Abstract
Background
The multidimensional prognostic index (MPI) is a validated, sensitive, and specific prognosis estimation tool based on a comprehensive geriatric assessment (CGA). The MPI accurately predicts mortality after 1 month and 1 year in older, multimorbid patients with acute disease or relapse of chronic conditions.
Objective
To evaluate whether the MPI predicts indicators of healthcare resources, i.e. grade of care (GC), length of hospital stay (LHS) and destination after hospital discharge in older patients in an acute medical setting.
Material and methods
In this study 135 hospitalized patients aged 70 years and older underwent a CGA evaluation to calculate the MPI on admission and discharge. Accordingly, patients were subdivided in low (MPI‑1, score 0–0.33), moderate (MPI-2, score 0.34–0.66) and high (MPI-3, score 0.67–1) risk of mortality. The GC, LHS and the discharge allocation were also recorded.
Results
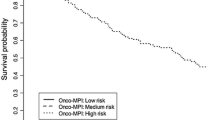
The MPI score was significantly related to LHS (p = 0.011) and to GC (p < 0.001). In addition, MPI-3 patients were significantly more often transferred from other hospital settings (p = 0.007) as well as significantly less likely to be discharged home (p = 0.04) than other groups.
Conclusion
The CGA-based MPI values are significantly associated with use of indicators of healthcare resources, including GC, LHS and discharge allocation. These findings suggest that the MPI may be useful for resource planning in the care of older multimorbid patients admitted to hospital.
Zusammenfassung
Hintergrund
Der Multidimensionale Prognostische Index (MPI) ist ein validiertes, sensitives und spezifisches Instrument zur Abschätzung der Prognose auf der Basis des Comprehensive Geriatric Assessment (CGA). Der MPI eignet sich für eine genaue Vorhersage der Einmonats- und der Einjahresmortalität für ältere, multimorbide Patienten mit einer akuten Erkrankung oder mit einem Rezidiv bzw. einer Exazerbation einer chronischen Erkrankung.
Ziel
Verifiziert werden sollte, ob sich mit Hilfe des MPI bei älteren, hospitalisierten Patienten in einem akuten Setting Indikatoren gesundheitsassoziierter Ressourcen, wie Pflegegrad („grade of care“, GC), Dauer des stationären Aufenthalts („length of hospital stay“, LHS) und das Verlegungsziel, genau vorhersagen lassen.
Material und Methoden
Einhundertfünfunddreißig hospitalisierte Patienten im Alter über 70 Jahren wurden mit dem CGA untersucht, um den MPI bei Aufnahme und bei Entlassung zu berechnen. Dabei wurden die Patienten verschiedenen Risikobereichen zugeordnet: niedriges (MPI-1, Score 0–0,33), mittleres (MPI-2, 0,34–0,66) und hohes (MPI-3, 0,67–1) Mortalitätsrisiko. Zusätzlich wurden GC, LHS und Verlegungsziel erhoben.
Ergebnisse
Der MPI-Wert war signifikant mit der LHS (p = 0,011) und dem GC (p < 0,001) assoziiert. Zusätzlich wurden MPI-3-Patienten signifikant häufiger aus anderen Krankenhäusern bei Aufnahme verlegt (p = 0,007) als die der anderen Gruppen, und es war weniger wahrscheinlich, dass die MPI-3-Patienten nach Hause entlassen wurden (p = 0,04).
Diskussion
Die CGA-basierten MPI-Werte waren signifikant mit Indikatoren gesundheitsbezogener Ressourcen assoziiert, einschließlich GC, LHS und Verlegungsziel. Diese Ergebnisse deuten darauf hin, dass der MPI bei der Ressourcenplanung in der Versorgung von älteren, multimorbiden und hospitalisierten Patienten hilfreich sein könnte.

Similar content being viewed by others
References
Angleman SB et al (2015) Multidimensional prognostic index in association with future mortality and number of hospital days in a population-based sample of older adults: results of the EU funded MPI_AGE project. PLoS ONE. https://doi.org/10.1371/journal.pone.0133789
Baake CP (ed) (2017) Begutachtungsverfahren NBA – Pflegegrad bei Erwachsenen. Walhalla, Regensburg
Barmer (2017) https://www.barmer.de/blob/135698/ac141c44b72fe5a24a6d453c6fda9bf0/data/dl-pflegereport-2017.pdf. Accessed 26 Mar 2018
Bliss MR, McLaren R, Exton-Smith AN (1966) Mattresses for preventing pressure sores in geriatric patients. Mon Bull Minist Health Public Health Lab Serv 25:238–268
BMC Pulm Med (2012). https://doi.org/10.1186/1471-2466-12-21
Bundesministerium für Gesundheit (2017) https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/Statistiken/Pflegeversicherung/Zahlen_und_Fakten/Zahlen_und_Fakten.pdf. Accessed 2 Mar 2018
Campbell SE, Seymour DG, Primrose WR, Lynch JE et al (2005) A multi-centre European study of factors affecting the discharge destination of older people admitted to hospital: analysis of in-hospital data from the ACMEplus project. Age Ageing 34(5):467–475. https://doi.org/10.1093/ageing/afi141
Challiner Y, Carpenter GI, Potter J et al (2003) Performance indicators for hospital services for older people. Age Ageing 32:343–346
Dent E, Kowal P, Hoogendijk EO (2016) Frailty measurement in research and clinical practice: A review. Eur J Intern Med 31:3–10. https://doi.org/10.1016/j.ejim.2016.03.007
Destatis (2016) https://www.destatis.de/DE/Publikationen/Datenreport/Downloads/Datenreport2016Kap2.pdf?__blob=publicationFile. Accessed 26 Mar 2018
European Union (2017) State of health in the EU: companion report 2017. http://ec.europa.eu/health/sites/health/files/state/docs/2017_companion_en.pdf. Accessed 2 Mar 2018
Forsyth NR, McWhir J (2007) Human embryonic stem cell telomere length impacts directly on clonal progenitor isolation frequency. Rejuvenation Res. https://doi.org/10.1089/rej.2007.0569
Gallucci M, Battistella G, Bergamelli C, Spagnolo P et al (2014) Multidimensional prognostic index in a cognitive impairment outpatient setting: Mortality and hospitalizations. The treviso dementia (TREDEM) study. J Alzheimers Dis 42(4):1461–1468. https://doi.org/10.3233/JAD-140516
Gill TM (2012) The central role of prognosis in clinical decision making. JAMA 307(2):199–200. https://doi.org/10.1001/jama.2011.1992
Harari D, Martin FC, Buttery A, O’Neill S, Hopper A (2007) The older persons’ assessment and liaison team ‘OPAL’: evaluation of comprehensive geriatric assessment in acute medical inpatients. Age Ageing 36(6):670–675. https://doi.org/10.1093/ageing/afm089
Hashimoto M, Matsuzaki Y, Kawahara K (2014) Medication-related factors affecting discharge to home. Biol Pharm Bull 37(7):1228–1233
Joob B, Wiwanitkit V (2012) Multidimensional prognostic index and the estimated glomerular filtration rate. Rejuvinated Research. https://doi.org/10.1089/rej.2012.1327
Katz S, Downs TD, Cash HR, Grotz RC (1970) Progress in the development of an index of ADL. Gerontologist 10:20–30
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Linn BS, Linn MW, Gurel L (1968) The Cumulative Illness Rating Scale. J Am Geriatr Soc 16:622–626
Lohaus S (2015) Land ohne Kinder. http://www.faz.net/aktuell/.../bevoelkerungsentwicklung-land-ohne-kinder-13630943.html. Accessed 2 Mar 2018
MPI_Age (2018) http://www.mpiage.eu. Accessed 2 Mar 2018
Paulus W, Schweitzer R, Wiemer S (2010) Klassifikation der Berufe 2010 – Entwicklung und Ergebnis. Methodenbericht der Statistik der BA. BA, Nürnberg
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Pilotto A, Cella A, Pilotto A, Daragjati J, Veronese N et al (2016) Three decades of comprehensive geriatric assessment: evidence coming from different healthcare settings and specific clinical conditions. J Am Med Dir Assoc 18(2):192.e1–192.e11. https://doi.org/10.1016/j.jamda.2016.11.004
Sancarlo D, D’Onofrio G, Franceschi M et al (2011) Validation of a modified-Multidimensional Prognostic Index (m-MPI) including the Mini Nutritional Assessment Short-Form (MNA-SF) for the prediction of one-year mortality in hospitalized elderly patients. J Nutr Health Aging 3:169–173
Warnier RM, van Rossum E, van Velthuijsen E, Mulder WJ, Schols JM, Kempen GI (2015) Validity, reliability and feasibility of tools to identify frail older patients in inpatient hospital care: A systematic review. J Nutr Health Aging 20(2):218–230. https://doi.org/10.1007/s12603-015-0567-z
Acknowledgements
The results were partly presented at the Annual Congress of the German Geriatrics Society 2017, where the study MPI_InGAH received the prize for the “Promotion of the interdisciplinary age medicine” of the German Geriatrics Society. The authors are grateful to the patients who took their time during the hospital stay to take part of that interview.
Author contributions
AMM and MCP conceived and designed the clinical trial. AMM performed the experiments. AMM, IB and GS analyzed the data. AMM wrote the paper. AMM, MCP and IB conceived the manuscript. AMM, MCP, IB, TB, PTB and AP performed critical revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.M. Meyer, I. Becker, G. Siri, P.T. Brinkkötter, T. Benzing, A. Pilotto and M. C. Polidori declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
A. Pilotto and M.C. Polidori contributed equally to the manuscript.
Caption Electronic Supplementary Material
Supplement 1
Calculating the multidimensional prognostic index (MPI) after Pilotto et al. [12]
Rights and permissions
About this article
Cite this article
Meyer, A.M., Becker, I., Siri, G. et al. New associations of the Multidimensional Prognostic Index. Z Gerontol Geriat 52, 460–467 (2019). https://doi.org/10.1007/s00391-018-01471-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-018-01471-6