Access to Research in Residency Transition Scholar (StARRTS) under Award Number 1R38HL143605-01. (Eric L Stulberg and Alex R Zheutlin). Adam de Havenon reports NIH/NINDS funding (K23NS105924). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Eric L. Stulberg, Alen L. Delic, Alexander R. Zheutlin, Benjamin A. Steinberg, Shadi Yaghi, and Richa Sharma report no disclosures or conficts of interest. Adam de Havenon has received funding from Integra, Novo Nordisk, UpToDate and has equity in TitinKM and Certus.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stulberg, E.L., Delic, A., Zheutlin, A.R. et al. Modelling anticoagulation and health-related quality of life in those with atrial fibrillation: a secondary analysis of AFFIRM. Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02335-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00392-023-02335-9