Abstract
Purpose
This meta-analysis is aimed at understanding the potential role of circulating C-reactive protein (CRP) in the prediction of colorectal cancer (CRC) risk and the potential effect of relevant variables, with specific concern to determine the incorporation of CRP into a CRC risk prediction model.
Methods
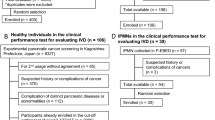
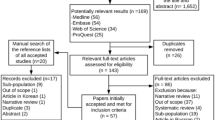
Relevant articles on the association between circulating CRP and CRC risk were searched from PubMed, Embase, Web of Science, and Cochrane Database of Systematic Reviews through August 2022. Random-effects models were used to estimate the pooled relative risk (RR) for the highest versus lowest CRP categories. Linear and non-linear trend analyses were conducted to explore the dose–response associations between CRP and CRC risk.
Results
Twenty-three articles including 780,985 participants and 11,289 cancer cases met the selection criteria. The overall result demonstrated a remarkable association between elevated CRP levels and CRC risk (RR, 1.259; 95% CI, 1.060–1.457), but not in dose–response analysis (RR, 1.002 (95% CI, 0.964–1.041) per natural log unit change in CRP). Subgroup analyses indicated a significant difference when grouped by study location, the length of follow-up, and gender composition. No evidence of publication bias was observed.
Conclusion
The predictive role of CRP in CRC incidence is limited to colon cancer and a period of 10 years after the initial discovery of CRP elevation. The result did not support the etiological role of CRP in CRC and the inclusion of CRP into the CRC risk prediction model.




Similar content being viewed by others
Data Availability
All data supporting the findings of this study are available in this published article and its supplementary information.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians 71(3):209–249. https://doi.org/10.3322/caac.21660
Schmitt M, Greten FR (2021) The inflammatory pathogenesis of colorectal cancer. Nat Rev Immunol 21(10):653–667. https://doi.org/10.1038/s41577-021-00534-x
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454(7203):436–444. https://doi.org/10.1038/nature07205
Greten FR, Grivennikov SI (2019) Inflammation and cancer: triggers, mechanisms, and consequences. Immunity 51(1):27–41. https://doi.org/10.1016/j.immuni.2019.06.025
Tuomisto AE, Makinen MJ, Vayrynen JP (2019) Systemic inflammation in colorectal cancer: underlying factors, effects, and prognostic significance. World J Gastroenterol 25(31):4383–4404. https://doi.org/10.3748/wjg.v25.i31.4383
Hou J, Karin M, Sun B (2021) Targeting cancer-promoting inflammation - have anti-inflammatory therapies come of age? Nat Rev Clin Oncol 18(5):261–279. https://doi.org/10.1038/s41571-020-00459-9
Pan L, Zhou Y, Yin H, Hui H, Guo Y, Xie X (2022) Omega-3 polyunsaturated fatty acids can reduce c-reactive protein in patients with cancer: a systematic review and meta-analysis of randomized controlled trials. Nutr Cancer 74(3):840–851. https://doi.org/10.1080/01635581.2021.1931365
Guo Y, Ma B, Li X, Hui H, Zhou Y, Li N et al (2022) n -3 PUFA can reduce IL-6 and TNF levels in patients with cancer. Brit J Nutr:1–12. https://doi.org/10.1017/S0007114522000575
Allin KH, Bojesen SE, Nordestgaard BG (2016) Inflammatory biomarkers and risk of cancer in 84,000 individuals from the general population. Int J Cancer 139(7):1493–1500. https://doi.org/10.1002/ijc.30194
Toriola AT, Cheng TD, Neuhouser ML, Wener MH, Zheng Y, Brown E et al (2013) Biomarkers of inflammation are associated with colorectal cancer risk in women but are not suitable as early detection markers. Int J Cancer 132(11):2648–2658. https://doi.org/10.1002/ijc.27942
Song M, Wu K, Ogino S, Fuchs CS, Giovannucci EL, Chan AT (2013) A prospective study of plasma inflammatory markers and risk of colorectal cancer in men. Brit J Cancer 108(9):1891–1898. https://doi.org/10.1038/bjc.2013.172
Lee YJ, Lee HR, Nam CM, Hwang UK, Jee SH (2006) White blood cell count and the risk of colon cancer. Yonsei Med J 47(5):646–656. https://doi.org/10.3349/ymj.2006.47.5.646
Aleksandrova K, Jenab M, Bueno-De-Mesquita HB, Fedirko V, Kaaks R, Lukanova A et al (2014) Biomarker patterns of inflammatory and metabolic pathways are associated with risk of colorectal cancer: results from the European Prospective Investigation into Cancer and Nutrition (EPIC). Eur J Epidemiol 29(4):261–275. https://doi.org/10.1007/s10654-014-9901-8
Chan AT, Ogino S, Giovannucci EL, Fuchs CS (2011) Inflammatory markers are associated with risk of colorectal cancer and chemopreventive response to anti-inflammatory drugs. Gastroenterology 140(3):799–808. https://doi.org/10.1053/j.gastro.2010.11.041
Nost TH, Alcala K, Urbarova I, Byrne KS, Guida F, Sandanger TM et al (2021) Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol 36(8):841–848. https://doi.org/10.1007/s10654-021-00752-6
Wesselink E, Balvers M, Kok DE, Winkels RM, van Zutphen M, Schrauwen R et al (2021) Levels of inflammation markers are associated with the risk of recurrence and all-cause mortality in patients with colorectal cancer. Cancer Epidemiol Biomarkers Prev 30(6):1089–1099. https://doi.org/10.1158/1055-9965.EPI-20-1752
Allin KH, Nordestgaard BG (2011) Elevated C-reactive protein in the diagnosis, prognosis, and cause of cancer. Crit Rev Clin Lab Sci 48(4):155–170. https://doi.org/10.3109/10408363.2011.599831
Erlinger TP (2004) C-reactive protein and the risk of incident colorectal cancer. JAMA 291(5):585. https://doi.org/10.1001/jama.291.5.585
Zhou B, Shu B, Yang J, Liu J, Xi T, Xing Y (2014) C-reactive protein, interleukin-6 and the risk of colorectal cancer: a meta-analysis. Cancer Causes Control 25(10):1397–1405. https://doi.org/10.1007/s10552-014-0445-8
Tsilidis KK, Branchini C, Guallar E, Helzlsouer KJ, Erlinger TP, Platz EA (2008) C-reactive protein and colorectal cancer risk: a systematic review of prospective studies. Int J Cancer 123(5):1133–1140. https://doi.org/10.1002/ijc.23606
Heikkila K, Harris R, Lowe G, Rumley A, Yarnell J, Gallacher J et al (2009) Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes Control 20(1):15–26. https://doi.org/10.1007/s10552-008-9212-z
Guo YZ, Pan L, Du CJ, Ren DQ, Xie XM (2013) Association between C-reactive protein and risk of cancer: a meta-analysis of prospective cohort studies. Asian Pac J Cancer Prev 14(1):243–248. https://doi.org/10.7314/apjcp.2013.14.1.243
Wang G, Xu WG, Li F, Su K, Li N, Lu ZY et al (2017) [Relationship between inflammatory markers and the risk of colorectal cancer in Kailuan male cohort]. Zhonghua Yi Xue Za Zhi 97(40):3158–3161. https://doi.org/10.3760/cma.j.issn.0376-2491.2017.40.008
Ghuman S, Van Hemelrijck M, Garmo H, Holmberg L, Malmström H, Lambe M et al (2017) Serum inflammatory markers and colorectal cancer risk and survival. Brit J Cancer 116(10):1358–1365. https://doi.org/10.1038/bjc.2017.96
Prizment AE, Linabery AM, Lutsey PL, Selvin E, Nelson HH, Folsom AR et al (2016) Circulating beta-2 microglobulin and risk of cancer: the atherosclerosis risk in communities study (ARIC). Cancer Epidem Biomar 25(4):657–664. https://doi.org/10.1158/1055-9965.EPI-15-0849
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA: J Am Med Assoc 283(15):2008–2012. https://doi.org/10.1001/jama.283.15.2008
Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-response data. Stata J 6(1):40–57. https://doi.org/10.1177/1536867X0600600103
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135(11):1301–1309. https://doi.org/10.1093/oxfordjournals.aje.a116237
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175(1):66–73. https://doi.org/10.1093/aje/kwr265
Borges ÁH, Silverberg MJ, Wentworth D, Grulich AE, Fätkenheuer G, Mitsuyasu R et al (2013) Predicting risk of cancer during HIV infection. Aids 27(9):1433–1441. https://doi.org/10.1097/qad.0b013e32835f6b0c
Il'Yasova D (2005) Circulating levels of inflammatory markers and cancer risk in the health aging and body composition cohort. Cancer Epidem Biomar 14(10):2413–2418. https://doi.org/10.1158/1055-9965.EPI-05-0316
van T Klooster CC, Ridker PM, Hjortnaes J, van der Graaf Y, Asselbergs FW, Westerink J et al (2019) The relation between systemic inflammation and incident cancer in patients with stable cardiovascular disease: a cohort study. Eur Heart J 40(48):3901–3909. https://doi.org/10.1093/eurheartj/ehz587
Zuo H, Tell GS, Vollset SE, Ueland PM, Nygård O, Midttun Ø et al (2014) Interferon-γ–induced inflammatory markers and the risk of cancer: the Hordaland Health Study. Cancer-Am Cancer Soc 120(21):3370–3377. https://doi.org/10.1002/cncr.28869
Hopkins MH, Flanders WD, Bostick RM (2012) Associations of circulating inflammatory biomarkers with risk factors for colorectal cancer in colorectal adenoma patients. Biomark Insights 7:143–150. https://doi.org/10.4137/BMI.S10092
Aleksandrova K, di Giuseppe R, Isermann B, Biemann R, Schulze M, Wittenbecher C et al (2016) Circulating omentin as a novel biomarker for colorectal cancer risk: data from the epic-potsdam cohort study. Cancer Res 76(13):3862–3871. https://doi.org/10.1158/0008-5472.CAN-15-3464
Boden S, Myte R, Harbs J, Sundkvist A, Zingmark C, Lofgren BA et al (2020) C-reactive protein and future risk of clinical and molecular subtypes of colorectal cancer. Cancer Epidemiol Biomarkers Prev 29(7):1482–1491. https://doi.org/10.1158/1055-9965.EPI-19-1339
Proctor MJ, Talwar D, Balmar SM, O'Reilly DS, Foulis AK, Horgan PG et al (2010) The relationship between the presence and site of cancer, an inflammation-based prognostic score and biochemical parameters. initial results of the glasgow inflammation outcome study. Br J Cancer 103(6):870–876. https://doi.org/10.1038/sj.bjc.6605855
Tsilidis KK, Erlinger TP, Rifai N, Hoffman S, Hoffman-Bolton J, Helzlsouer KJ et al (2008) C-reactive protein and colorectal adenoma in the CLUE II cohort. Cancer Causes Control 19(6):559–567. https://doi.org/10.1007/s10552-008-9117-x
Gunter MJ, Cross AJ, Huang WY, Stanczyk FZ, Purdue M, Xue X et al (2011) A prospective evaluation of C-reactive protein levels and colorectal adenoma development. Cancer Epidemiol Biomarkers Prev 20(3):537–544. https://doi.org/10.1158/1055-9965.EPI-10-1099
Chiu HM, Lin JT, Chen TH, Lee YC, Chiu YH, Liang JT et al (2008) Elevation of C-reactive protein level is associated with synchronous and advanced colorectal neoplasm in men. Am J Gastroenterol 103(9):2317–2325. https://doi.org/10.1111/j.1572-0241.2008.01952.x
Nimptsch K, Aleksandrova K, Boeing H, Janke J, Lee YA, Jenab M et al (2015) Association of CRP genetic variants with blood concentrations of CRP and colorectal cancer risk. Int J Cancer 136(5):1181–1192. https://doi.org/10.1002/ijc.29086
Allin KH, Nordestgaard BG, Zacho J, Tybjaerg-Hansen A, Bojesen SE (2010) C-reactive protein and the risk of cancer: a Mendelian randomization study. J Natl Cancer Inst 102(3):202–206. https://doi.org/10.1093/jnci/djp459
Slattery ML, Curtin K, Poole EM, Duggan DJ, Samowitz WS, Peters U et al (2011) Genetic variation in C-reactive protein in relation to colon and rectal cancer risk and survival. Int J Cancer 128(11):2726–2734. https://doi.org/10.1002/ijc.25721
Jung SY, Yu H, Pellegrini M, Papp JC, Sobel EM, Zhang ZF (2021) Genetically determined elevated C-reactive protein associated with primary colorectal cancer risk: Mendelian randomization with lifestyle interactions. Am J Cancer Res 11(4):1733–1753
Izano M, Wei EK, Tai C, Swede H, Gregorich S, Harris TB et al (2016) Chronic inflammation and risk of colorectal and other obesity-related cancers: the health, aging and body composition study. Int J Cancer 138(5):1118–1128. https://doi.org/10.1002/ijc.29868
Wang G, Li N, Chang S, Bassig BA, Guo L, Ren J et al (2015) A prospective follow-up study of the relationship between c-reactive protein and human cancer risk in the Chinese Kailuan female cohort. Cancer Epidem Biomar 24(2):459–465. https://doi.org/10.1158/1055-9965.EPI-14-1112
Ananthakrishnan AN, Cheng SC, Cai T, Cagan A, Gainer VS, Szolovits P et al (2014) Serum inflammatory markers and risk of colorectal cancer in patients with inflammatory bowel diseases. Clin Gastroenterol H 12(8):1342–1348. https://doi.org/10.1016/j.cgh.2013.12.030
Wu J, Cai Q, Li H, Cai H, Gao J, Yang G et al (2013) Circulating c-reactive protein and colorectal cancer risk: a report from the Shanghai Men’s Health Study. Carcinogenesis 34(12):2799–2803. https://doi.org/10.1093/carcin/bgt288
Prizment AE, Folsom AR, Dreyfus J, Anderson KE, Visvanathan K, Joshu CE et al (2013) Plasma C-reactive protein, genetic risk score, and risk of common cancers in the atherosclerosis risk in communities study. Cancer Cause Control 24(12):2077–2087. https://doi.org/10.1007/s10552-013-0285-y
Van Hemelrijck M, Holmberg L, Garmo H, Hammar N, Walldius G, Binda E et al (2011) Association between levels of c-reactive protein and leukocytes and cancer: three repeated measurements in the Swedish AMORIS study. Cancer Epidem Biomar 20(3):428–437. https://doi.org/10.1158/1055-9965.EPI-10-1190
Prizment AE, Anderson KE, Visvanathan K, Folsom AR (2011) Association of Inflammatory markers with colorectal cancer incidence in the atherosclerosis risk in communities study. Cancer Epidem Biomar 20(2):297–307. https://doi.org/10.1158/1055-9965.EPI-10-1146
Lee S, Choe JW, Kim HK, Sung J (2011) High-sensitivity C-reactive protein and cancer. J Epidemiol 21(3):161–168. https://doi.org/10.2188/jea.je20100128
Aleksandrova K, Jenab M, Boeing H, Jansen E, Bueno-De-Mesquita HB, Rinaldi S et al (2010) Circulating c-reactive protein concentrations and risks of colon and rectal cancer: a nested case-control study within the European prospective investigation into cancer and nutrition. Am J Epidemiol 172(4):407–418. https://doi.org/10.1093/aje/kwq135
Allin KH, Bojesen SE, Nordestgaard BG (2009) Baseline c-reactive protein is associated with incident cancer and survival in patients with cancer. J Clin Oncol 27(13):2217–2224. https://doi.org/10.1200/JCO.2008.19.8440
Gunter MJ, Stolzenberg-Solomon R, Cross AJ, Leitzmann MF, Weinstein S, Wood RJ et al (2006) A prospective study of serum c-reactive protein and colorectal cancer risk in men. Cancer Res 66(4):2483–2487. https://doi.org/10.1158/0008-5472.CAN-05-3631
Siemes C, Visser LE, Coebergh JW, Splinter TAW, Witteman JCM, Uitterlinden AG et al (2006) C-reactive protein levels, variation in the c-reactive protein gene, and cancer risk: the Rotterdam Study. J Clin Oncol 24(33):5216–5222. https://doi.org/10.1200/JCO.2006.07.1381
Otani T, Iwasaki M, Sasazuki S, Inoue M, Tsugane S (2006) Plasma C-reactive protein and risk of colorectal cancer in a nested case-control study: Japan Public Health Center–based prospective study. Cancer Epidem Biomar 15(4):690–695. https://doi.org/10.1158/1055-9965.EPI-05-0708
Ito Y, Suzuki K, Tamakoshi K, Wakai K, Kojima M, Ozasa K et al (2005) Colorectal cancer and serum C-reactive protein levels: a case-control study nested in the JACC Study. J Epidemiol 15 Suppl 2:S185-S189. https://doi.org/10.2188/jea.15.s185
Zhang SM, Buring JE, Lee I, Cook NR, Ridker PM (2005) C-reactive protein levels are not associated with increased risk for colorectal cancer in women. Ann Intern Med 142(6):425. https://doi.org/10.7326/0003-4819-142-6-200503150-00008
Hart PC, Rajab IM, Alebraheem M, Potempa LA (2020) C-reactive protein and cancer-diagnostic and therapeutic insights. Front Immunol 11:595835. https://doi.org/10.3389/fimmu.2020.595835
Hua X, Dai JY, Lindstrom S, Harrison TA, Lin Y, Alberts SR et al (2021) Genetically predicted circulating C-reactive protein concentration and colorectal cancer survival: a Mendelian randomization consortium study. Cancer Epidemiol Biomarkers Prev 30(7):1349–1358. https://doi.org/10.1158/1055-9965.EPI-20-1848
Wang X, Dai JY, Albanes D, Arndt V, Berndt SI, Bézieau S et al (2019) Mendelian randomization analysis of C-reactive protein on colorectal cancer risk. Int J Epidemiol 48(3):767–780. https://doi.org/10.1093/ije/dyy244
Davies NM, Holmes MV, Davey SG (2018) Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 362:k601. https://doi.org/10.1136/bmj.k601
Hinshaw T, Lea S, Arcury J, Parikh AA, Snyder RA (2021) Racial and geographic disparities in stage-specific incidence and mortality in the colorectal cancer hotspot region of eastern North Carolina, 2008–2016. Cancer Causes Control 32(3):271–278. https://doi.org/10.1007/s10552-020-01381-2
Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, Mcglynn KA et al (2020) Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159(1):335–349. https://doi.org/10.1053/j.gastro.2020.02.068
Anand SS, Razak F, Yi Q, Davis B, Jacobs R, Vuksan V et al (2004) C-reactive protein as a screening test for cardiovascular risk in a multiethnic population. Arterioscler Thromb Vasc Biol 24(8):1509–1515. https://doi.org/10.1161/01.ATV.0000135845.95890.4e
Paschke S, Jafarov S, Staib L, Kreuser ED, Maulbecker-Armstrong C, Roitman M et al (2018) Are colon and rectal cancer two different tumor entities? A proposal to abandon the term colorectal cancer. Int J Mol Sci 19(9). https://doi.org/10.3390/ijms19092577
Tamas K, Walenkamp AM, de Vries EG, van Vugt MA, Beets-Tan RG, van Etten B et al (2015) Rectal and colon cancer: not just a different anatomic site. Cancer Treat Rev 41(8):671–679. https://doi.org/10.1016/j.ctrv.2015.06.007
Kalady MF, Sanchez JA, Manilich E, Hammel J, Casey G, Church JM (2009) Divergent oncogenic changes influence survival differences between colon and rectal adenocarcinomas. Dis Colon Rectum 52(6):1039–1045. https://doi.org/10.1007/DCR.0b013e31819edbd4
Kuipers EJ, Grady WM, Lieberman D, Seufferlein T, Sung JJ, Boelens PG et al (2015) Colorectal cancer. Nat Rev Dis Primers 1:15065. https://doi.org/10.1038/nrdp.2015.65
Joshu CE, Tsilidis KK, Peskoe SB, Giardiello FM, Dluzniewski PJ, Nelson WG et al (2014) The association between circulating high-sensitivity C-reactive protein concentration and pathologic measures of colonic inflammation. Cancer Causes Control 25(4):409–418. https://doi.org/10.1007/s10552-014-0343-0
Wu S, Zhu W, Thompson P, Hannun YA (2018) Evaluating intrinsic and non-intrinsic cancer risk factors. Nat Commun 9(1):3490. https://doi.org/10.1038/s41467-018-05467-z
Author information
Authors and Affiliations
Contributions
Liang Han and Xiaoxuan Xie conceived and designed the study; Yongzhong Guo, Xiaoxuan Xie and Dunqiang Ren selected the studies; Hui Hui, Xiaoxuan Xie, and Na Li extracted the data; Yongzhong Guo and Xiaoxuan Xie performed the statistical analyses; Liang Han, Xiaoxuan Xie, Dunqiang Ren, and Yongzhong Guo wrote the manuscript; Liang Han, Xiaoxuan Xie, Yongzhong Guo, and Dunqiang Ren prepared Tables 1 and 2 and Figs. 1, 2, 3, and 4; all authors prepared the supplementary material. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, L., Guo, Y., Ren, D. et al. A predictive role of C-reactive protein in colorectal cancer risk: an updated meta-analysis from 780,985 participants and 11,289 cancer cases. Int J Colorectal Dis 38, 121 (2023). https://doi.org/10.1007/s00384-023-04419-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04419-4