Abstract
Purpose
Haemorrhoidal disease (HD) plagues one in every ten people, with a plethora of surgical treatment modalities, of which laser haemorrhoidoplasty (LHP) is a relatively novel option. This systematic review and meta-analysis objectively evaluated the efficacy, safety, and tolerability of LHP compared against conventional (Milligan-Morgan) open haemorrhoidectomy (CoH).
Method
A comprehensive search of MEDLINE, EMBASE, CENTRAL, and Google Scholar was conducted. Randomised controlled trials (RCTs) and comparative cohort studies (CCSs) which compared LHP against CoH were included, with postoperative pain as the primary outcome. Secondary outcomes included intraoperative characteristics, short- and moderate-term outcome, and complications.
Results
A total of 12 studies (6 RCTs and 6 CCSs), with a total of 1824 patients, were analysed. LHP resulted in reduced postoperative pain for the first day (mean difference of 2.07 visual analogue scale units), week, and month. The mean dosage and duration of postoperative analgesia use was similarly lower, with a mean difference of 4.88 mg (morphine) and 2.25 days, respectively. Crucially, recurrence was equivocal (HR: 0.72, CI: 0.21–2.40) at a mean follow-up duration of 8.58 ± 9.55 months. LHP resulted in lower blood loss and was 12.74 min shorter on average. LHP’s postoperative recovery time was 9.03 days less with equivalent or decreased risk of most short- and moderate-term complications except anal thrombosis.
Conclusion
Our study suggests that LHP is more tolerable than CoH, providing patients with superior postoperative quality of life at equivalent moderate-term efficacy. These findings contribute to improved understanding of LHP and its potential at enhancing the quality of HD care.
Similar content being viewed by others
Introduction
HD is widely prevalent, plaguing up to 11% of the population [1,2,3]. The disease is defined by the abnormal dilatation and distortion of vasculature with subsequent connective tissue destruction within the anal cushion [4]. The aetiopathogenetic theory concerning HD is multifactorial and complex; factors contributing to its pathogenesis are manifold. It is mostly thought to arise from vascular tone dysregulation and vascular hyperplasia, contributed by elevated intraabdominal pressure and increased inflow of the superior rectal artery, ultimately causing dilatation of the haemorrhoidal plexus. Whilst benign, it causes marked discomfort, anxiety, and distress [5, 6]. Management depends on patient factors and grading; [5, 7] surgery is usually indicated after failure of conservative measures or higher grades (III and IV), classified by grading scales such as the Banov, Goligher, or BPRST classification [8,9,10].
Conventional open haemorrhoidectomy (CoH), initially described by Milligan-Morgan, is still regarded by literature in the modern era as the current gold standard surgical treatment [11, 12]. It is adopted globally and provides low recurrence, where haemorrhoids are excised with a scalpel [13]. Unfortunately, it is associated with significant postoperative pain and risk of postoperative complications [14]. Alternative operations such as the Ferguson closed haemorrhoidectomy, rubber-band ligation, and stapled haemorrhoidopexy were subsequently developed in efforts to mitigate said complications associated with CoH [15,16,17,18,19] but they were found to be compromised by pelvic sepsis, postoperative bleeding, and higher recurrence [20,21,22].
Non-excisional laser haemorrhoidoplasty (LHP) is a relatively novel minimally invasive modality, comprising of laser probe introduced through a small incision at the ano-cutaneous junction and anodermis into the haemorrhoid [23]. Radial energy at a wavelength of 980 to 1470 nm is deployed from the laser diode into the haemorrhoid cushion. Thermal energy causes closure of the haemorrhoidal plexus by venous thrombosis and obliteration of downstream haemorrhoidal cushions, with adherence of the rectal mucosal and submucosal layers to the underlying muscular layer whilst avoiding injury to the inner lining of the anal canal. This initiates fibrosis and tissue remodelling, causing volume reduction and eventual obliteration of the haemorrhoidal tissue [24,25,26,27]. An anorectal mucopexy can also be performed in the same setting with absorbable sutures to hitch up any remaining prolapse after the laser coagulation.
LHP and CoH are conducted under general or spinal anaesthesia, typically in ambulatory surgical settings, with oral analgesia for postoperative pain management. Previous studies have demonstrated reduced postoperative pain and risk of bleeding post-LHP, [27,28,29,30,31] recommending it for grade II and III HD with satisfactory long-term outcomes compared to CoH [24, 32]. Consequently, this study was conducted to evaluate the efficacy, safety, and tolerability of LHP compared against the established standard surgical modality that is CoH. This systematic review identified all existing randomised controlled trials (RCTs) and prospective comparative cohort studies (CCSs) and conducted a pairwise meta-analysis primarily to compare postoperative pain, with secondary objectives, including efficacy, clinical outcomes, and complication rates.
Materials and methods
Search strategy
A systematic literature review was conducted for all RCTs and CCSs comparing LHP against CoH in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [33]. Articles published in MEDLINE/Pubmed, Embase, and Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library were identified using search terms ‘Haemorrhoid’ (MeSH term), ‘Laser’, ‘Open’, ‘Milligan-Morgan’, ‘Conventional’, ‘Excisional’, ‘Haemorrhoidectomy’ (MeSH term), and ‘Clinical Trial’ (MeSH term). The top 100 most relevant results from Google Scholar were screened for each search string, in concordance with recommendations as an adjunctive database [34,35,36]. The references of shortlisted articles were searched. The last search date was 27th June 2021. The study protocol was registered in PROSPERO, the international prospective register of systematic reviews, on 31st July 2021 (CRD42021271029), with no post-registration amendments.
Inclusion and exclusion criteria
Original RCTs and CCSs comparing LHP against CoH were considered for this meta-analysis. Studies that compared LHP to other modalities were included if a comparison was made with CoH. No restrictions were made based on publication year or article language. All other study types were excluded.
Outcomes of interest
Data from individual studies were tabulated, including study design, demographical, and clinical parameters of patients, HD grade according to the Banov grading scale, and procedural details. Table 1 summarises the characteristics of included studies. The primary and secondary outcomes of this study were defined based on the repeatedly reported disadvantages of postoperative pain and complications and the advantage of low disease recurrence associated with CoH, to objectively assess and compare LHP against it.
The primary outcome assessed was postoperative pain, measured with the visual analogue scale (VAS) on days 1, 7, and 1 month after surgery, as all included studies reported according to this timeline to provide common timepoints of comparison. Postoperative pain was also measured indirectly through analgesia dose, duration of usage, and its post-discharge usage. Secondary outcomes included intraoperative characteristics, postoperative short- and moderate-term outcome, and complications. Postoperative short-term outcomes included were duration of hospitalisation and recovery time, defined as the time required to return to work or normal activity. Short-term complications included acute urinary retention (ARU), significant postoperative bleeding, reoperation, early recurrence, anal thrombosis, and acute anal discharge. Moderate-term outcomes included recurrence and assessment of postoperative quality of life (QoL). Recurrence was defined as recurrent internal or prolapsed haemorrhoids at the studies’ maximum follow-up period. Postoperative QoL was partly assessed by standardised questionnaires. Moderate-term complications included anal stenosis, bowel incontinence, and perianal skin tags.
Data extraction and synthesis
Relevant studies were identified by two authors through title and abstract screening. Further selection was based on full text. Any discrepancy was resolved by the senior author after discussion. Aforementioned data parameters were collected independently through a predetermined standardised data extraction form. Risk of bias assessment was performed using the revised Cochrane risk-of-bias tool for randomised trials (RoB 2) for RCTs and the risk of bias in non-randomised studies of interventions (ROBINS-I) for CCSs independently [37, 38].
Statistical analysis
Data were presented as mean with standard deviation, and frequencies as appropriate. Comparison between patients who underwent LHP (LHP group) and CoH (CoH group) were performed using chi-square test for categorical outcomes. A confidence level of p < 0.05 was considered statistically significant.
For each outcome, forest plots were rendered to include all applicable studies. Begg’s funnel plot was drawn for postoperative day 1 pain to assess publication bias [39] with Egger’s regression test. The presence of heterogeneity was assessed using the I2 index. The fixed-effects model was utilised for plots with I2 index less than 70% and the random-effects model for those more than 70% [40]. For binary data, a binomial model was used for the analysis, and the hazards ratio (HR) was calculated. The mean difference (MD), confidence interval (CI), and p-value were calculated for continuous outcomes [41].
All analyses were performed using the Review Manager (RevMan) computer program (version 5.4. Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration, 2020), GraphPad Prism v9 (GraphPad Software, La Jolla California, USA), Comprehensive Meta-Analysis Version 2 (Engelwood, NJ, Biostat; 2005), Risk-of-bias VISualization (robvis): An R package, and Shiny web app for visualising risk-of-bias assessments [42].
Results
Eligible studies
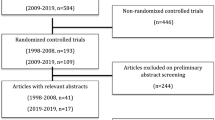
The initial search revealed a total of 7844 studies, of which 2756 were duplicates and 5088 were original studies. Non-relevant articles were excluded based on title and abstract screening, resulting in 32 studies. After examination by full text, 20 studies were excluded, leaving 12 studies (Fig. 1), of which 6 (50%) were RCTs with 419 (23%) total patients, and 6 (50%) studies were non-randomised, with 1405 (77%) total patients. The total cohort from all included studies was 1824 patients. The mean duration of follow-up was 8.58 ± 9.55 months. Sample sizes for individual studies ranged from 25 to 1000 patients (Table 1).
Demographic characteristics
The mean patient age ranged from 34.7 to 47.0 years for the LHP group and 33.7 to 49.0 years for the CoH group. With the exclusion of data from Plapler et al. [43] as gender was not reported, a male preponderance of 65.3% (n = 1174/1799) was observed in the total cohort. LHP group had 65.0% males (n = 584/899) and CoH group had 66.1% males (n = 588/900), with no statistical difference between them (p = 0.87). With the exclusion of data from Nazari et al. as grade breakdown was not specified, [44] most patients had Banov grade II or III haemorrhoids (97.6%, n = 1722/1765), with none having grade I haemorrhoidal disease (Table 2). The most common indications for surgery were bleeding (76.1%, n = 350/460), pain (37.4%, n = 172/460), and itching (17.4%, n = 80/460). The CoH group had a higher proportion of patients presenting with itching (p = 0.02).
Methodological quality of included studies
The RoB 2 and ROBINS-I revealed all six RCTs of ‘low risk’ and all six CCSs to be of ‘moderate risk,’ respectively. Egger’s test confirmed no significant publication bias: t = 1.69 (95% CI = − 31.5 to 7.9; p = 0.17).
Postoperative pain and analgesia
A total of 6 studies reported pain through the VAS on postoperative day 1 with 404 patients. The LHP group had significantly reduced pain compared to the CoH group with a mean difference of 2.07 (CI: 0.61–3.53, p = 0.005) units (Fig. 2). Pain at postoperative week 1 (Fig. 3) and month 1 (Fig. 4) demonstrated congruent findings, with a mean difference of 3.34 (CI: 1.10–5.57, p = 0.003) units and 0.52 (CI: 0.31–0.73, p < 0.0001) units of 3 and 2 studies (n = 205 and n = 125), respectively.
There was a reduction in the mean dosage of analgesia used postoperatively in the LHP group compared to the CoH group, with a mean difference of 4.88 mg (CI: 4.31–5.45, p < 0.0001) of morphine, reported by 4 studies (n = 279) (Fig. 5). Similarly, 2 studies (n = 140) observed a shorter duration of post-discharge use of oral analgesia with a mean difference of 2.25 days (CI: 0.83–3.67, p = 0.002) favouring the LHP group. A total of 2 studies (n = 120) demonstrated no significant difference in the number of patients who used post-discharge oral analgesia.
Intraoperative characteristics
A total of 9 studies (n = 719) reported the mean duration of surgery, where LHP was shorter than CoH, with a mean difference of 12.74 min (CI: 10.05–15.43, p < 0.0001). Additionally, the pooled estimate from 4 studies (n = 279) demonstrated that LHP resulted in less intraoperative blood loss, a mean difference of 16.43 ml (CI: 9.05–23.82, p < 0.0001).
Short-term outcome and complications
The short-term outcome was overall better after LHP. 4 studies (n = 320) described the mean duration of hospitalisation, which demonstrated no significant difference but tended to favour LHP with a mean difference of 0.45 days (CI: − 0.14–1.03, p = 0.13). A total of 4 studies (n = 440) revealed a shorter mean recovery time after discharge in the LHP group, with a mean difference of 9.03 days (CI: 1.87–16.18, p = 0.01).
From the analysis of 7 studies (n = 1540), LHP demonstrated a significantly lower risk ratio (RR) of significant postoperative bleeding at 0.22 (CI: 0.14–0.36, p < 0.0001). Similarly, though not significant, 2 studies (n = 160) demonstrated that LHP patients were less likely to have anal discharge with a HR of 0.13 (CI: 0.02–0.98, p = 0.05). The pooled estimate from 6 studies (n = 1359) demonstrated no significant difference in the RR of developing ARU; however, it tended to favour LHP at 0.23 (CI: 0.05–1.15, p = 0.07). On the other hand, there was a significantly elevated risk of developing acute thrombosis after LHP at RR of 5.50 (CI: 1.24–24.41, p = 0.02) through the pooled estimate of 4 studies (n = 279).
Moderate-term outcome and complications
Crucially, there was no significant difference between the rate of recurrence between the two groups from the pooled estimate of 7 studies (n = 1379), with a HR of 0.72 (CI: 0.21–2.40, p = 0.59), which tended to favour LHP (Fig. 6). Two studies utilised standardised patient questionnaires including the Wexner incontinence score, 36-item Short Form Health Survey (SF-36), and Faecal Incontinence Quality of Life (FIQOL). Poskus et al. reported no significant difference in the Wexner incontinence score and FIQOL between their LHP and CoH cohorts [45]. The SF-36, however, favoured CoH for the evaluation of General Health; while other components of the SF-36 were equivocal. However, LHP was evaluated as the best operation by patients. Shabahang et al. [46] result also favoured LHP at 6 months post-operation, where patients’ QoL was significantly better in their LHP cohort for all domains except for physical functioning.
Moderate-term complication rates were overall lower post-LHP, with a HR of 0.07 (CI: 0.02–0.31, p = 0.0004) for developing anal stenosis for patients undergoing LHP compared to CoH through the pooled estimate of 4 studies (n = 1240). Other moderate-term complications were not widely reported; one study described the incidence of anal stricture, with one patient from their CoH cohort and none after LHP. Two studies reported 8 total patients developing incontinence after CoH whilst all patients retained continence after LHP.
Discussion
LHP is relatively novel and has previous evidence demonstrating good efficacy and tolerability. Consequently, a pair-wise meta-analysis comparing LHP against CoH was conducted as the authors deemed the direct comparison against the established gold standard was the most appropriate for the objective evaluation of LHP. Apart from pre-operative itching, the two groups had congruent baseline characteristics. All haemorrhoidal disease grades were included as only 2.4% of the cohort presented with grade IV. Therefore, whilst its more severe symptomology may interfere with outcomes such as pain, the small percentage bears minimal impact upon the meta-analysis. A deliberate choice to forgo meta-regression was made to reflect how both surgeries perform in real-world settings, where multiple confounders affect the patient’s recovery and postoperative pain, and interpretation of isolated post-regression data may not accurately reflect practical patient care. Given the paucity of literature comparing long-term (> 1 year) recurrence rates after LHP and CoH and clinical significance of postoperative pain, postoperative pain was chosen as the primary outcome.
Pain and quality of life
In the current study, LHP was found to have resulted in significantly lower postoperative pain compared to CoH in the immediate period up to the first postoperative month, where the highest limitation in function and QoL occurs. Moreover, there was overall reduced analgesia use post-LHP compared to CoH, with reduced mean dosage and shorter duration of post-discharge oral analgesia use. Our findings are consistent with existing literature, where reduced pain is the greatest benefit of LHP [14, 32]. Importantly, pain is not limited to discomfort, but its effects expand into a myriad of sequelae associated with increased morbidity and mortality [47, 48].
Patients who underwent LHP experienced better short-term postoperative QoL, evidenced by quicker recovery and qualitative evaluation. However, it is challenging to ascertain the exact difference in recovery due to inter-study postoperative recovery time definition variation. Taken in context with decreased postoperative pain and risk of short-term complications, our findings suggest that LHP is superior in the short term.
Efficacy and safety profile of LHP
A major determinant of CoH as the standard of care is its low postoperative recurrence. Crucially, there was no significant difference between recurrence of LHP and CoH in the moderate term. Alternative surgeries such as stapled haemorrhoidectomy and Doppler-guided transanal haemorrhoid artery ligation (HAL) had higher rates of recurrence than CoH [14, 49,50,51]. Therefore, whilst several of these options provided similar benefits to LHP over CoH, patients had to weigh these advantages against elevated recurrence risk. Unsurprisingly, our pooled mean follow-up duration was relatively short at 8.58 ± 9.55 months, as HD patients are not followed-up beyond a year due to the quick postoperative healing time [22]. While a sub-year follow-up length is not ideal for assessing long-term outcomes, the clinical benefit of a long-term review is outweighed by unnecessary consumption of healthcare resources. Therefore, our findings remain an adequate and realistic reflection of the postoperative recurrence seen in routine clinical practice.
For providers, LHP provided reduced operative duration and intraoperative blood loss with no significant difference in the hospitalisation duration. From the patients’ perspective, risks of developing short-term complications after LHP, except acute thrombosis, which is expected considering LHP induces thrombosis, were either equivalent to or lower than CoH. Whilst not significant (p = 0.07), CoH had higher rates of ARU, which may predispose to further complications, including delirium, which burdens the patient-caregiver complex [52]. The risks of developing moderate-term complications were similarly lower post-LHP, though the studies did not extensively describe these likely due to the low risk inherent in these minor procedures.
Comparison of LHP against other modalities
Postoperative pain and postoperative complications are the most concerning disadvantages of CoH and closed (Ferguson) haemorrhoidectomy [50, 53, 54]. Akin to LHP, alternative modalities including LigaSure, harmonic scalpel haemorrhoidectomy, stapled haemorhoidopexy, and HAL have better intraoperative and postoperative profiles compared to CoH and closed haemorrhoidectomy. Most importantly, they are similarly less painful for the patients. Crucially, these advantages were accompanied by the major issue of higher recurrence rates [14, 22, 49,50,51]. Therefore, given equivalent recurrence rate between LHP and CoH, evidenced by consistent results from independent institutions across 9 countries, LHP may potentially be superior to CoH by providing greater tolerability whilst maintaining CoH’s standard-defining efficacy in the moderate term [44,45,46, 54,55,56,57,58,59,60,61,62].
A noteworthy disadvantage of LHP is cost efficacy. Due to the technology’s novelty, the cost of the laser diode and generator are greater than consumables used in simpler procedures such as CoH, closed haemorrhoidectomy or HAL, which has been touted as a quick and affordable alternative [63, 64]. Currently, there is limited literature analysing LHP’s cost-effectiveness to support its widespread use globally. Consequently, further cost-analyses need to be conducted considering the interest of different stakeholders, including the patient, institutions, and insurance companies. The effects of variations of healthcare payment structures and distinct economical capacity of different countries on the cost-analysis of LHP should be recognised. Therefore, LHP’s uptake should be considered within national contexts.
It should be emphasised that every individual modality in the modern surgical arsenal for haemorrhoid management has its own unique surgical profile accompanied by its respective benefits and risks, the details of which lie beyond the scope of this review. Ultimately, despite the presence of CoH as the standard of care, there exist a plethora of favourable techniques widely available across institutions. In the fraternity’s bid for personalised surgical practice, an open discussion between patients and physicians is imperative to guide individualised care, catering to each patient’s unique goals and lifestyle.
Strengths and limitations
The strength of this study was its ability to overcome inter-study variation and mitigate the effect of practical confounding factors, given the general paucity of studies comparing LHP and CoH directly. Our study fills an essential gap in the literature, providing a high level of evidence for a quick, effective, and tolerable procedure to treat a remarkably prevalent condition.
However, our study has limitations which should be considered during interpretation. The principal limitation was the inclusion of nonrandomised comparative cohort studies. Whilst we acknowledged that observational cohort studies are subjected to selection and observational bias, ultimately affecting the study’s evidence level, their inclusion was maintained to improve external validity as the larger sample size would provide a more generalisable assessment of our findings, mitigating the compromise on the study’s validity had CCSs been excluded. It should also be noted that the exact laser probe used differed across studies, though the procedure is broadly similar. Biolitec© provides the laser equipment for one RCT (Poskus et al.), though the company was not involved in the study design and data analysis [45]. We acknowledge that the higher cost of LHP’s equipment may be a bias in the included studies; however, as the methodological quality of the included studies was found to be adequate, its impact on the final pooled analysis may be minimal.
Most of our included studies hail from Eastern European and Middle Eastern nations, owing to the paucity of available studies from larger territories such as North America or East Asia. It should be noted that they had limited follow-up periods, where larger studies such as the eTHoS trial measure symptom recurrence up to 24 months post-intervention, therefore disallowing the evaluation of long-term post-procedure recurrence rate of LHP [65, 66]. Nevertheless, all RCTs and CCSs on the subject were included, with the evaluation of moderate-term efficacy. Our findings should encourage Western institutions to increase their attention to LHP. Additionally, the results were tabulated from a limited sample size of twelve studies. However, the funnel plot complemented by the results of Egger’s test pointed to low possibility of publication bias.
Conclusion
This systematic review revealed a paucity of well-conducted, large RCTs comparing CoH and LHP that measure symptom recurrence as a primary outcome and a minimum follow-up period of 24 months. Our findings suggest that LHP provides benefits firstly to patients through reduced intraoperative blood loss, substantial reduction of postoperative pain up till the first postoperative month, reduced risk of most postoperative short- and moderate-term complications and improved postoperative QoL; and secondly to providers by reducing operative time. Crucially, the moderate-term recurrence rate is equivalent to CoH. Our findings contribute to the pool of evolving data regarding contemporary surgical treatments for HD. In addition, cost-utility data in a robust health economics study is needed.
References
Johanson JF, Sonnenberg A (1990) The prevalence of hemorrhoids and chronic constipation an epidemiologic study. Gastroentrrology 98
Loder PB, Kamm MA, Nicholls RJ, Phillips RKS (1994) Haemorrhoids: pathology, pathophysiology and aetiology. Br J Surg 81:946–54. Available from: https://pubmed.ncbi.nlm.nih.gov/7922085/
Riss S, Weiser FA, Schwameis K, Riss T, Mittlböck M, Steiner G et al (2012) The prevalence of hemorrhoids in adults. Int J Colorectal Dis 27(2):215–20. Available from: https://doi.org/10.1007/s00384-011-1316-3
Lohsiriwat V (2012) Hemorrhoids: from basic pathophysiology to clinical management Varut Lohsiriwat. World J Gastroenterol 18(17):2009–2017
Lohsiriwat V (2021) Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol. Baishideng Publishing Group Inc; Vol. 18 p. 2009–17. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3342598/
Koh FH, Foo FJ, Ho L, Sivarajah SS, Tan WJ, Chew MH (2020) Study protocol for the use of conventional open haemorrhoidectomy versus laser haemorrhoidoplasty in the treatment of symptomatic haemorrhoids: a randomized controlled trial. Euro Surg Res 61(6):201–8. Available from: https://doi.org/10.1159/000513844
van Tol RR, Kleijnen J, Watson AJM, Jongen J, Altomare DF, Qvist N et al (2020) European Society of ColoProctology: guideline for haemorrhoidal disease. Colorectal Dis 22(6):650–662
Banov L, Knoepp LF, Erdman LH, Alia RT (1985) Management of hemorrhoidal disease. J S C Med Assoc 81(7):398—401. Available from: http://europepmc.org/abstract/MED/3861909
Júnior CWS, de Almeida Obregon C, da Silva e Sousa Júnior AH, Sobrado LF, Nahas SC, Cecconello I (2020) A new classification for hemorrhoidal disease: the creation of the “BPRST” staging and its application in clinical practice. Annal Coloproctol 36(4):249–55
Dekker L, Han-Geurts IJM, Grossi U, Gallo G, Veldkamp R (2022) Is the Goligher classification a valid tool in clinical practice and research for hemorrhoidal disease? Tech Coloproctol 26(5):387–392
Gallo G, Luc AR, Tiesi V, Trompetto M (2021) Sign of the times: the Milligan–Morgan era. Vol. 25, Techniques in Coloproctology. Springer Science and Business Media Deutschland GmbH p. 1327
Bhatti MI, Sajid MS, Baig MK (2016) Milligan-Morgan (Open) versus ferguson haemorrhoidectomy (closed): a systematic review and meta-analysis of published randomized, controlled trials. World J Surg 40:1509–19. Springer New York LLC
Milligan ETC, Melb OBE, Eng FRCS, Morgan CN, Jones LE, Lond MB Addresses and original articles surgical anatomy of the anal canal, and the operative treatment of HÆ Morrhoids Mark’s Hospital For Diseases of the Rectum, London
Simillis C, Thoukididou SN, Slesser AAP, Rasheed S, Tan E, Tekkis PP (2015) Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg 102(13):1603–18.
Faucheron JL, Poncet G, Voirin D, Badic B, Gangner Y (2011) Doppler-guided hemorrhoidal artery ligation and rectoanal repair (HAL-RAR) for the treatment of grade IV hemorrhoids: long-term results in 100 consecutive patients. In: Diseases of the Colon and Rectum [Internet]. Dis Colon Rectum p. 226–31. Available from: https://pubmed.ncbi.nlm.nih.gov/21228673/
Arroyo A, Pørez F, Miranda E, Serrano P, Candela F, Lacueva J et al (2004) Open versus closed day-case haemorrhoidectomy: is there any difference? Int J Colorectal Dis 19:370–373
Hoyuela C, Carvajal F, Juvany M, Troyano D, Trias M, Martrat A et al (2016) HAL-RAR (Doppler guided haemorrhoid artery ligation with recto-anal repair) is a safe and effective procedure for haemorrhoids. Results of a prospective study after two-years follow-up. Int J Surg 28:39–44
Pernice LM (2002) Stapled anopexy and stapled hemorrhoidectomy: two opposite concepts and procedures (multiple letters). Dis Colon Rectum 45:571–2. Available from: https://pubmed.ncbi.nlm.nih.gov/12006945/
Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S et al (2008) Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation. Health Technol Assess 12(8). Available from: https://pubmed.ncbi.nlm.nih.gov/18373905/
van Tol RR, Bruijnen MPA, Melenhorst J, van Kuijk SMJ, Stassen LPS, Breukink SO (2018) A national evaluation of the management practices of hemorrhoidal disease in the Netherlands. Int J Colorectal Dis 33(5):577–88. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5899108/
Sim HL, Tan KY, Poon PL, Cheng A, Mak K (2009) Life-threatening perineal sepsis after rubber band ligation of haemorrhoids. Tech Coloproctol 13(2):161–164
Bouchard D, Abramowitz L, Castinel A, Suduca JM, Staumont G, Soudan D et al (2013) One-year outcome of haemorrhoidectomy: a prospective multicentre French study. Colorectal Dis 15(6):719–726
Lim SY, Rajandram R, Roslani AC (2022) Comparison of post-operative bleeding incidence in laser hemorrhoidoplasty with and without hemorrhoidal artery ligation: a double-blinded randomized controlled trial. Available from: https://doi.org/10.21203/rs.3.rs-1095466/v1
Longchamp G, Liot E, Meyer J, Toso C, Buchs NC, Ris F (2021) Non-excisional laser therapies for hemorrhoidal disease: a systematic review of the literature. Available from: https://doi.org/10.1007/s10103-020-03142-8
Salfi R (2009) A new technique for ambulatory hemorrhoidal treatment: doppler-guided laser photocoagulation of hemorrhoidal arteries. Coloproctology 31(2):99–103. Available from: https://doi.org/10.1007/s00053-009-0009-7
Plapler H (2008) A new method for hemorrhoid surgery: experimental model of diode laser application in monkeys. Photomed Laser Surg 26(2):143–6. Available from: https://pubmed.ncbi.nlm.nih.gov/18341413/
Faes S, Pratsinis M, Hasler-Gehrer S, Keerl A, Nocito A (2019) Short- and long-term outcomes of laser haemorrhoidoplasty for grade II–III haemorrhoidal disease. Colorectal Dis 21(6):689–696
Crea N, Pata G, Lippa M, Chiesa D, Gregorini ME, Gandolfi P (2014) Hemorrhoidal laser procedure: short- and long-term results from a prospective study. Am J Surg 208(1):21–5. Available from: https://pubmed.ncbi.nlm.nih.gov/24507943/
de Nardi P, Tamburini AM, Gazzetta PG, Lemma M, Pascariello A, Asteria CR (2016) Hemorrhoid laser procedure for second- and third-degree hemorrhoids: results from a multicenter prospective study. Tech Coloproctol 20(7):455–459
Maloku H, Gashi Z, Lazovic R, Islami H, Juniku-Shkololli A (2014) Laser hemorrhoidoplasty procedure vs open surgical hemorrhoidectomy: a trial comparing 2 treatments for hemorrhoids of third and fourth degree. Acta Informatica Med 22(6):365–7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4315650/
Naderan M, Shoar S, Nazari M, Elsayed A, Mahmoodzadeh H, Khorgami Z (2017) A randomized controlled trial comparing laser intra-hemorrhoidal coagulation and Milligan–Morgan Hemorrhoidectomy. J Invest Surg 30(5):325–31. Available from: https://doi.org/10.1080/08941939.2016.1248304
Lakmal K, Basnayake O, Jayarajah U, Samarasekera DN (2021) Clinical outcomes and effectiveness of laser treatment for hemorrhoids: a systematic review. World Journal of Surgery. Springer Science and Business Media Deutschland GmbH
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714672/
Haddaway NR, Collins AM, Coughlin D, Kirk S (2015) The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS ONE 17;10(9)
Gusenbauer M, Haddaway NR (2020) Which academic search systems are suitable for systematic reviews or meta-analyses? Evaluating retrieval qualities of Google Scholar, PubMed, and 26 other resources. Res Synthesis Methods 11(2):181–217
Shultz M (2007) Comparing test searches in PubMed and Google Scholar. J Med Libr Assoc 95(4):442–445
Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) (2019)
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Online) 355
Joober R, Schmitz N, Annable L, Boksa P, -Douglas B (2012) Publication bias: what are the challenges and can they be overcome? J Psychiatry Neurosci 37(3)
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ : Br Med J 327(7414):557. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC192859/
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al (2021) Cochrane Handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane. Available from: www.training.cochrane.org/handbook
McGuinness LA, Higgins JPT (2021) Risk-of-bias visualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. In: Research Synthesis Methods. John Wiley and Sons Ltd. p. 55–61
Plapler H, Hage R, Duarte J, Lopes N, Masson I, Cazarini C et al (2009) A new method for hemorrhoid surgery: intrahemorrhoidal diode laser, Does It Work? Photomed Laser Surg 27(5):819–23. Available from: https://doi.org/10.1089/pho.2008.2368
Nazari MS, Hedayati MK (2015) Comparison of Intrahemorrhoidal Coagulation with 980 nanometer diode laser and Milligan Morgan hemorrhoidectomy: a randomized clinical trial. J Clin Res Govern
Poskus T, Danys D, Makunaite G, Mainelis A, Mikalauskas S, Poskus E et al (2020) Results of the double-blind randomized controlled trial comparing laser hemorrhoidoplasty with sutured mucopexy and excisional hemorrhoidectomy. Int J Colorectal Dis 35(3):481–490
Shabahang H, Maddah G, Mofidi A, Nooghabi MJ, Khaniki SH (2019) A randomized clinical trial of laser hemorrhoidoplasty vs milligan and morgan hemorrhoidectomy. World J Laparoscop Surg 12(2):59–63
van Boekel RLM, Warlé MC, Nielen RGC, Vissers KCP, van der Sande R, Bronkhorst EM et al (2019) Relationship between postoperative pain and overall 30-day complications in a broad surgical population: an observational study. Ann Surg 269(5):856–865
Ghoneim MM, O’Hara MW (2016) Depression and postoperative complications: an overview visceral and general surgery. BMC Surgery. BioMed Central Ltd 16
Giordano P, Gravante G, Sorge R (2009) Long-term outcomes of stapled hemorrhoidopexy vs conventional hemorrhoidectomy a meta-analysis of randomized controlled trials. Arch Surgery 144(3):266-272
Jayaraman S, Colquhoun PHD, Malthaner RA (2006) Stapled versus conventional surgery for hemorrhoids. Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd
Sajid MS, Parampalli U, Whitehouse P, Sains P, McFall MR, Baig MK (2012) A systematic review comparing transanal haemorrhoidal de-arterialisation to stapled haemorrhoidopexy in the management of haemorrhoidal disease. Techniq Coloproctol 16:1–8.
Oh ST, Park JY (2019) Postoperative delirium. Korean Soc Anesthesiol 72:4–12
Halverson A (2007) Hemorrhoids. Clin Colon Rectal Surg 20:77–85
Eskandaros M, Darwish A (2020) Comparative study between Milligan-Morgan hemorrhoidectomy, stapled hemorrhoidopexy, and laser hemorrhoidoplasty in patients with third degree hemorrhoids: a prospective study. Egyptian J Surg 39(2):352
Maloku H, Lazović R, Terziqi H (2019) Laser hemorrhoidoplasty versus Milligan-Morgan hemorrhoidectomy - short-term outcome. Vojnosanit Pregl 76(1):8–12
Mohammed AF, Ali D, Al-Sultani H, Majeed H, Janabi F (2019) A comparative study between laser hemorrhoidoplasty procedure and conventional hemorrhoidectomy. Pure Appl Sci
Mubarak Khan H, Sanjeevaiah Shankare Gowda V, Shamburao Ramesh B, Sandeep D (2021) Journal of clinical and investigative surgery a comparative evaluation of laser hemorrhoidoplasty versus open surgical hemorrhoidectomy treatment of grade III and IV hemorrhoids. A prospective observational study. J Clin Invest Surg 6(1):30–6. Available from: https://doi.org/10.25083/2559-5555
Hassan A, El-Shemy G (2021) Laser hemorrhoidoplasty versus open hemorrhoidectomy in Upper Egypt. Al-Azhar Int Med J
Maloku H, Gashi Z, Lazovic R, Islami H, Juniku-Shkololli A (2014) Laser hemorrhoidoplasty procedure vs open surgical hemorrhoidectomy: a trial comparing 2 treatments for hemorrhoids of third and fourth degree. Acta Informatica Medica 22(6):365–367
Alsisy A, Alkhateep Y, Salem I (2019) Comparative study between intrahemorrhoidal diode laser treatment and Milligan-Morgan hemorrhoidectomy. Menoufia Med J 32(2):560
Naderan M, Shoar S, Nazari M, Elsayed A, Mahmoodzadeh H, Khorgami Z (2017) A randomized controlled trial comparing laser intra-hemorrhoidal coagulation and Milligan-Morgan hemorrhoidectomy. J Invest Surg 30(5):325–331
Lio Plapler H, Hage R, Duarte J, Lopes N, Masson I, Udio Cazarini C et al (2009) A new method for hemorrhoid surgery: intrahemorrhoidal diode laser, does it work? Available from: www.liebertpub.com
Emile SH, Elfeki H, Sakr A, Shalaby M (2019) Transanal hemorrhoidal dearterialization (THD) versus stapled hemorrhoidopexy (SH) in treatment of internal hemorrhoids: a systematic review and meta-analysis of randomized clinical trials. Int J Colorectal Dis Vol. 34. Springer Verlag
Abudeeb H, Ugwu A, Darabnia J, Hammad A, Khan K, Maung M et al (2017) THD and mucopexy: efficacy and controversy. Annal Med Surg 1(21):89–92
Watson AJM, Hudson J, Wood J, Kilonzo M, Brown SR, McDonald A et al (2016) Comparison of stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease (eTHoS): a pragmatic, multicentre, randomised controlled trial. The Lancet 388(10058):2375–2385
Brown S, Tiernan J, Biggs K, Hind D, Shephard N, Bradburn M et al (2016) The HubBle trial: Haemorrhoidal artery ligation (HAL) versus rubber band ligation (RBL) for symptomatic second- and third-degree haemorrhoids: a multicentre randomized controlled trial and health-economic evaluation. Health Technol Assess 20(88):1–180
Funding
VZZ Tan received the SingHealth Medical Student Talent Development Award (SMSTDA)—Project from SingHealth, Singapore, which provided funding purely for the purchase of analysis software which were used for this study (Grant Reference SMSTDA-VAREN). For the remaining authors, none were declared.
Author information
Authors and Affiliations
Contributions
VT conceptualised and designed the study, participated in data collection, data extraction, data analysis, statistical analysis, and writing of the manuscript. EP conceptualised and designed the study, participated in data collection, data extraction, data analysis, statistical analysis, and writing of the manuscript. SS revised and approved the final manuscript. WT revised and approved the final manuscript. LH revised and approved the final manuscript. JN revised and approved the final manuscript. CC revised and approved the final manuscript. DA revised and approved the final manuscript. FM revised and approved the final manuscript. FF revised and approved the final manuscript. FK acted as the senior author, conceptualised and designed the study, reviewed the analysed data, reviewed and revised the manuscript, and approved the final manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval
In concordance with the prevailing law in Singapore, this study did not require an institutional review board.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tan, V.Z.Z., Peck, Ew., Sivarajah, S.S. et al. Systematic review and meta-analysis of postoperative pain and symptoms control following laser haemorrhoidoplasty versus Milligan-Morgan haemorrhoidectomy for symptomatic haemorrhoids: a new standard. Int J Colorectal Dis 37, 1759–1771 (2022). https://doi.org/10.1007/s00384-022-04225-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04225-4