Abstract
Background and aims
Body composition changes in patients with Crohn’s disease (CD) have received increasing attention in recent years. This review aims to describe the changes in body composition in patients with CD on imaging and to analyze and summarize the prognostic value of body composition.
Methods
We systematically searched Web of Science, PubMed, Embase, Cochrane Library, and Medline via OVID for literature published before November 2022, and two researchers independently evaluated the quality of the retrieved literature.
Results
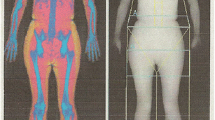
A total of 39 publications (32 cohort studies and 7 cross-sectional studies) involving 4219 patients with CD were retrieved. Imaging methods for body composition assessment, including dual-energy X-ray absorptiometry (DXA), computed tomography (CT) and magnetic resonance imaging (MRI), were included in this review. The study found that patients with CD typically have more visceral adipose tissue and less skeletal muscle mass, and the prevalence of sarcopenia and visceral obesity was significantly different in different studies (sarcopenia: 16–100%; visceral obesity: 5.3–30.5%). Available studies suggest that changes in the body composition of CD patients are significantly related to inflammatory status, disease behavior, poor outcomes, and drug efficacy.
Conclusion
Altered body composition can be a significant predictor of poor outcomes for CD patients. Therefore, the body composition of CD patients may serve as a potential therapeutic target to help optimize disease management strategies in clinical practice.



Similar content being viewed by others
Data availability
Not applicable.
References
Palmese F, Del Toro R, Di Marzio G, Cataleta P, Sama MG, Domenicali M (2021) Sarcopenia and vitamin D deficiency in patients with Crohn’s disease: pathological conditions that should be linked together. Nutrients 13:1378. https://doi.org/10.3390/nu13041378
Vavricka SR, Brun L, Ballabeni P, Pittet V, Prinz VB, Zeitz J et al (2011) Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol 106:110–119. https://doi.org/10.1038/ajg.2010.343
Scaldaferri F, Pizzoferrato M, Lopetuso LR, Musca T, Ingravalle F, Sicignano LL et al (2017) Nutrition and IBD: malnutrition and/or sarcopenia? a practical guide. Gastroenterol Res Pract 2017:8646495. https://doi.org/10.1155/2017/8646495
Prieto JMI, Andrade AR, Magro DO, Imbrizi M, Nishitokukado I, Ortiz-Agostinho CL et al (2021) Nutritional gobal status and its impact in Crohn’s disease. Journal of the Canadian Association of Gastroenterology 4:290–295. https://doi.org/10.1093/jcag/gwab006
Balestrieri P, Ribolsi M, Guarino M, Emerenziani S, Altomare A, Cicala M (2020) Nutritional aspects in inflammatory bowel diseases. Nutrients 12. https://doi.org/10.3390/nu12020372
Cioffi I, Marra M, Imperatore N, Pagano MC, Santarpia L, Alfonsi L et al (2020) Assessment of bioelectrical phase angle as a predictor of nutritional status in patients with Crohn’s disease: a cross sectional study. Clin Nutr 39:1564–1571. https://doi.org/10.1016/j.clnu.2019.06.023
Ding NS, Tassone D, Al Bakir I, Wu K, Thompson AJ, Connell WR et al (2022) Systematic review: the impact and importance of body composition in inflammatory bowel disease. J Crohns Colitis 16:1475–1492. https://doi.org/10.1093/ecco-jcc/jjac041
Adams DW, Gurwara S, Silver HJ, Horst SN, Beaulieu DB, Schwartz DA et al (2017) Sarcopenia is common in overweight patients with inflammatory bowel disease and may predict need for surgery. Inflamm Bowel Dis 23:1182–1186. https://doi.org/10.1097/MIB.0000000000001128
Grillot J, D’Engremont C, Parmentier AL, Lakkis Z, Piton G, Cazaux D et al (2020) Sarcopenia and visceral obesity assessed by computed tomography are associated with adverse outcomes in patients with Crohn’s disease. Clin Nutr 39:3024–3030. https://doi.org/10.1016/j.clnu.2020.01.001
Magro DO, Barreto M, Cazzo E, Camargo MG, Kotze PG, Coy C (2018) Visceral fat is increased in individuals with Crohn’s disease: A comparative analysis with healthy controls. Arq Gastroenterol 55:142–147. https://doi.org/10.1590/S0004-2803.201800000-25
Kullberg J, Brandberg J, Angelhed JE, Frimmel H, Bergelin E, Strid L et al (2009) Whole-body adipose tissue analysis: comparison of MRI, CT and dual energy X-ray absorptiometry. Br J Radiol 82:123–130. https://doi.org/10.1259/bjr/80083156
Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL (2012) Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity (Silver Spring) 20:1109–1114. https://doi.org/10.1038/oby.2011.367
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in older people. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T et al (2019) GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr 38:1–9. https://doi.org/10.1016/j.clnu.2018.08.002
Cushing KC, Kordbacheh H, Gee MS, Kambadakone A, Ananthakrishnan AN (2018) Sarcopenia is a novel predictor of the need for rescue therapy in hospitalized ulcerative colitis patients. J Crohns Colitis 12:1036–1041. https://doi.org/10.1093/ecco-jcc/jjy064
Ryan E, McNicholas D, Creavin B, Kelly ME, Walsh T, Beddy D (2019) Sarcopenia and inflammatory bowel disease: A systematic review. Inflamm Bowel Dis 25:67–73. https://doi.org/10.1093/ibd/izy212
Rivera ED, Coffey JC, Walsh D, Ehrenpreis ED (2019) The mesentery, systemic inflammation, and Crohn’s disease. Inflamm Bowel Dis 25:226–234. https://doi.org/10.1093/ibd/izy201
Sheehan AL, Warren BF, Gear MW, Shepherd NA (1992) Fat-wrapping in Crohn’s disease: pathological basis and relevance to surgical practice. Br J Surg 79:955–958. https://doi.org/10.1002/bjs.1800790934
Karaskova E, Velganova-Veghova M, Geryk M, Foltenova H, Kucerova V, Karasek D (2021) Role of adipose tissue in inflammatory bowel disease. Int J Mol Sci 22. https://doi.org/10.3390/ijms22084226
Ananthakrishnan AN (2021) Frailty in patients with inflammatory bowel disease. Gastroenterol Hepatol (N Y) 17:263–268
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Plos Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Schneider SM, Al-Jaouni R, Filippi J, Wiroth J, Zeanandin G, Arab K et al (2008) Sarcopenia is prevalent in patients with Crohnʼs disease in clinical remission. Inflamm Bowel Dis 14:1562–1568. https://doi.org/10.1002/ibd.20504
Katznelson L, Fairfield WP, Zeizafoun N, Sands BE, Peppercorn MA, Rosenthal DI et al (2003) Effects of growth hormone secretion on body composition in patients with Crohn’s disease. J Clin Endocrinol Metab 88:5468–5472. https://doi.org/10.1210/jc.2003-030608
Tjellesen L, Nielsen PK, Staun M (1998) Body composition by Dual-Energy X-Ray absorptiometry in patients with Crohn’s disease. Scand J Gastroentero 33:956–960. https://doi.org/10.1080/003655298750026985
Büning C, von Kraft C, Hermsdorf M, Gentz E, Wirth EK, Valentini L et al (2015) Visceral adipose tissue in patients with Crohnʼs disease correlates with disease activity, inflammatory markers, and outcome. Inflamm Bowel Dis 21:2590–2597. https://doi.org/10.1097/MIB.0000000000000527
Zhang X, Peng K, Li G, Wan L, Xu T, Cui Z et al (2022) Evaluation of bone mineral density and body compositions interrelation in young and middle-aged male patients with Crohn’s disease by quantitative computed tomography. Front Endocrinol 13. https://doi.org/10.3389/fendo.2022.953289
Carvalho D, Viana C, Marques I, Costa C, Martins SF (2019) Sarcopenia is associated with postoperative outcome in patients with Crohn’s disease undergoing bowel resection. Gastrointestinal Disorders 1:201–209. https://doi.org/10.3390/gidisord1010015
Hong JT, James S, Tran A, Kutaiba N (2022) Sarcopenia measurements and clinical outcomes in Crohn’s disease surgical patients. Anz J Surg. https://doi.org/10.1111/ans.18063
Nardone OM, Ponsiglione A, de Sire R, Calabrese G, Liuzzi R, Testa A et al (2022) Impact of sarcopenia on clinical outcomes in a cohort of caucasian active Crohn’s disease patients undergoing multidetector CT-enterography. Nutrients 14:3460. https://doi.org/10.3390/nu14173460
Zhang Z, Yu X, Fang N, Long X, Ruan X, Qiu J et al (2022) Can visceral adipose tissue and skeletal muscle predict recurrence of newly diagnosed Crohn’s disease in different treatments. BMC Gastroenterol 22. https://doi.org/10.1186/s12876-022-02327-5
Yasueda A, Sekido Y, Takeda T, Ogino T, Miyoshi N, Takahashi H et al (2022) Sarcopenia hinders the decline in disease activity after surgery for people with Crohn's disease: Preliminary results. Nutrition 94:111526. https://doi.org/10.1016/j.nut.2021.111526
Ando K, Uehara K, Sugiyama Y, Kobayashi Y, Murakami Y, Sato H et al (2022) Correlation among body composition parameters and long-term outcomes in Crohn's disease after anti-TNF therapy. Front Nutr 9. https://doi.org/10.3389/fnut.2022.765209
Argeny S, Tamandl D, Scharitzer M, Stift A, Bergmann M, Riss S et al (2018) Visceral fat area measured with computed tomography does not predict postoperative course in Crohn´s disease patients. Plos One
Boparai G, Kedia S, Kandasamy D, Sharma R, Madhusudhan KS, Dash NR et al (2021) Combination of sarcopenia and high visceral fat predict poor outcomes in patients with Crohn’s disease. Eur J Clin Nutr 75:1491–1498. https://doi.org/10.1038/s41430-021-00857-x
Bryant RV, Schultz CG, Ooi S, Goess C, Costello SP, Vincent AD et al (2019) Visceral adipose tissue is associated with stricturing Crohn’s disease behavior, fecal calprotectin, and quality of life. Inflamm Bowel Dis 25:592–600. https://doi.org/10.1093/ibd/izy278
Connelly TM, Juza RM, Sangster W, Sehgal R, Tappouni RF, Messaris E (2014) Volumetric fat ratio and not body mass index is predictive of ileocolectomy outcomes in Crohn’s disease patients. Digest Surg 31:219–224. https://doi.org/10.1159/000365359
Cravo ML, Velho S, Torres J, Costa SM, Palmela C, Cruz R et al (2017) Lower skeletal muscle attenuation and high visceral fat index are associated with complicated disease in patients with Crohn’s disease: an exploratory study. Clin Nutr ESPEN 21:79–85. https://doi.org/10.1016/j.clnesp.2017.04.005
Ding NS, Malietzis G, Lung PFC, Penez L, Yip WM, Gabe S et al (2017) The body composition profile is associated with response to anti-TNF therapy in Crohn’s disease and may offer an alternative dosing paradigm. Aliment Pharm Ther 46:883–891. https://doi.org/10.1111/apt.14293
Ding Z, Wu XR, Remer EM, Lian L, Stocchi L, Li Y et al (2016) Association between high visceral fat area and postoperative complications in patients with Crohn’s disease following primary surgery. Colorectal Dis 18:163–172. https://doi.org/10.1111/codi.13128
Erhayiem B, Dhingsa R, Hawkey CJ, Subramanian V (2011) Ratio of visceral to subcutaneous fat area is a biomarker of complicated Crohn’s disease. Clin Gastroenterol Hepatol 9:684–687. https://doi.org/10.1016/j.cgh.2011.05.005
Galata C, Hodapp J, Weiß C, Karampinis I, Vassilev G, Reißfelder C et al (2020) Skeletal muscle mass index predicts postoperative complications in intestinal surgery for Crohn’s disease. Jpen-Parenter Enter 44:714–721. https://doi.org/10.1002/jpen.1696
Holt DQ, Moore GT, Strauss BJ, Hamilton AL, De Cruz P, Kamm MA (2017) Visceral adiposity predicts post-operative Crohn’s disease recurrence. Aliment Pharmacol Ther 45:1255–1264. https://doi.org/10.1111/apt.14018
Labarthe G, Dolores M, Verdalle-Cazes M, Charpentier C, Roullee P, Dacher JN et al (2020) Magnetic resonance imaging assessment of body composition parameters in Crohn’s disease. Dig Liver Dis 52:878–884. https://doi.org/10.1016/j.dld.2020.06.024
Lee CH, Yoon H, Oh DJ, Lee JM, Choi YJ, Shin CM et al (2020) The prevalence of sarcopenia and its effect on prognosis in patients with Crohn’s disease. Intest Res 18:79–84. https://doi.org/10.5217/ir.2019.00107
Li Y, Zhu W, Gong J, Zhang W, Gu L, Guo Z et al (2015) Visceral fat area is associated with a high risk for early postoperative recurrence in Crohn’s disease. Colorectal Dis 17:225–234. https://doi.org/10.1111/codi.12798
Lim Z, Welman CJ, Raymond W, Thin L (2020) The effect of adiposity on anti-tumor necrosis fctor-alpha levels and loss of response in Crohn's disease patients. Clin Transl Gastroenterol 11:e233. https://doi.org/10.14309/ctg.0000000000000233
Pozios I, Kaufmann D, Boubaris K, Seeliger H, Weixler B, Stroux A et al (2022) Impact of myopenia and myosteatosis on postoperative outcome and recurrence in Crohn’s disease. Int J Colorectal Dis 37:791–804. https://doi.org/10.1007/s00384-022-04104-y
Shen W, Cao L, Li Y, Cai X, Ge Y, Zhu W (2018) Visceral fat is associated with mucosal healing of infliximab treatment in Crohn’s disease. Dis Colon Rectum 61:706–712. https://doi.org/10.1097/DCR.0000000000001074
Subramaniam K, Fallon K, Ruut T, Lane D, McKay R, Shadbolt B et al (2015) Infliximab reverses inflammatory muscle wasting (sarcopenia) in Crohn’s disease. Aliment Pharm Ther 41:419–428. https://doi.org/10.1111/apt.13058
Thiberge C, Charpentier C, Gillibert A, Modzelewski R, Dacher J, Savoye G et al (2018) Lower subcutaneous or visceral adiposity assessed by abdominal computed tomography could predict adverse outcome in patients with Crohn’s disease. J Crohns Colitis 12:1429–1437. https://doi.org/10.1093/ecco-jcc/jjy124
Van Der Sloot KWJ, Joshi AD, Bellavance DR, Gilpin KK, Stewart KO, Lochhead P et al (2017) Visceral adiposity, genetic susceptibility, and risk of complications among individuals with Crohnʼs disease. Inflamm Bowel Dis 23:82–88. https://doi.org/10.1097/MIB.0000000000000978
Xiong Z, Zhou Z, Hao L, Li Y, Hu X, Hu D et al (2022) The relationship between perianal fistula activity and abdominal adipose tissue in Crohn’s disease: an observational study. Insights into Imaging 13. https://doi.org/10.1186/s13244-022-01293-6
Yuan G, He Y, Cao Q, Tang M, Xie Z, Qiu Y et al (2022) Visceral adipose volume is correlated with surgical tissue fibrosis in Crohn's disease of the small bowel. Gastroenterol Rep 10. https://doi.org/10.1093/gastro/goac044
Zager Y, Khalilieh S, Ganaiem O, Gorgov E, Horesh N, Anteby R et al (2021) Low psoas muscle area is associated with postoperative complications in Crohn’s disease. Int J Colorectal Dis 36:543–550. https://doi.org/10.1007/s00384-020-03799-1
Zhang C, Yu D, Hong L, Zhang T, Liu H, Fan R et al (2021) Prevalence of Sarcopenia and its effect on postoperative complications in patients with Crohn’s disease. Gastroent Res Pract 2021:1–8. https://doi.org/10.1155/2021/3267201
Zhang T, Cao L, Cao T, Yang J, Gong J, Zhu W et al (2017) Prevalence of sarcopenia and its impact on postoperative outcome in patients with Crohn’s disease undergoing bowel resection. JPEN. J Parenter Enter Nutr 41:592–600. https://doi.org/10.1177/0148607115612054
Zhou Z, Xiong Z, Shen Y, Li Z, Hu X, Hu D (2021) Magnetic resonance imaging-based body composition is associated with nutritional and inflammatory status: a longitudinal study in patients with Crohn’s disease. Insights Imaging 12:178. https://doi.org/10.1186/s13244-021-01121-3
Zhou Z, Xiong Z, Xie Q, Xiao P, Zhang Q, Gu J et al (2021) Computed tomography-based multiple body composition parameters predict outcomes in Crohn’s disease. Insights Imaging 12:135. https://doi.org/10.1186/s13244-021-01083-6
Gomez-Perez SL, Haus JM, Sheean P, Patel B, Mar W, Chaudhry V et al (2016) Measuring abdominal circumference and skeletal muscle from a single Cross-Sectional computed tomography image: a step-by step guide for clinicians using national institutes of health ImageJ. JPEN J Parenter Enteral Nutr 40:308–318. https://doi.org/10.1177/0148607115604149
Bani HE, Demontiero O, Vogrin S, Ng A, Duque G (2018) Marrow adipose tissue in older men: association with visceral and subcutaneous fat, bone volume, metabolism, and inflammation. Calcif Tissue Int 103:164–174. https://doi.org/10.1007/s00223-018-0412-6
Ha C, Martin A, Sepich-Poore GD, Shi B, Wang Y, Gouin K et al (2020) Translocation of viable gut microbiota to mesenteric adipose drives formation of creeping fat in humans. Cell 183:666–683. https://doi.org/10.1016/j.cell.2020.09.009
Dhaliwal A, Quinlan JI, Overthrow K, Greig C, Lord JM, Armstrong MJ et al (2021) Sarcopenia in inflammatory bowel disease: A narrative overview. Nutrients 13:656. https://doi.org/10.3390/nu13020656
Ehlers L, Bannert K, Rohde S, Berlin P, Reiner J, Wiese M et al (2020) Preclinical insights into the gut-skeletal muscle axis in chronic gastrointestinal diseases. J Cell Mol Med 24:8304–8314. https://doi.org/10.1111/jcmm.15554
Marco P, Roberto DS, Fabio I, Maria CM, Valentina P, Anna MM et al (2019) Characterization of sarcopenia in an IBD population attending an italian gastroenterology tertiary center. Nutrients 11
Cohen S, Nathan JA, Goldberg AL (2015) Muscle wasting in disease: molecular mechanisms and promising therapies. Nat Rev Drug Discov 14:58–74. https://doi.org/10.1038/nrd4467
Chen L, Woo J, Assantachai P, Auyeung T, Chou M, Iijima K et al (2020) Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 21:300–307. https://doi.org/10.1016/j.jamda.2019.12.012
Wan Y, Zhang D, Xing T, Liu Q, Chi Y, Zhang H et al (2021) The impact of visceral obesity on chronic constipation, inflammation, immune function and cognitive function in patients with inflammatory bowel disease. Aging (Albany NY) 13:6702–6711. https://doi.org/10.18632/aging.202526
Barajas Ordonez F, Melekh B, Rodríguez-Feria P, Damm R, Thormann M, March C et al (2023) Parameters of body composition and creeping fat are associated with activity of Crohn’s disease. Magn Reson Imaging 98:1–6. https://doi.org/10.1016/j.mri.2023.01.005
Barajas Ordonez F, Melekh B, Rodríguez-Feria P, Melekh O, Thormann M, Damm R et al (2023) Body composition predictors of complicated Crohn’s disease. Dig Dis. https://doi.org/10.1159/000529426
Bamba S, Inatomi O, Takahashi K, Morita Y, Imai T, Ohno M et al (2021) Assessment of body composition from CT images at the level of the third lumbar vertebra in inflammatory bowel disease. Inflamm Bowel Dis 27:1435–1442. https://doi.org/10.1093/ibd/izaa306
Karmiris K, Koutroubakis IE, Xidakis C, Polychronaki M, Kouroumalis EA (2007) The effect of infliximab on circulating levels of leptin, adiponectin and resistin in patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol 19:789–794. https://doi.org/10.1097/MEG.0b013e3282202bca
Ziegler JF, Bottcher C, Letizia M, Yerinde C, Wu H, Freise I et al (2019) Leptin induces TNFalpha-dependent inflammation in acquired generalized lipodystrophy and combined Crohn’s disease. Nat Commun 10:5629. https://doi.org/10.1038/s41467-019-13559-7
Gu P, Chhabra A, Chittajallu P, Chang C, Mendez D, Gilman A et al (2022) Visceral adipose tissue volumetrics inform odds of treatment response and risk of subsequent surgery in IBD patients starting antitumor necrosis factor therapy. Inflamm Bowel Dis 28:657–666. https://doi.org/10.1093/ibd/izab167
Funding
This research was funded by the Chongqing Science and Technology Bureau of Science and Technology Innovation and Application Development Special (Grant No. cstc2020jscx-sbqwX0015) and Chongqing Postgraduate Research Innovation Project (Grant No. CYS22391).
Author information
Authors and Affiliations
Contributions
Conceptualization, Wuli Tang and Kang Li; literature search, Wuli Tang; software, Gang Xie; validation, Danni Wang and Ting Li; formal analysis, Wangli Tang; investigation, Junlin Li; resources, Wuli Tang; data curation, Junlin Li and Jiaxing Deng; writing—original draft preparation, Wuli Tang; writing—review and editing, Gang Xie and Kang Li; funding acquisition, Wuli Tang and Kang Li. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, W., Xie, G., Wang, D. et al. Imaging-based assessment of body composition in patients with Crohn’s disease: a systematic review. Int J Colorectal Dis 38, 126 (2023). https://doi.org/10.1007/s00384-023-04413-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04413-w