Abstract
Aims
Recent randomized trials have documented the superiority of TAVR—particularly via transfemoral access—over SAVR in patients with severe aortic stenosis considered to have a high or intermediate operative risk of death. We sought to assess in-hospital outcomes of patients with severe aortic stenosis and a low risk of operative mortality undergoing routine surgical aortic valve replacement (SAVR) or transcatheter aortic valve replacement (TAVR).
Methods and results
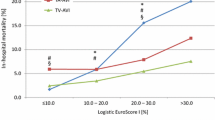
We performed a propensity-score matched comparison of all patients undergoing first-time treatment by SAVR or transfemoral TAVR (TF-TAVR) in 2014 in Germany who had a logistic EuroSCORE (logES) ≤ 10%, considered to reflect low surgical risk. The primary endpoint of our analysis was in-hospital mortality. Of 7624 SAVR and 9969 TF-TAVR procedures, 6844 (89.8%) and 2751 patients (27.6%), respectively, were considered low risk with a logES between 1.505 and 10.0%. Matching yielded 805 TF-TAVR/SAVR patient pairs with identical propensity scores and no difference in pertinent baseline characteristics, except for the logES, which was significantly higher in TF-TAVR patients (6.8 ± 1.7 vs. 4.2 ± 1.3% in SAVR patients, P < 0.001). Observed in-hospital mortalities were 1.7% (95% confidence interval, 1.1–3.0%) in SAVR and 2.0% (1.3–3.3%) in TF-TAVR patients (P = 0.85).
Conclusion
Our finding of no difference in in-hospital mortality in propensity-score matched low-surgical-risk patients treated by SAVR or TF-TAVR in a routine clinical setting indicates that TF-TAVR can be offered safely to individual patients, despite their operative risk being low. This finding needs to be confirmed in a randomized trial.


Similar content being viewed by others
Abbreviations
- AS:
-
Aortic stenosis
- AVR:
-
Aortic valve replacement
- EuroSCORE:
-
European system for cardiac operative risk evaluation
- logES:
-
Logistic EuroSCORE
- PARTNER:
-
Placement of aortic transcatheter valve
- SAVR:
-
Surgical aortic valve replacement
- TAVR:
-
Transcatheter aortic valve replacement
- TA-TAVR:
-
Transapical TAVR
- TF-TAVR:
-
Transfemoral TAVR
- THV:
-
Transcatheter heart valve
References
Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, Alfieri O, Andreotti F et al (2012) Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 33:2451–2496
Leon MB, Smith CR, Mack M et al PARTNER Trial Investigators (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Smith CR, Leon MB, Mack MJ et al; PARTNER Trial Investigators (2011) Transcatheter vs. surgical aortic-valve replacement in high-risk patients. N Engl J Med 364:2187–2198
Mack MJ, Leon MB, Smith CR et al; PARTNER 1 trial investigators (2015) 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385:2477–2484
Adams DH, Popma JJ, Reardon MJ et al (2014) U.S. CoreValve Clinical Investigators. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 370:1790–1798
Reardon MJ, Adams DH, Kleiman NS et al (2015) 2-Year outcomes in patients undergoing surgical or self-expanding transcatheter aortic valve replacement. J Am Coll Cardiol 66:113–121
Leon MB, Smith CR, Mack MJ et al; PARTNER 2 Investigators (2016) Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 374:1609–1620
Thourani VH, Kodali S, Makkar RR et al (2016) Transcatheter aortic valve replacement vs. surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet 387:2218–2225
Thyregod HG, Steinbrüchel DA, Ihlemann N et al (2015) Transcatheter vs. surgical aortic valve replacement in patients with severe aortic valve stenosis: 1-year results from the all-comers NOTION randomized clinical trial. J Am Coll Cardiol 65:2184–2194
Bestehorn K, Bestehorn M, Fleck E (2015) Influence of different approaches of aortic valve replacement on the incidence of post-operative delirium in intermediate risk patients—a matched pair analysis. Curr Med Res Opin 31:2157–2163
Abdul-Jawad Altisent O, Ferreira-Gonzalez I, Marsal JR et al (2016) Neurological damage after transcatheter aortic valve implantation compared with surgical aortic valve replacement in intermediate risk patients. Clin Res Cardiol 105:508–517
Hobson CE, Yavas S, Segal MS et al (2009) Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119:2444–2453
Eggebrecht H, Mehta RH (2016) Transcatheter aortic valve implantation (TAVI) in Germany 2008–2014: on its way to standard therapy for aortic valve stenosis in the elderly? Eurointervention 11:1029–1033
Möllmann H, Bestehorn K, Bestehorn M et al (2016) In-hospital outcome of transcatheter vs. surgical aortic valve replacement in patients with aortic valve stenosis: complete dataset of patients treated in 2013 in Germany. Clin Res Cardiol 105:553–559
Rosato S, Santini F, Barbanti M et al; OBSERVANT Research Group (2016 May) Transcatheter aortic valve implantation compared with surgical aortic valve replacement in low-risk patients. Circ Cardiovasc Interv 9:e003326
Dizon JM, Nazif TM, Hess PL et al; PARTNER Publications Office (2015) Chronic pacing and adverse outcomes after transcatheter aortic valve implantation. Heart 101:1665–1671
Mouillet G, Lellouche N, Yamamoto M et al (2015) Outcomes following pacemaker implantation after transcatheter aortic valve implantation with CoreValve(®) devices: results from the FRANCE 2 Registry. Catheter Cardiovasc Interv 86:E158–E166
Biner S, Michowitz Y, Leshem-Rubinow E et al (2014) Hemodynamic impact and outcome of permanent pacemaker implantation following transcatheter aortic valve implantation. Am J Cardiol 113:132–137
Schymik G, Tzamalis P, Bramlage P et al (2015) Clinical impact of a new left bundle branch block following TAVI implantation: 1-year results of the TAVIK cohort. Clin Res Cardiol 104:351–362
Dvir D (2016) First look at long-term durability of transcatheter heart valves: assessment of valve function up to 10 years after implantation. Presented at: EuroPCR 2016. Paris, France. http://www.pcronline.com/Lectures/2016/First-look-at-long-term-durability-of-transcatheter-heart-valves-assessment-of-valve-function-up-to-10-years-after-implantation. Accessed 16 Jan 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study was partly funded by an unrestricted grant from the German Cardiac Society.
Conflicts of interest
CWH has served on the Advisory Board for Medtronic. HAK has received personal fees from Roche Diagnostics, Bayer Vital, AstraZeneca, and Daiichi Sankyo. KHK has received personal fees from Medtronic, Biosense Webster, and St. Jude Medical. The other authors declare no conflicts of interest.
Additional information
C. Frerker and K. Bestehorn contributed equally to this work.
Rights and permissions
About this article
Cite this article
Frerker, C., Bestehorn, K., Schlüter, M. et al. In-hospital mortality in propensity-score matched low-risk patients undergoing routine isolated surgical or transfemoral transcatheter aortic valve replacement in 2014 in Germany. Clin Res Cardiol 106, 610–617 (2017). https://doi.org/10.1007/s00392-017-1097-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1097-y