Abstract
Aim
The purpose of this study was to explore the clinical factors associated with achieving good response after neoadjuvant chemoradiotherapy (nCRT) in patients with locally advanced rectal cancer (LARC) and to develop and validate a nomogram.
Methods
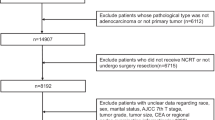
A total of 1724 consecutive LARC patients treated at Fujian Medical University Union Hospital from January 2010 to December 2021 were retrospectively evaluated as the training cohort; 267 consecutive LARC patients treated at Zhangzhou Affiliated Hospital of Fujian Medical University during the same period were evaluated as the external 2 cohorts. Based on the pathological results after radical surgery, treatment response was defined as follows: good response, stage ypT0∼2N0M0 and poor response, ypT3∼4N0M0 and/or N positive. Independent influencing factors were analyzed by logistic regression, a nomogram was developed and validated, and the model was evaluated using internal and external data cohorts for validation.
Results
In the training cohort, 46.6% of patients achieved good response after nCRT combined with radical surgery. The rate of the retained anus was higher in the good response group (93.5% vs. 90.7%, P < 0.001). Cox regression analysis showed that the risk of overall survival and disease-free survival was significantly lower among good response patients than poor response patients, HR = 0.204 (95%CI: 0.146–0.287). Multivariate logistic regression analysis showed an independent association with 9 clinical factors, including histopathology, and a nomogram with an excellent predictive response was developed accordingly. The C-index of the predictive accuracy of the nomogram was 0.764 (95%CI: 0.742–0.786), the internal validation of the 200 bootstrap replication mean C-index was 0.764, and the external validation cohort showed an accuracy C-index of 0.789 (95%CI: 0.734–0.844), with good accuracy of the model.
Conclusion
We identified factors associated with achieving good response in LARC after treatment with nCRT and developed a nomogram to contribute to clinical decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rectal cancer with characteristics such as anatomical proximity to the sphincter structure, high local recurrence rate, and different metastatic behavior requires multiple means of combined and comprehensive treatment to obtain better outcomes [1]. In recent years, neoadjuvant chemoradiotherapy (nCRT) combined with total mesorectal excision (TME) has become the standard treatment mode for locally advanced rectal cancer (LARC) [2]. However, in clinical practice, the tumor response after nCRT in LARC patients varies according to individual differences, and some patients have a good tumor response; i.e., the tumor cells in radical surgical resection specimens infiltrate within the rectal muscular layer (ypT0∼2) and have no lymph node metastasis (N0) or even partially achieve a pathological complete response (pCR) [3]. This not only reduces the local recurrence rate but also results in a better prognosis. Meanwhile, selective ypT0∼2N0 patients are considered potential candidates for anal organ preservation [4]. However, due to the heterogeneity of rectal cancer, another proportion of patients respond poorly to nCRT, resulting in prolonged waiting time for surgery and increased risk of distant metastasis. Reportedly, 30∼40% of patients respond poorly after nCRT treatment, 20∼30% of patients fail to respond, and in a few cases, tumor progression even occurs [5].
Individually tailored treatment is urgently needed to develop tools that can accurately predict whether LARC patients will have a good response after nCRT treatment even before treatment decisions are made to help develop the best comprehensive treatment strategy in clinical work and allow some patients to be exempted from nCRT treatment [6]. The nomogram is a popular and well-visualized tool for predicting outcomes in the clinic and has been widely used to predict the different responses after nCRT among LARC patients [7, 8]. The purpose of this study was to explore the clinical factors associated with LARC patients achieving a good response after nCRT and to develop and validate a nomogram that can be used to predict good response before treatment decisions are made, as well as to assess the prognosis of good or poor tumor response.
Patients and methods
Patient selection
Consecutive patients with LARC treated at the Union Hospital of Fujian Medical University from January 2010 to December 2021 were retrospectively evaluated as the training cohort; consecutive patients with LARC treated at the Department of Colorectal and Anal Surgery of the Zhangzhou Hospital of Fujian Medical University during the same period were evaluated as the external validation cohort.
The inclusion criteria were as follows: ① pathologically confirmed rectal cancer; ② a clinical stage of cII or cIII (cT3∼4N0∼2M0) determined by two imaging experts according to the American Joint Committee on Cancer (AJCC) 8th edition colorectal cancer staging criteria; ③ completed nCRT combined with radical surgery; ④ complete clinicopathological features and follow-up data; and ⑤ signed informed consent form. The exclusion criteria were as follows: ① recurrence of rectal cancer; ② distant organ metastasis before treatment; ③ preoperative combined intestinal obstruction, perforation, intestinal bleeding, and other patients requiring emergency surgical resection; ④ death within 60 days after surgery; ⑤ first diagnosis combined with simultaneous or heterochronous malignant tumors from another organ. This study was approved by the Ethics Committee of Zhangzhou Affiliated Hospital of Fujian Medical University and Fujian Medical University Union Hospital (2020LWB078).
Treatment
The comprehensive treatment plan was as follows: All patients received concurrent radiotherapy, with radiation therapy in the form of 3-dimensional conformal radiation therapy (3DCRT) or intensity-modulated radiation therapy (IMRT) and concurrent oral fluorouracil-based chemotherapy during radiotherapy. The long-course radiotherapy dose was 45.0∼50.4 Gy 25∼28 times, and the short-course radiotherapy dose was 25 Gy 5 times. The patients underwent neoadjuvant chemotherapy within 1 week following the completion of radiotherapy and while awaiting surgery. The neoadjuvant chemotherapy regimen was mFolFox6 (total fluorouracil 2600 mg/m2, calcium folinate 400 mg/m2, oxaliplatin 85 mg/m2) or Xelox (capecitabine 1000 mg/m2 bid, oxaliplatin 130 mg/m2). TME surgery was performed after a median time interval of 6–8 weeks after radiotherapy. Laparoscopic, robot, or open surgery was used.
Definitions
The classification criteria were as follows: Specimens of all cases were reviewed by 2 pathologists in their units for pathological findings. Based on postoperative pathological examinations as criteria, treatment response was defined as follows: good response, stage ypT0∼2N0M0 and as the primary study endpoint in this study; and poor response, stage ypT3∼4N0M0 or N positive [3, 8]. pCR was defined as complete tumor regression, no found tumor cells, and those patients with only fibroblasts remaining would not receive postoperative adjuvant chemotherapy after surgery, whereas the remaining patients continued the total preoperative and postoperative courses of chemotherapy for a cumulative period of 6 months. After comprehensive treatment, follow-ups were conducted by telephone and outpatient visits. The follow-up period ended in June 2022.
Statistical analysis
T tests, chi-square tests, and Fisher’s exact tests were used to analyze whether the differences between the training cohort and external validation cohort were statistically significant. Binary logistic regression analysis was used for variable analysis and selected variables as the basis for model construction. The Cox regression analysis method was used for the comparison of DFS and OS. SPSS 25.0 (IBM SPSS Statistics, Chicago, IL, USA) software was used for statistical analysis. P < 0.05 indicated that the difference was statistically significant. Independent factors were introduced into R 4.1.1 (http://www.r-project.org) software to create a nomogram using R packages such as car, pROC, and survivor. Internal validation of the model was performed using 200 bootstrap replications with put back sampling. External validation was also performed using validation cohort data. The accuracy of the model was judged by the consistency index (C-index). Calibration curves were used to evaluate the consistency of the model’s predicted results with the actual results. Decision curve analysis (DCA) was used to assess whether there was clinical benefit.
Results
Finally, the training cohort included 1724 consecutive patients, and the external validation cohort included 267 consecutive patients. The general clinical characteristics of both groups are shown in Table 1. The two groups had good tumor responses of 46.6% and 43.8%, respectively, and the difference between the two groups was not statistically significant (P = 0.391); the follow-up times were 50.0 ± 24.2 months and 25.0 ± 22.79 months, respectively (Table 1).
In the training cohort, recent outcomes showed that while the tumors were lower relative to the anal verge in the patients with good response than in the patients with poor response (≤ 8 cm, 90.7% vs. 84.9%, P < 0.001), the patients who had a good response ultimately had a greater chance of preserving the anal sphincter (93.5% vs. 90.7%, P < 0.001). Among the patients who had a poor response, 9.6% suffered distant metastases after nCRT treatment (Table 2).
The long-term outcome was analyzed by survival curve results, and DFS and OS were significantly better among patients with good response than among patients with poor response (5-year OS: 93.7% vs. 72.1%; 5-year DFS: 90.8% vs. 63.8%; all P < 0.001), HR = 0.204 (95%CI: 0.146–0.287) (Fig. 1A, B).
Univariate logistic regression analysis indicated that the differences in histopathology, distance to the anal verge (DTAV), pre-CRT circumferential resection margin (CRM), pre-CRT magnetic resonance imaging (MRI), extramural venous invasion (EMVI), pre-CRT MRI T stage, pre-CRT lymph node metastasis status, total neoadjuvant therapy (TNT), interval to surgery, and whole circumference of the rectal wall were all statistically significant (all P < 0.05) (Table 3).
Independent factors associated with good response were further analyzed. The results of multivariate logistic regression analysis showed that histopathological diagnosis of nonspecific adenocarcinoma (OR = 4.697, 95%CI: 3.216–6.862; P < 0.001), DTAV > 8 cm (OR = 0.639, 95%CI: 0.460–0.889; P = 0.008), pre-CRT CEA (carcinoembryonic antigen) > 5 ng/ml (OR = 0.428, 95%CI: 0.343–0.535; P < 0.001), positive pre-CRT MRI EMVI positive (OR = 0.447, 95%CI: 0.338–0.591; P < 0.001), pre-CRT MRI T stage cT4 (OR = 0.754, 95%CI: 0.621–0.914; P = 0.004), positive pre-CRT LN metastasis (OR = 0.415, 95%CI: 0.317–0.542; P < 0.001), total neoadjuvant therapy (OR = 1.929, 95%CI: 1.121–3.318; P = 0.018), interval to surgery (OR = 1.055, 95%CI: 1.018–1.092; P = 0.003), and whole circumference of the rectal wall (OR = 0.446, 95%CI: 0.334–0.597; P < 0.001) were independent influencing factors for good response (Table 3).
Nine independent factors were included in the construction of the nomogram for LARC patients with good response after nCRT treatment (Fig. 2). The C-index of the predictive accuracy of the nomogram (Fig. 3A) was 0.764 (95%CI: 0.742–0.786), and the average C-index of the final model in internal validation using the 200 bootstrap replication sampling method was 0.764. The model had good accuracy. The external validation cohort (n = 267) showed an accuracy C-index (Fig. 3B) of 0.789 (95%CI: 0.734–0.844). The calibration curves (Fig. 4A, B) showed good agreement between the predicted probabilities and the actual observations of the obtained response prediction model for the training cohort and external validation cohort. The decision curve analysis (Fig. 5A, B) lies above both the None and All lines, quantitatively showing that the model has clinical utility.
Discussion
Previous research mostly defined the study endpoint as pCR after LARC treated with nCRT [9, 10], but in practice, there are still difficulties in implementing methods including watch and wait and endoscopic transanalresection, even after achieving clinical complete remission (cCR); most patients still undergo TME surgery. Due to the excellent prognosis, patients defined as having a good response, including pCR and stage yp I patients, are the population with the greatest benefit after nCRT, but this population has rarely been studied, and no reliable predictive models are available. Therefore, this study retrospectively included consecutive patients from two major colorectal cancer consultation centers in China, and the study identified independent influencing factors for attaining good response after nCRT in LARC patients and established a nomogram to help clinical decision-making.
A meta-analysis that included more than 40,000 patients showed that the prognosis of patients after LARC treated with nCRT depended on the post-treatment pathological stage and was not related to the pretreatment clinical stage [11]. Tumor regression after nCRT can accurately predict whether patient prognoses can improve. The results of this study showed that 46.6% of patients in the training cohort had a good response, with significant downstaging or even pCR, and the long-term prognosis was significantly better than that in the poor response group, which is consistent with the results of previous studies [6]. Patients who achieve cCR or near cCR as assessed by strict selection criteria can be managed with watch and wait and endoscopic transanal resection to preserve the rectum [12]. In this study, compared to the patients with a poor response, a lower distance to the anal verge of the tumor was observed among patients with a good response (P > 0.05); however, more patients experienced preservation of the anal organ. The construction and application of this model has significant clinical significance. However, there is still no reasonable and effective screening tool to help select the right patients for the best treatment plan to improve treatment efficiency.
The development of a treatment plan for rectal cancer depends on the evaluation of high-resolution rectal MRI. Accurate clinical staging, including the depth of tumor infiltration, the presence of lymph node metastasis, CRM, and EMVI, is a prerequisite for deciding whether a patient should receive nCRT treatment. The efficacy of nCRT needs to be dynamically evaluated during the treatment process so that the treatment plan can be adjusted in time and the best timing of surgery can be achieved. Several studies have been devoted to exploring whether comprehensive pretreatment MRI features can be used for the early prediction of LARC response to nCRT, and studies have shown good predictive performance for models predicting treatment response, with AUC ranges as high as 0.793∼0.940 [13,14,15].
Wan et al. included 2267 LARC patients to compare the prognostic impact of different interval to surgery times, and as a result, fewer survival outcomes were observed in the shortest interval time group, and interval times longer than 13 weeks were associated with lower DFS rates (HR = 0.884, 95%CI: 0.778 to 0.921, P < 0.001) [16]. A meta-analysis evaluated the TNT regimen used for an extended interval time and showed that the pCR rate was 22.4% (95%CI: 19.4∼25.7%) and that TNT increased the odds of pCR by 40% (1.40, 95%CI: 1.08∼1.81, p = 0.010) [17]. As the application of nCRT expands and clinical research continues, it is becoming increasingly important to establish the optimal interval time between final radiotherapy and surgery to achieve the maximum number of patient benefits [18].
The impact of circumferential tumor location on neoadjuvant therapy has been rarely studied, and our center’s study was the first to find a higher proportion of pCR among patients with tumors located in the anterior rectal wall (26.7% in the anterior wall vs. 20.0% in the lateral wall vs. 12.3% in the posterior wall, P = 0.006), but the exact mechanism remains unknown [19]. Similar to the present study, it was concluded that patients with tumors occupying the whole range of rectal wall circumference had a lower proportion of good response, and tumors occupying different circumferential positions, including the lateral wall and posterior wall, in this group of patients with greater tumor burden may respond poorly to nCRT. This new finding helps to improve prediction accuracy and can be further studied in the future. Additionally, the shorter the DTAV was, the greater the use of neoadjuvant therapy (< 5 cm, 75.2% vs. 38.0%; P < 0.001) [20]; a DTAV ≤ 5 cm independently predicted the rate of tumor downstaging (OR = 2.66, 95%CI: 1.72–4.40, P < 0.001) [21]. Similar to this study, low rectal occupation was higher (≤ 8 cm, 87.6%), and there was an independent association between lower tumor location and good response (> 8 cm, OR = 0.639, 95%CI: 0.460–0.889, P = 0.008).
The nomogram, as a visual predictive tool, is easy to use and understand, and it can be easily used in the clinic to calculate the probability of disease occurrence and treatment efficacy and determine the prognosis of patients based on the graph [6, 7, 15, 22]. Some studies have compared nomograms with the traditional tumor-node-metastasis stage (TNM stage) system, which has specific advantages in determining treatment efficacy and tumor prognosis, even though tumors of the same stage still differ in terms of survival and local recurrence rates according to certain factors affecting prognosis [15, 22]. The model constructed in this study was internally and externally validated and confirmed to accurately and individually estimate the probability of whether patients will obtain good response after nCRT, which is a major advantage over the estimates provided by the current TNM system. The usefulness of this nomogram for clinical decision-making can be confirmed by decision curve analysis (DCA), which helps to guide the treatment choice more accurately for the benefit of the patient [23].
Based on very few previous studies of this population, most focused on predictions for pCR patients [3, 6, 7], Zhang et al. considered good response as a predictive endpoint and developed a nomogram model C-index of 0.760 (95%CI: 0.681–0.844), but the study had a smaller sample size, fewer included factors in the model, and no external validation, with lower predictive accuracy than the present study [8]. This study was based on a retrospective cohort analysis of patients from two large colorectal consultation centers to compensate for the predictive model for this population, and the model was applied in an external institution for validation, with some external applicability to help clinical decision-making. There are also limitations in this study, as it was based on a retrospective cohort analysis with some selection bias; patients with incomplete clinical data were excluded, and the probability of good response may be overestimated or underestimated. In the future, as research on colorectal cancer progresses, many new prognosis-related variables, including microsatellite status (MSS), RAS, and BRAF genes, will be gradually discovered. The nomogram model used to predict good response should also be updated to obtain more accurate predictive assessment efficacy.
In conclusion, LARC treated with nCRT had a high probability of a good response, and patients with a good response not only had a greater chance of preserving the anal organ but also had a better prognosis. The nomogram was created to help clinicians predict the likely outcome of treatment, reduce unnecessary radiation therapy for some patients, and help LARC patients choose the best treatment option.
Data availability
All data obtained or analyzed during this work are included within the article.
References
Wiegering A, Isbert C, Dietz UA et al (2014) Multimodal therapy in treatment of rectal cancer is associated with improved survival and reduced local recurrence - a retrospective analysis over two decades. BMC Cancer 14:816. https://doi.org/10.1186/1471-2407-14-816
Benson AB, Venook AP, Al-Hawary MM et al (2018) Rectal cancer, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 16(7):874–901. https://doi.org/10.6004/jnccn.2018.0061
Pang X, Gao Y, Yi H, Liu H, Liu S, Zheng J (2021) Associations between clinical characteristics and tumor response to neoadjuvant chemoradiotherapy in rectal cancer. Cancer Med 10(14):4832–4843. https://doi.org/10.1002/cam4.4051
Lee L, Kelly J, Nassif GJ et al (2017) Chemoradiation and local excision for T2N0 rectal cancer offers equivalent overall survival compared to standard resection: a national cancer database analysis. J Gastrointest Surg 21(10):1666–1674. https://doi.org/10.1007/s11605-017-3536-5
Del Carmen S, Corchete LA, González Velasco C et al (2021) High-risk clinicopathological and genetic features and outcomes in patients receiving neoadjuvant radiochemotherapy for locally advanced rectal cancer. Cancers (Basel). 13:3166. https://doi.org/10.3390/cancers13133166
Li Y, Wang J, Ma X et al (2016) A review of neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Int J Biol Sci 12(8):1022–1031. https://doi.org/10.7150/ijbs.15438
Sun Y, Chi P, Lin H et al (2017) A nomogram predicting pathological complete response to neoadjuvant chemoradiotherapy for locally advanced rectal cancer: implications for organ preservation strategies. Oncotarget 8(40):67732–67743. https://doi.org/10.18632/oncotarget.18821
Zhang J, Cai Y, Hu H et al (2016) Nomogram basing pre-treatment parameters predicting early response for locally advanced rectal cancer with neoadjuvant chemotherapy alone: a subgroup efficacy analysis of FOWARC study. Oncotarget 7(4):5053–5062. https://doi.org/10.18632/oncotarget.6469
Huang CM, Huang MY, Huang CW et al (2020) Machine learning for predicting pathological complete response in patients with locally advanced rectal cancer after neoadjuvant chemoradiotherapy. Sci Rep 10(1):12555. https://doi.org/10.1038/s41598-020-69345-9
Shin J, Seo N, Baek SE et al (2022) MRI radiomics model predicts pathologic complete response of rectal cancer following chemoradiotherapy. Radiology 303(2):351–358. https://doi.org/10.1148/radiol.211986
Delitto D, George TJ Jr, Loftus TJ et al (2018) Prognostic value of clinical vs pathologic stage in rectal cancer patients receiving neoadjuvant therapy. J Natl Cancer Inst 110(5):460–466. https://doi.org/10.1093/jnci/djx228
Martens MH, Maas M, Heijnen LA et al (2016) Long-term outcome of an organ preservation program after neoadjuvant treatment for rectal cancer. J Natl Cancer Inst 108(12). https://doi.org/10.1093/jnci/djw171
Petresc B, Lebovici A, Caraiani C, Feier DS, Graur F, Buruian MM (2020) Pre-treatment T2-WI based radiomics features for prediction of locally advanced rectal cancer non-response to neoadjuvant chemoradiotherapy: a preliminary study. Cancers (Basel) 12(7). https://doi.org/10.3390/cancers12071894
Zhou X, Yi Y, Liu Z et al (2019) Radiomics-based pretherapeutic prediction of non-response to neoadjuvant therapy in locally advanced rectal cancer. Ann Surg Oncol 26(6):1676–1684. https://doi.org/10.1245/s10434-019-07300-3
Liu Y, Zhang FJ, Zhao XX et al (2021) Development of a joint prediction model based on both the radiomics and clinical factors for predicting the tumor response to neoadjuvant chemoradiotherapy in patients with locally advanced rectal cancer. Cancer Manag Res 13:3235–3246. https://doi.org/10.2147/CMAR.S295317
Wan XB, Zhang Q, Chen M et al (2020) Prognostic value of interval between the initiation of neoadjuvant treatment to surgery for patients with locally advanced rectal cancer following neoadjuvant chemotherapy, radiotherapy and definitive surgery. Front Oncol 10:1280. https://doi.org/10.3389/fonc.2020.01280
Petrelli F, Trevisan F, Cabiddu M et al (2020) Total neoadjuvant therapy in rectal cancer: a systematic review and meta-analysis of treatment outcomes. Ann Surg 271(3):440–448. https://doi.org/10.1097/SLA.0000000000003471
Lefevre JH, Rousseau A, Svrcek M et al (2013) A multicentric randomized controlled trial on the impact of lengthening the interval between neoadjuvant radiochemotherapy and surgery on complete pathological response in rectal cancer (GRECCAR-6 trial): rationale and design. BMC Cancer 13:417
Xiaojie W, Guangliang C, Yiyi Z et al (2020) The impact of circumferential tumour location on the clinical outcome of rectal cancer patients managed with neoadjuvant chemoradiotherapy followed by total mesorectal excision. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2020.02.034
Khan MAS, Ang CW, Hakeem AR et al (2017) The impact of tumor distance from the anal verge on clinical management and outcomes in patients having a curative resection for rectal cancer. J Gastrointest Surg 21(12):2056–2065. https://doi.org/10.1007/s11605-017-3581-0
Yu SKT, Brown G, Tait DM (2012) Use of MRI-defined tumor distance from the anal verge to predict tumor response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. J Clin Oncol 30(4). https://doi.org/10.1200/jco.2012.30.4_suppl.573
Jwa E, Kim JH, Han S et al (2014) Nomogram to predict ypN status after chemoradiation in patients with locally advanced rectal cancer. Br J Cancer 111(2):249–254. https://doi.org/10.1038/bjc.2014.256
Vickers AJ, Cronin AM, Elkin EB, Gonen M (2008) Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inf Dec Making. https://doi.org/10.1186/1472-6947-8-53
Acknowledgements
The authors thank AJE for language editorial advice.
Funding
This study was supported by the Startup Fund for Scientific Research, Fujian Medical University (grant number: 2019QH1276); Natural Science Foundation of Fujian Province (2020J011030); Medical Science Research Foundation of Beijing Medical and Health Foundation (B20062DS); Fujian Provincial Health Technology Project (2020CXA025); Bethune Charitable Foundation (X-J-2018–004); and Joint Funds for the Innovation of Science and Technology, Fujian Province (2020Y9071).
Author information
Authors and Affiliations
Contributions
Protocol/project development: GW, YH, YG. Data collection or management: JY, ZT, HT, BL. Data analysis: GW, YF, KY, QZ, YY. Manuscript writing/editing: GW. Other: YH and YG contributed equally to this work as co-corresponding author. GW, ZZ, and JC contributed equally to this work and should be considered as co-first authors. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was all approved by the Ethics Committee of Zhangzhou Affiliated Hospital of Fujian Medical University and Fujian Medical University Union Hospital (2020LWB078).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, G., Zheng, Z., Chen, J. et al. A nomogram for predicting good response after neoadjuvant chemoradiotherapy for locally advanced rectal cancer: a retrospective, double-center, cohort study. Int J Colorectal Dis 37, 2157–2166 (2022). https://doi.org/10.1007/s00384-022-04247-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04247-y