Abstract
Purpose
Computer-aided polyp detection (CADe) systems for colonoscopy are already presented to increase adenoma detection rate (ADR) in randomized clinical trials. Those commercially available closed systems often do not allow for data collection and algorithm optimization, for example regarding the usage of different endoscopy processors. Here, we present the first clinical experiences of a, for research purposes publicly available, CADe system.
Methods
We developed an end-to-end data acquisition and polyp detection system named EndoMind. Examiners of four centers utilizing four different endoscopy processors used EndoMind during their clinical routine. Detected polyps, ADR, time to first detection of a polyp (TFD), and system usability were evaluated (NCT05006092).
Results
During 41 colonoscopies, EndoMind detected 29 of 29 adenomas in 66 of 66 polyps resulting in an ADR of 41.5%. Median TFD was 130 ms (95%-CI, 80–200 ms) while maintaining a median false positive rate of 2.2% (95%-CI, 1.7–2.8%). The four participating centers rated the system using the System Usability Scale with a median of 96.3 (95%-CI, 70–100).
Conclusion
EndoMind’s ability to acquire data, detect polyps in real-time, and high usability score indicate substantial practical value for research and clinical practice. Still, clinical benefit, measured by ADR, has to be determined in a prospective randomized controlled trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Screening colonoscopies are highly effective at reducing the incidence of colorectal cancer (CRC). Previous studies revealed a decrease of 68% regarding CRC-related mortality by performing screening colonoscopies as most of these carcinomas develop over years following the adenoma-carcinoma sequence [1]. Adenoma detection rate (ADR) evolved to one of the most important colonoscopy quality parameters correlated to interval carcinoma rate [1]. As the research of artificial intelligence (AI) progressed, clinical applications were tested for viability [2]. A meta-analysis by Hassan et al. analyzed the current randomized studies regarding deep learning–based polyp detection in colonoscopy (CADe) [3]. They concluded that AI-assisted polyp detection increases the ADR, especially for small (< 5 mm), flat adenomas. Anyhow, only one of the five analyzed studies was performed in Europe [4] while the others are limited to an Asian study population [5,6,7,8]. Furthermore, three of the studies included mostly symptomatic patients [5,6,7]. Regarding generalizability, only one of the CADe systems [4] was evaluated with multiple processor types and only one study was multicentric [4]. Therefore, the authors concluded that more data for non-Asian populations is necessary. Furthermore, examiners focus on the center of the endoscopic image and CADe systems improve detection in the image’s periphery [9]. Lastly, to our knowledge there is no data regarding usability and acceptance of CADe systems in clinical practice.
In this study, we present the pilot phase results of our real-time CADe polyp detection system EndoMind and its framework applied in clinical practice. The proposed framework is an end-to-end solution capable of data acquisition for the training of neural networks as well as clinical application of the AI. The AI was developed utilizing multicentric data acquired by the EndoMind framework itself using different endoscopy processor types. Therefore, it is capable of fast development, evaluation, and real-time application of AI-based video analysis. Lastly, we analyzed the physicians’ feedback to evaluate the potential hardships of migrating this powerful tool for polyp detection to clinical application.
Methods
Development of EndoMind hardware and software
EndoMind hardware utilizes regular off-the-shelf components including a high-performance computer and a video grabber card that provide compatibility with a multitude of available endoscopy processors. The components were determined based on optimal requirements for a real-time AI application system while maintaining affordable pricing to make this freely available system easy to implement for clinicians in the future. Supplementary Table 1 lists the hardware composition resulting in a total price of about 2,880 €.
The CADe system, including software and hardware, was developed to perform data acquisition of the video signal and the exact location of the AI predictions as well as real-time polyp detection simultaneously. The software is able to handle a wide range of endoscopy processor video signals, including analog to ultra-high definition standards. The video signal is processed to single images called frames independently of the input source. Those are then forwarded to three processing pipelines (Display, AI, and Recording) in parallel to fit the requirements for real-time application (Supplementary Fig. 1). This parallelization minimizes video delay as only the predictions are visualized on a later frame. Furthermore, the AI predicts only every second to third frame and extrapolates the results to the remaining frames. The AI is based on a convolutional neural network that was trained with 506,338 manually annotated images from endoscopic examinations with and without visible polyps. The software’s detailed structure is explained in Supplementary Material. EndoMind software including a detailed installation handbook is freely available for research purposes (https://www.ukw.de/research/inexen/ai-applied-in-real-time/).
Participants
We retrospectively reviewed colonoscopy reports and corresponding videos of our randomized controlled trial’s pilot phase data. Here, examiners with at least 10 years of experience in performing colonoscopies were asked to evaluate EndoMind before starting the randomized study phase (NCT05006092). Only complete video recordings were included. The evaluated video recordings originate from four different endoscopy processors (Olympus CV-170 and CV-190 (Olympus Europa SE & Co. KG, Hamburg, Germany), Pentax i7000 (Pentax Europe GmbH, Hamburg, Germany), and Storz TC301 (Karl Storz SE & Co. KG, Tuttlingen, Germany)). Centers included three outpatient gastroenterological practices and one community-based hospital.
Data annotation
A physician (TJL) annotated each video from start to end and a board-certified gastroenterologist (AH) verified annotations. Sequences including polyps were labeled as such. Polyp size, morphology, pathological report if available, location and Boston bowel preparation scale (BBPS) were retrospectively identified. Polyps were categorized as proximal if located between caecum and the left flexure, otherwise as distal. Withdrawal time was determined as the time difference of the last anatomic landmark inspection (ileocecal valve, appendix, or ileum) and last image inside of the body [10]. Time spent on endoscopic interventions was manually annotated and subtracted from withdrawal time as well as all other evaluations. Each CADe prediction was labeled as true or false positive.
Survey
Examiners of the four centers were asked to participate in an online survey about the EndoMind usage (Supplementary Table 2). The survey consisted of the System Usability Scale (SUS) resulting in a total score of 0 to 100 points. Additional questions about the EndoMind performance were rated using a Likert scale from 1 (strongly disagree) to 5 (strongly agree) or percentage estimates.
Statistical analysis
Statistical analysis was performed using Python 3.10. Sensitivity was defined as the number of polyps detected in at least one frame divided by the number of all visible polyps. Time to first detection (TFD) was determined for each polyp as the visible time between polyp appearance and the first frame with correct CADe detection. For histology-based analyses, polyps without available histology due to not performed resection were excluded. Data was tested for normal distribution using SciPy’s normal test. For data with normal distribution, mean and standard deviation were calculated. For non-normal distributed data, median and its two-sided 95% confidence intervals (CI) were calculated using bootstrapping (n = 1000).
Ethical considerations
The study was approved by the local ethical committee responsible for each study center (Ethik-Kommission Landesärztekammer Baden-Württemberg (F-2021–047), Ethik-Kommission Landesärztekammer Hessen (2021–2531), and Ethik-Kommission der Landesärztekammer Rheinland-Pfalz (2021–15,955)). All procedures were in accordance with the Helsinki Declaration of 1964 and later versions. Signed informed consent from each patient was obtained prior to participation.
Results
Patient characteristics
Using EndoMind (Fig. 1), 41 examinations were recorded during the pilot phase of the study in four centers. Patient characteristics are presented in Table 1. Most examinations were performed for colorectal cancer screening or surveillance (63.4%). BBPS was rated as six or higher in 95.1% of the examinations. Characteristics of the participating examiners are presented in Supplementary Table 3.
CADe performance
In total, 66 polyps were identified in 41 colonoscopies. Figure 2 depicts representative images of EndoMind detections. Polyp characteristics and detection metrics are summarized in Table 2. Of the 37 histologically evaluated polyps, 29 were diagnosed as adenomatous resulting in an ADR of 41.5%. EndoMind detected 29 of 29 adenomas and 66 of 66 polyps. Overall, median TFD was as fast as 130 ms (95%-CI, 80–200 ms).
Manual annotation of all 1,544,063 individual images of which 74,422 (4.82%) contained a visible polyp, revealed an overall CADe accuracy of 95.3%. Median false positive detection rate per examination was 2.2% (95%-CI, 1.7–2.8%).
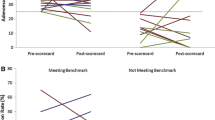
Usability survey
Examiners participating in the pilot phase rated the usability of EndoMind with a median SUS score of 96.3 (95%-CI, 70–100). The physicians subjectively stated that 89% (95%-CI, 79–94%) of the polyps were detected by our system. Of those polyps 46% (95%-CI, 21–61%) were subjectively detected by EndoMind before the examiner. Anyhow, users partially criticized false detections as distracting (median 3, 95%-CI, 2–3) and as a possible reason for a prolonged withdrawal time (median 2.5, 95%-CI, 2.0–5.0). Lastly, interventionists agreed that the EndoMind system would benefit patient care (median 4.5, 95%-CI, 3.0–5.0) and therefore would like to use it in their clinical routine (median 4.5, 95%-CI, 4.0–5.0).
Discussion
In this work, we present the freely available CADe system EndoMind. It incorporates recording of endoscopy videos with AI predictions. Additionally, it is capable of real-time polyp detection on a variety of endoscopy processors. We could demonstrate successful installation and use of our system in four non-research-focused centers. While previous studies included mostly symptomatic patients of Asiatic origin in a hospital setting [5,6,7, 11], 63.4% of the colonoscopies included in our pilot phase study were performed as screening or surveillance examinations. Furthermore, we could preliminarily validate high sensitivity (100% of polyps detected) and fast detection (median TFD 130 ms). While this preliminary data may not be directly compared to other studies, the ADR in our pilot phase study was 41.5%. A total of 29 out of 37 (78.4%) histologically evaluated polyps were diagnosed as adenoma which indicates high quality of the performed colonoscopies. Assessing the characteristics of the detected adenomas, we found a similar size distribution compared to previously published studies [4,5,6,7]. Other CAD systems report a false positive (FP) rate of 0.9 to 8% [12,13,14]. Assessment of false detections by EndoMind is located in the lower range with 2.2%. Qualitative screening of coherent false positive detections revealed mainly stool-covered areas, air bubbles, or pseudo-polyps generated by artifacts due to suction of the mucosa as the most common sources. As especially right-sided polyps are initially often covered by mucus, some of those FP detections may not be eliminated without severely affecting detection of these polyps in the early phase when they appear. Nevertheless, as a recent in depth analysis by Spadaccini et al. demonstrated, examiners can quickly disregard these FPs [15].
Our usability-focused survey involved only highly experienced examiners, mostly from outpatient treatment centers. We designed EndoMind to assist in screening colonoscopies; therefore, this group resembles the future target group. The participating physicians found EndoMind to be easy to use and maintain with a median SUS of 96.3 which exceeds the average of 69 [16]. Furthermore, they agreed that their clinical routine would benefit from the regular usage of EndoMind. However, the examiners also stated that false positive detections might increase their withdrawal time. Additionally, even correctly detected polyps might disturb the workflow if the physician has already identified it. Therefore, features to easily and even automatically deactivate the system should be implemented in future. While manual deactivation may be achieved by a foot switch or voice command, automatic deactivation based on the examination state seems also promising. For this, the most practical approaches include activation of the CADe system only after identification of the caecum and deactivation if an instrument is detected in the field of view. This would restrict the CADe detections to the withdrawal time and prevent disturbing activations during resections and biopsies.
Additionally, we evaluated the physician’s impressions of how many polyps were missed (11%), as well as how many polyps were detected by the system before the examiner (46%). The discrepancy between our determined sensitivity and the survey result may result from a different definition of detection: while frequently used metrics accept a polyp as detected if it is recognized at all, examiners might define a polyp, which is only detected after it is centered and focused on the image, as missed. As a more realistic measure, we therefore evaluated the TFD. Here, 89.4% of the polyps were detected in less than a second, which closely correlates with the examiners’ impression of the percentage of CADe-identified polyps.
While our results imply high clinical value of our freely available CADe system, absence of a control group in this early stage as well as the small sample size demands verification by a larger, randomized, controlled study. The aim of this study was therefore not to present how our system improves the ADR, but instead to demonstrate the application of this new CADe system in a clinical scenario involving multiple processor types and an evaluation of its performance on a frame-by-frame basis.
As our system is easy to use, and preliminary results indicate high practical value, we are confident that patient care would profit if systems like EndoMind are utilized in the daily routine. Furthermore, the implemented recording capabilities reduce the effort for continuously improving the system. By usage of rapid training iterations, our system enables for user- or patient group–specific AI fine-tuning as it is known from other applications like text to speech applications which improve their performance with increasing time of use. We hope that the EndoMind platform might contribute to improving endoscopy by continuously incorporating new AI features.
References
Corley DA, Levin TR, Doubeni CA (2014) Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 370:2541. https://doi.org/10.1056/NEJMc1405329
Liu P, Wang P, Glissen Brown JR et al (2020) The single-monitor trial: an embedded CADe system increased adenoma detection during colonoscopy: a prospective randomized study. Ther Adv Gastroenterol 13:1756284820979165. https://doi.org/10.1177/1756284820979165
Hassan C, Spadaccini M, Iannone A et al (2021) Performance of artificial intelligence in colonoscopy for adenoma and polyp detection: a systematic review and meta-analysis. Gastrointest Endosc 93:77-85.e6. https://doi.org/10.1016/j.gie.2020.06.059
Repici A, Badalamenti M, Maselli R et al (2020) Efficacy of real-time computer-aided detection of colorectal neoplasia in a randomized trial. Gastroenterology 159:512-520.e7. https://doi.org/10.1053/j.gastro.2020.04.062
Wang P, Liu X, Berzin TM et al (2020) Effect of a deep-learning computer-aided detection system on adenoma detection during colonoscopy (CADe-DB trial): a double-blind randomised study. Lancet Gastroenterol Hepatol 5:343–351. https://doi.org/10.1016/S2468-1253(19)30411-X
Wang P, Berzin TM, Glissen Brown JR et al (2019) Real-time automatic detection system increases colonoscopic polyp and adenoma detection rates: a prospective randomised controlled study. Gut 68:1813–1819. https://doi.org/10.1136/gutjnl-2018-317500
Liu W-N, Zhang Y-Y, Bian X-Q et al (2020) Study on detection rate of polyps and adenomas in artificial-intelligence-aided colonoscopy. Saudi J Gastroenterol Off J Saudi Gastroenterol Assoc 26:13–19. https://doi.org/10.4103/sjg.SJG_377_19
Su J-R, Li Z, Shao X-J et al (2020) Impact of a real-time automatic quality control system on colorectal polyp and adenoma detection: a prospective randomized controlled study (with videos). Gastrointest Endosc 91:415-424.e4. https://doi.org/10.1016/j.gie.2019.08.026
Troya J, Fitting D, Brand M et al (2022) The influence of computer-aided polyp detection systems on reaction time for polyp detection and eye gaze. Endoscopy. https://doi.org/10.1055/a-1770-7353
Kaminski MF, Thomas-Gibson S, Bugajski M et al (2017) Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy 49:378–397. https://doi.org/10.1055/s-0043-103411
Gong D, Wu L, Zhang J et al (2020) Detection of colorectal adenomas with a real-time computer-aided system (ENDOANGEL): a randomised controlled study. Lancet Gastroenterol Hepatol 5:352–361. https://doi.org/10.1016/S2468-1253(19)30413-3
Urban G, Tripathi P, Alkayali T et al (2018) Deep learning localizes and identifies polyps in real time with 96% accuracy in screening colonoscopy. Gastroenterology 155:1069-1078.e8. https://doi.org/10.1053/j.gastro.2018.06.037
Hassan C, Wallace MB, Sharma P et al (2020) New artificial intelligence system: first validation study versus experienced endoscopists for colorectal polyp detection. Gut 69:799–800. https://doi.org/10.1136/gutjnl-2019-319914
Pfeifer L, Neufert C, Leppkes M et al (2021) Computer-aided detection of colorectal polyps using a newly generated deep convolutional neural network: from development to first clinical experience. Eur J Gastroenterol Hepatol 33:e662–e669. https://doi.org/10.1097/MEG.0000000000002209
Spadaccini M, Hassan C, Alfarone L et al (2022) Comparing number and relevance of false activations between two artificial intelligence CADe SystEms: the NOISE study. Gastrointest Endosc S0016–5107(21):01945–01953. https://doi.org/10.1016/j.gie.2021.12.031
Bangor A, Kortum P, Miller J (2009) Determining what individual SUS scores mean: Adding an adjective rating scale. J Usability Stud 4:114–123
Acknowledgements
The authors acknowledge the support by Prof. J.F. Riemann, “Stiftung Lebensblicke” the Foundation for early detection of colon cancer.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors AH and WGZ receive public funding from the state government of Baden-Württemberg, Germany (Funding cluster “Forum Gesundheitsstandort Baden-Württemberg”) to research and develop artificial intelligence applications for polyp detection in screening colonoscopy (funding number 5409.0–001.01/15). AM receives funding from the IZKF Würzburg (funding number F-406) and the Bavarian Center for Cancer Research (BZKF) for further implementation and development of artificial intelligence for detection of (pre-) neoplastic lesions.
Author information
Authors and Affiliations
Contributions
AH and TJL: study concept and design. AH, TJL, and ZS: statistical analysis. AK and MB: development of the software and neural network. AH, TJL, and MB: interpretation of results, and drafting of the manuscript. AH, TJL, ZS, JT, AK, DF, BS, WGZ, FP, and AM: acquisition of data and providing study material. All authors: critical revision of the article for important intellectual content and final approval of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lux, T.J., Banck, M., Saßmannshausen, Z. et al. Pilot study of a new freely available computer-aided polyp detection system in clinical practice. Int J Colorectal Dis 37, 1349–1354 (2022). https://doi.org/10.1007/s00384-022-04178-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04178-8